INTRODUCTION
Cavernous hemangiomas of the central nervous system are vascular malformations that can affect any part of the neuraxis. Most of these lesions are found intracranially, with supratentorial sites being most commonly affected while vertebral locations are rare3). Cavernous hemangiomas constitute 5-12% of vascular lesions of the spine and are seen most frequently in the vertebral bodies17). The majority of extradural cavernous hemangiomas represent extension from a vertebral hemangioma into the spinal canal with purely extradural locations only representing 1-2% of spinal hemangiomas7,23). These tumors commonly affect the vertebral bodies and extend into the epidural space27), and are less commonly found within the thoracic cavity20). Here, we report our experience with a case of upper thoracic extradural cavernous hemangioma successfully treated by complete removal through combined approaches by video-assisted thoracoscopy and laminectomy.
CASE REPORT
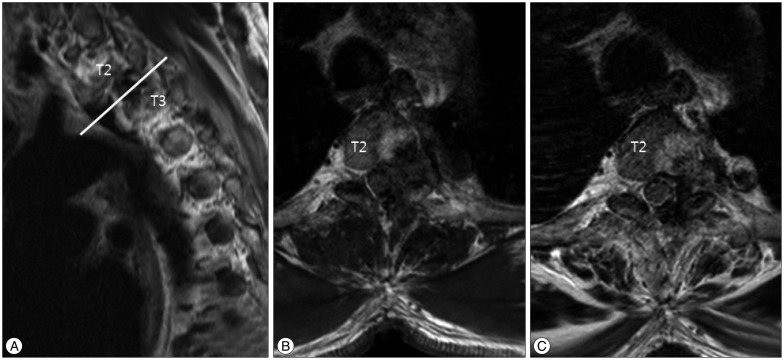
A 64-year-old man was admitted to our hospital with a 6-month history of slowly progressive back pain in the right side infrascapular area. He was otherwise well. Physical examination on admission revealed no focal neurologic deficit. Preoperative magnetic resonance imaging showed a well-demarcated round-shaped abnormal high-signal intensity lesion with mottled low signal intensity on both T1- and T2-weighted sequences within the left half of the T2 vertebral body extending to the left pedicle. An associated left-sided dumbbell-shaped mass at the level of T2-3 was noted and comprised of an extradural mass causing mild cord compression without an intradural portion and extending through the left T2-3 neural foramen to form a 3.0×2.0×2.5-cm intrathoracic mass (Fig. 1). The mass demonstrated isosignal intensity on T1-weighted images (Fig. 1B) and high signal intensity on T2-weighted images (Fig. 1C). There was no contrast-enhanced T1-weighted sequence. The preoperative radiological diagnosis was an extradural dumbbell-shaped schwannoma and concomitant vertebral body hemangioma.
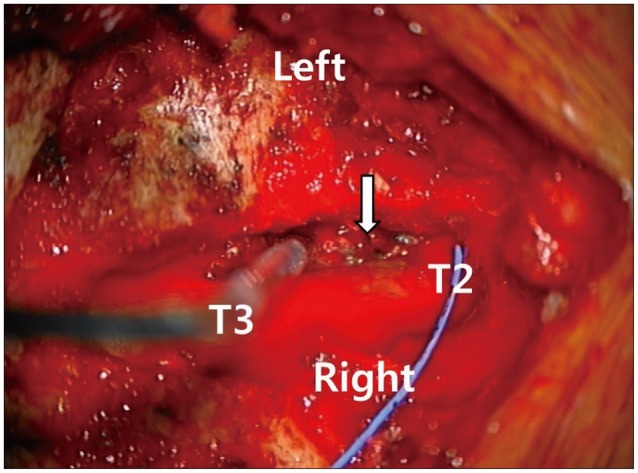
The patient underwent a planned combined posterior and thoracoscopic approach performed by the neurosurgery and cardiothoracic surgery teams, respectively. First, the neurosurgery team performed total laminectomies from T2 to T4. A pinkish, non-encapsulated tumor was found attached to the dura mater and extended through the left T2-3 intervertebral foramen (Fig. 2). Epidural portion of tumor was connected to the tumor of vertebral body portion which mainly involved the cancellous bony part. However, the margin of extradural hemangioma from vertebral body hemangioma was easily separated.
Gross total resection of the tumor was performed by piecemeal method. The left T2 nerve root was sacrificed after resection of the spinal cord-compressing tumor to have cardiothoracic team easily remove the paravertebral mass which was preoperatively diagnosed as an extradural schwannoma. The mass was hypervascular and entirely extradural. After changing the patient's position from prone to lateral, the cardiothoracic surgery team performed a video-assisted thoracoscopic surgery and completely removed the paravertebral mass by piecemeal method. There was no adhesion to the pleura.
