Kim, Kim, Kim, Hwang, Jin, Lenke, and Cha: Outcomes of Non-Operative Management for Pseudarthrosis after Pedicle Subtraction Osteotomies at Minimum 5 Years Follow-Up
Abstract
Objective
Minimal data exist regarding non-operative management of suspected pseudarthrosis after pedicle subtraction osteotomy (PSO). This study reports radiographic and clinical outcomes of non-operative management for post-PSO pseudarthrosis at a minimum 5 years post-detection.
Methods
Nineteen consecutive patients with implant breakage indicating probable pseudarthrosis after PSO surgery (13 women/ six men; mean age at surgery, 58 years) without severe pain and disability were treated with non-operative management (mean follow-up, 5.8 years; range, 5-10 years). Non-operative management included medication, intermittent brace wearing and avoidance of excessive back strain. Radiographic and clinical outcomes analysis was performed.
Results
Sagittal vertical axis (SVA), proximal junctional angle, thoracic kyphosis achieved by a PSO were maintained after detection of pseudarthrosis through ultimate follow-up. Lumbar lordosis and PSO angle decreased at final follow-up. There was no significant change in Oswestry Disability Index (ODI) scores and Scoliosis Research Society (SRS) total score, or subscales of pain, self-image, function, satisfaction and mental health between detection of pseudarthrosis and ultimate follow-up. SVA greater than 11 cm showed poorer ODI and SRS total score, as well as the pain, self-image, and function subscales (p<0.05).
Conclusion
Non-operative management of implant failure of probable pseudarthrosis after PSO offers acceptable outcomes even at 5 years after detection of implant breakage, provided SVA is maintained. As SVA increased, outcome scores decreased in this patient population.
Key Words: Spine · Joint deformities, Acquired · Osteotomy · Pseudarthrosis · Conservative management.
INTRODUCTION
Pedicle subtraction osteotomy (PSO) may be necessary to achieve correction of spinal deformity in cases with severe, rigid curves and may be employed to help restore both coronal and sagittal spinopelvic alignment [ 10]. Although PSO procedures are associated with greater correction of adult spinal deformity, these procedure are associated with significant risk, with complications described in 21% to 34% of patients [ 6, 13, 17, 23- 25]. Pseudarthrosis is one of the most common complications and also one of the most common indications for revision surgery after PSO [ 1- 3, 6, 18, 19]. Kim et al. [ 15] reported that the rate of pseudarthrosis after PSO was surprisingly high at 29%. However, not all of these pseudarthrosis patients have severe clinical discomforts meriting revision surgery [ 6, 14, 21, 22]. Therefore, it is often difficult to predict which patients are likely to improve clinically and which will be functionally more compromised over time after detection of pseudarthrosis. Several studies have previously demonstrated that revision rates after PSO range from 12% to 23% [ 1, 3, 7, 12, 15, 18, 19]. Most studies on PSO outcomes have typically reported revision rates up to 2 years of follow-up. Revision procedures for non-mechanical complications such as neurologic deficit, infection, and wound dehiscence typically occur within the first year after index surgery. However, revision surgery for mechanical complication such as pseudarthrosis, implant failure, junctional failure, and loss/lack of correction have been reported to occur between 2 years and 5 years as well, beyond the reported follow-up of most PSO studies [ 14]. To the best of our knowledge, there are no published reports on the results of non-operative management for pseudarthrosis after PSO with long-term follow-up. The specific aim of this study was to report radiographic and clinical outcomes at a minimum of 5 years after detection for non-operative management and to analyze the characteristics of probable pseudarthrosis after PSO.
MATERIALS AND METHODS
Patient population
After Institutional Review Board approval (Ulsan University Hospital 2018-09-016), a retrospective radiographic and clinical analysis was conducted of patients who had undergone PSO for spinal deformity between 1999 and 2009. Data was collected and analyzed by an independent senior spine surgeon not involved in the surgical treatment. Of 335 patients who underwent PSO, pseudarthrosis was found in 32 patients (9.6%). Non-operative management was initially attempted in patients with pseudarthrosis. Revision surgery was done in nine patients : five cases were due to patient’s severe pain and four cases were due to severe deformity. Twenty-three patients who had non-operative management (observation, medication, avoidance of excessive back strain, and intermittent brace wearing) for pseudarthrosis as a complication after a PSO were identified. However, four patients were lost to follow-up before the 5-year follow-up period. Nineteen patients had complete medical records, including preoperative and postoperative radiographic data, operative data, hospital data, and a minimum 5-year follow-up. Demographic data and complications were recorded. Radiographs and patient-reported outcome questionnaires were done prospectively and then data that had been collected was reviewed retrospectively.
Radiographic measurements
Standing 36-inch long cassette anteroposterior (AP) and lateral radiographs of the spine were measured preoperatively, immediate postoperatively, and at ultimate follow-up with a minimum 5-year. All radiographic measurements were performed by one author, an attending spine surgeon who was not part of the surgical team.
Radiographic criteria used to define pseudarthrosis were as follows : 1) loss of fixation, such as implant breakage, dislodgment of rods or hooks, or a lucent halo around a pedicle screw; 2) lack of bridging bone across motion segments on computed tomography; 3) subsequent disc space collapse at the distally instrumented motion segment compared with the findings at the first postoperative visit; 4) any motion on side bending or flexion/extension plain radiographs; and 5) progression of the deformity clinically or radiographically [ 14]. Proximal junctional angle (PJA) was defined using the caudal endplate of the upper instrumented vertebra (UIV) and the cephalad endplate of the vertebra 2 segments proximal to the UIV (UIV+2) and pedicle subtraction osteotomy angle (PSOA) was defined as the angle between the caudal endplate of 1 supra-adjacent vertebra above the osteotomy site and the caudal endplate of 1 infra-adjacent vertebra below the osteotomy site. The Cobb method was used to measure thoracic kyphosis (TK : T5-T12), thoracolumbar kyphosis (TLK : T10- L2), and lumbar lordosis (LL : T12-S1) [ 5]. Standard spinopelvic parameters were recorded, as was sagittal vertical axis (SVA).
Patient-reported outcomes
All clinical questionnaires were collected prospectively. Oswestry Disability Index (ODI) [ 8] and Scoliosis Research Society-30 (SRS) [ 11] patient-reported outcomes were collected preoperatively and at each follow-up visit. Total SRS scores were converted to a 100-point scale. In addition, pain, self-image, function, satisfaction, and mental health domain scores were evaluated.
Statistical analysis
Data were analyzed using SPSS ver. 10.0 software (SPSS Inc., Chicago, IL, USA). Statistical analysis included descriptive statistics, means, standard deviation, and ranges. For most variables for which data were collected before and after surgery, paired t tests were used to determine whether there was a significant change between time points. The Mann-Whitney U test was used to assess the difference of continuous measures across groups. A p value <0.05 was considered significant.
RESULTS
Patient data
Patient demographics information including age at time of surgery, sex, mean follow-up period from defection of pseudarthrosis, and pre-PSO diagnosis is presented in Table 1.
Surgical procedure (PSO)
Pedicle screws were placed at the upper instrumented vertebrae for all but one patient (hook). The LIV was S1 including the ilium in 16 patients (84.2%). The number of rods used in the PSO surgery were two in all except two patients (three rods) and the rod size was 5.5 mm stainless steel in diameter in all but three patients (6.35 mm stainless steel). Bone morphogenetic protein was used in 10 patients ( Table 2).