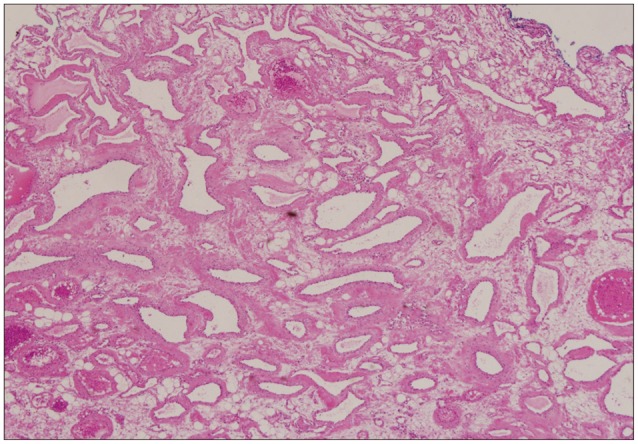
Histopathological diagnosis of the extradural and paravertebral mass was cavernous hemangioma composed of irregular cavernous vascular spaces. The resected specimen contained fibrous connective tissue and many irregular thin-walled vessels filled with blood cells (Fig. 3). The postoperative course of the patient was uneventful. The right infrascapular area back pain was improved, and the patient showed tolerable operative wound pain without symptoms caused by the sacrifice of the left T2 nerve root. Follow-up magnetic resonance imaging performed on the following day after surgery showed no residual extradural cavernous hemangioma (Fig. 4). The patient was discharged on postoperative day 6.
DISCUSSION
Cavernous hemangiomas are benign vascular malformations that can affect any part of the neuraxis4). These masses are composed of packed and dilated sinusoidal vascular spaces lined by a single endothelial layer with no elastic or muscular tissue20). In addition, sinusoidal blood vessels are separated by the hyalinizing stroma with no normal neural connective tissue 3,27). Clinically, patients with spinal cavernous hemagniomas may present with symptoms of spinal cord or nerve root compression. Depending on the location and growth rate, symptoms include local pain, radiculopathy, and slow progressive or acute spinal cord compression8,11). Because these lesions do not grow by mitotic activity, sudden onset of symptoms usually result from trauma, exercise, change in posture, infection, pregnancy, or sprain, all of which may cause hemorrhage or microhemorrhages within the blood vessels and thrombotic occlusion resulting in secondary swelling10,1112,16).
Vertebral hemangioma is extraordinary common, the reported incidences ranged from 10 to 27% in adults. The incidence varies depending on the diagnostic modality used. 10.7% in one large autopsy report, 10-12% in a large population based study using plain X-ray and 27% in a cross sectional study using MRI as the diagnostic tool2).
It has been reported that cavernous hemagnioma developed purely at the spinal epidural space accounts for about 4% or less than that of the other tumors developed at the spinal epidural space and also reported about 1-2% of the cavernous hemangioma developed at the spine3,423,2527). Therefore, most published literatures about epidural cavernous hemangioma had to be case reports1,1213,1820,2224).
These masses can very rarely occur within the organs in the thoracic cavity such as, the anterior mediastinum or the lungs16). Posterior mediastinal cavernous hemangioma may also extend from an extradural spinal cavernous hemangioma through the intervertebral foramen, adopting a 'dumbbell' shape21).
Magnetic resonance imaging can help to differentiate posterior mediastinal cavernous hemangioma from other dumbbell-shaped lesions27), because the location, extent of vertebral hemangioma (intradural or extradural), and presence of neural compression can be visualized. Extradural cavernous hemangiomas show iso- or low-signal intensity on T1-weighted images and high signal intensity in T2-weighted images, with homogeneous or strong enhancement with contrast, although variable enhancement patterns such as slight or peripheral enhancement have also been reported6,723).
The differential diagnosis for paravertebral dumbbell-shaped spinal tumors commonly includes schwannomas, lymphomas, and rarely, meningiomas23). Schwannomas present as an epidural mass with extension to the intervertebral neural foramen; however, a smooth rather than lobulated contour and frequent cystic changes are indicative of this tumor in the differential diagnosis5,7). Lymphomas less frequently extend into the paravertebral or show intervertebral neural foraminal widening. In addition, lymphomas frequently show iso-signal intensity on T2-weighted magnetic resonance imaging14). Meningiomas rarely present with a dumbbell shape or epidural location; however, isosignal intensity of the spinal cord with frequent broad dural attachment can be indications for the differential diagnosis23).
Complete resection is recommended for the treatment for extradural cavernous hemangioma25,27), because incomplete resection of the tumor may lead to recurrence of symptoms27), although malignant transformation of extradural cavernous hemangioma has not been reported26). However, incomplete resection of cavernous hemangiomas often occurs because conventional piecemeal resection may lead to profuse bleeding during the surgery due to its friable, thin-walled vessels25). Laminectomy, either standard or combined with foraminotomy or costo-transversectomy, has also been used to treat these tumors20,27). However, these approaches only provide limited exposure of the posterior mediastinum and lead to incomplete resection in case of the intrathoracic extension of the tumor25). To achieve complete resection, sufficient exposure of both lesions is needed. Therefore, intrathoracic extraforaminal extension of an extradural cavernous hemangioma, including the other dumbbell-shaped tumors could be surgically treated through the combination of posterior laminectomy followed by thoracoscopic resection, because this approach maximizes visibility of the lesion, controls possible residual lesions, and minimizes operation time21). After incomplete resection, subsequent surgery can be performed on the residual lesion if symptoms recur. Radiation therapy may be indicated in cases of asymptomatic growth or persistent pain. However, the role of radiation therapy still remain controversial20,2527).
CONCLUSION
Cavernous hemangiomas should be considered in the differential diagnoses of paravertebral dumbbell-shaped spinal tumors and should be treated by complete resection using combined approaches of posterior laminectomy for resection of extradural part and video-assisted thoracoscopic removal of intrathoracic one.