Characteristics of probable pseudarthrosis
Radiographic characteristics of pseudarthrosis including level of PSO, radiographic findings, site of pseudarthrosis and detection time of pseudarthrosis are presented in Table 1. In terms of the numbers of broken rods, most of patients (13 of 16 patients with rod breakage) were unilateral, but three patients had bilateral rod breakage. All three patients with bilateral rod breakage had pseudarthrosis at the non-PSO site (lumbobsacral junction) in which anterior spinal fusion at L5-S1 was performed ( Fig. 1). The non-PSO site included the lumbosacral junction (9/19) and thoracolumbar junction (6/19). The two disks space collapse occurred at the L5-S1 in which anterior spinal fusion was not performed, and all 3 pedicle screw pull-outs occurred at the UIV (1 in L1 and 2 in T11). Interestingly, all four of the patients with pseudarthrosis at the PSO site had an interbody device placed at either the PSO segment or the adjacent segment ( Fig. 2).
Time-dependent radiographic changes
Time-dependent radiographic changes including SVA, PJA, TK, TLK, LL, PSOA, and pelvic incidence (PI) are presented in Table 3. Mean SVA, TK, LL, and PSOA were significantly different between preoperative and 2 months post-surgery ( p<0.05). All of the radiographic changes were not significantly different between value at detection of pseuarthrosis and value at 1 year and 5 years after detection ( p>0.05).
Time-dependent clinical outcome changes
Time-dependent clinical outcomes changes are presented in Table 4. Both the ODI and SRS questionnaire scores improved significantly when comparing preop to ultimate follow-up scores. All scores worsened at detection of the pseudarthrosis but did not progressively worsen between detection and ultimate follow-up. There was no significant change in ODI scores and SRS total score, or subscales of pain, self-image, function, satisfaction, and mental health between detection of pseudarthrosis and ultimate follow-up ( p>0.05).
Comparison of clinical outcomes according to PI and SVA
We further evaluated the difference in outcomes by dividing the patients into two groups : group I, PI ≤60° and group II, PI >60° ( Table 5). At ultimate follow-up, the mean ODI and total SRS scores were worse in group II vs. group I, respectively. All SRS subscales were also worse in the group II patients but none of these differences were statistically significant. In addition, there were significant differences between the patients with SVA ≤11 cm and >11 cm in ODI scores, SRS total, SRS pain subscores, SRS self-image subscores, and SRS function subscores at ultimate follow-up ( p<0.05) ( Table 5).
DISCUSSION
In order to prevent complications after PSO, perfect correction is important. All of the cases in this journal have undergone primary PSO for “spinopelvic harmony” (SVA <5 cm, PT <20 degrees, and LL=PI±9 degrees), but pseudoarthrosis following POS has occurred [ 20]. SVA, PJA, and TK achieved by a PSO were maintained after detection of pseudarthrosis through ultimate follow-up, but were not preserved from the correction obtained immediately post-surgery. LL ( p=0.042) and PSO angle ( p=0.044) decreased at final follow-up, although this decrease was not significant ( Table 3). We postulate that LL and PSOA decreased at final follow-up due to the fact that most pseudarthrosis events occurred at either the L5-S1 segment (nine in 19 patients, 47.4%) or the PSO site (four in 19 patients, 21.1%). We previously reported on successful radiographic and improved clinical outcomes after revision surgery for pseudarthrosis following PSO [ 14]. In the current study, the ODI and all SRS subscores improved by PSO did not change significantly at ultimate follow-up. On the other hand, our previous report, regarding the SRS questionnaire, there was only significant improvement of the pain subscale after revision surgery and the self-image subscale was unchanged and the mental health subscale decreased after revision surgery for pseudarthrosis. We believe this might be due to different patient population. Most of the patients in the current study had not experienced prior surgeries and did not have many comorbidities which adversely affected the scores in contrast with the patients included in the previous study [ 14]. Interestingly, despite the loss by ultimate follow-up of LL and PSOA corrections initially achieved via PSO, ODI and SRS scores generally did not worsen after the time of initial pseudarthrosis detection. We think this might be due to maintenance of SVA achieved by PSO through ultimate follow-up. Glassman et al. [ 9] reported that sagittal balance using C7 SVA is the most important and reliable radiographic predictor of clinical health status, as patients with positive sagittal imbalance reported worse self-assessment in SRS 22 pain, function, and self-image subscores. ODI and all SRS subscores of the patients with a PI >60° demonstrated a trend toward poorer than in patients with a PI ≤60°, but the differences were not significant. This reinforces that patients with a high PI also need a high degree of correction of sagittal balance which could not be achieved by a single PSO [ 4, 15, 16]. This correction deficit may lead to higher strain forces on the instrumentation with an unbalanced equilibrium, in turn triggering a non-union or implant failure [ 16]. There are several limitations to this study. First, as a retrospective review. Second, our study did not analyze comparison between post-PSO pseudarthrosis patients who did undergo revision surgery vs. those who chose non-operative treatment. In addition, this study only evaluated patients who had a minimum 5 years follow-up. It is unclear whether a higher follow-up rate would impact our findings. We acknowledge the limitation of diagnosing pseudarthrosis based on radiographs alone. In other words, there may be a likelihood of possible pseudarthrosis which does not require revision surgery and they are usually discovered in a purely incidental fashion through follow-up without apparent symptoms related to definite pseudarthrosis. Most of patients in this current study had modest, but satisfactory improvement in symptoms with non-operative management and declined revision surgery.
We believe that non-operative management for probable pseudarthrosis following PSO can provide acceptable radiographic and clinical outcomes at a minimum 5 years after detection of pseudarthrosis, particularly in patients with a PI <60 degrees.
CONCLUSION
Non-operative management of possible pseudarthrosis after PSO offers acceptable outcomes even at 5 years after detection of pseudarthrosis, provided SVA is maintained. Based on this, it is considered better to try to conservative treatment for pseudarthrosis after POS, provided SVA is maintained. As SVA increased, clinical outcome scores decreased. Patients with a PI <60 degrees typically fared better at final follow-up.
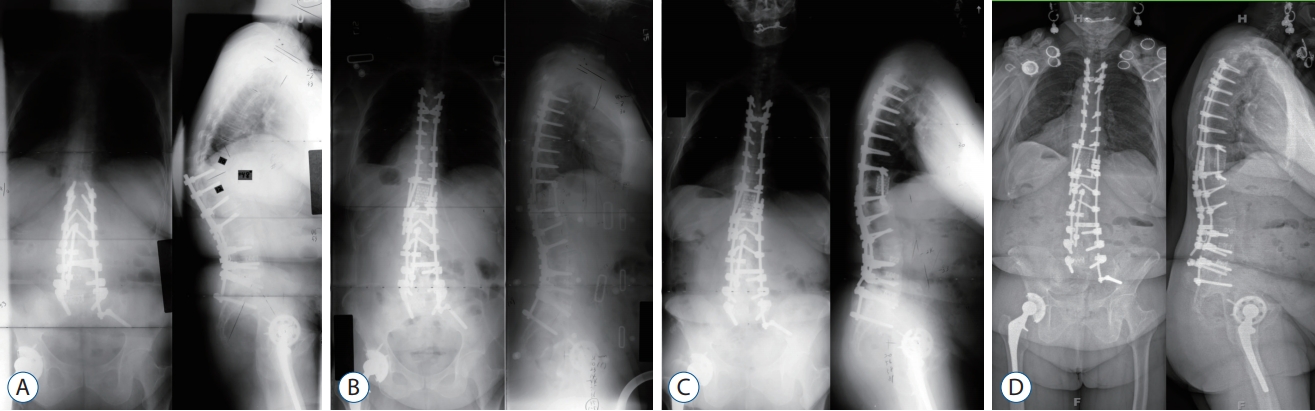
Fig. 1.
A 70-year-old female had sagittal imbalance due to proximal junctional kyphosis occurring after pedicle subtraction osteotomy. A : Standing AP and lateral radiographs at 1 year after pedicle subtraction osteotomy. B : Standing AP and lateral radiographs at 2 months after three column osteotomy. C : Standing AP and lateral radiographs at 4 years after three column osteotomy presents bilateral rod breakage at lumbosacral junction in which anterior spinal fusion in L5-S1 was performed. D : Standing AP and lateral radiographs at 6 years after detection of pseudarthrosis. AP : anteroposterior. 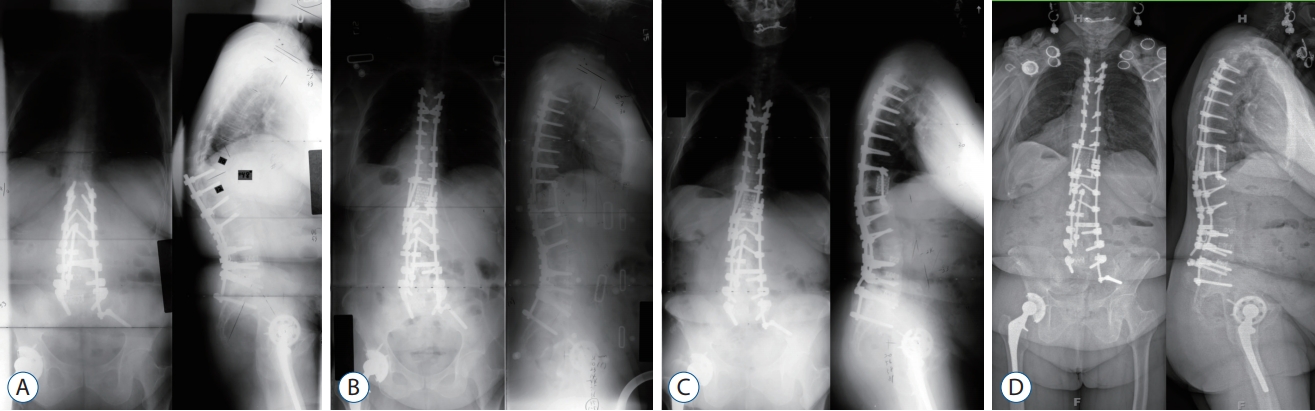
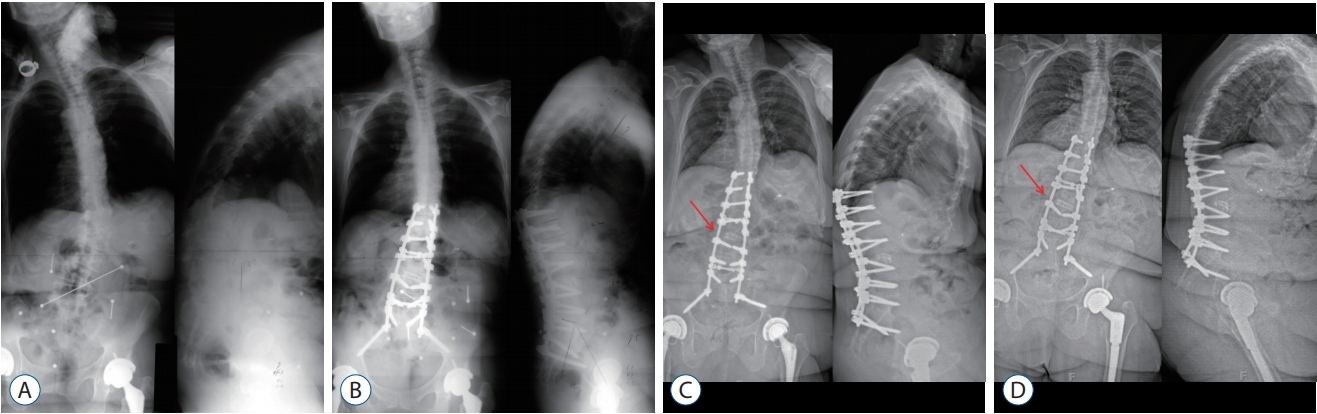
Fig. 2.
A 72-year-old female had sagittal imbalance due to degenerative lumbar kyphoscoliosis. A : Standing AP and lateral radiograph before pedicle subtraction osteotomy. B : Standing AP and lateral radiographs at 2 months after pedicle subtraction osteotomy on L3. C : Standing AP and lateral radiographs at 2 years after pedicle subtraction osteotomy presents right rod breakage at pedicle subtraction osteotomy site. The arrow indicating the broken portion of the rod. D : Standing AP and lateral radiographs at 5 years after detection of pseudarthrosis. The arrow indicating the broken portion of the rod. AP : anteroposterior. 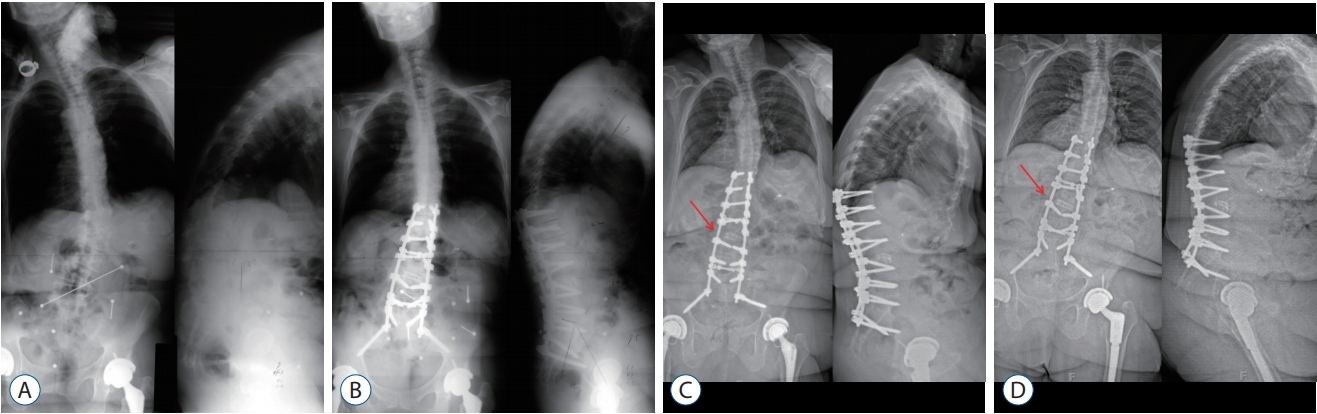
Table 1.
|
Value |
|
Gender |
13 women; 6 men |
|
Age at operation (years) |
58.0±9.9 (39.5-69.0) |
|
BMI (kg/m2) |
26.4±6.1 (20.4-46.0) |
|
Total follow-up (years) |
8.5±2.3 (6.0-12.6) |
|
Detection of pseudarthrosis to ultimate F/U (years) |
5.8 ±1.3 (5-10) |
|
Initial diagnosis |
8 degenerative lumbar kyphoscoliosis |
|
7 adult idiopathic scoliosis |
|
3 postoperative state of Idiopathic scoliosis |
|
1 postoperative state of burst fracture |
|
Level of PSO |
4 at L2, 12 at L3, 3 at L4 |
|
No. of fused vertebrae |
10.6±3.6 (5-16) |
|
Comorbidity |
5 patients (0 smokers; 6 comorbidities) |
|
Common radiographic findings |
Rod breakage (n=16, 84.2%; 13 in unilateral; 3 in bilateral) |
|
Disc space collapse (n=2, 10.5%) |
|
Pedicle screw pull-out (n=3, 15.8%; 2 in unilateral; 1 in bilateral) |
|
Halo sign around pedicle screw (n=1, 5.3%) |
|
Site of pseudarthrosis |
4 patients (21.2%) at PSO |
|
15 patients (78.8%) at non-PSO |
|
Detection time of pseudarthrosis (months) |
32.8±23.2 (range, 12-91) |
|
52.5±35 (range, 19-91) in pseudarthrosis at PSO site |
|
27.6±17.1 (range, 12-61) in pseudarthrosis at non-PSO site |
Table 2.
Surgical procedure of pedicle subtraction osteotomy
|
PSO level |
Pseudarthrosis site |
Radiographic finding |
ASF |
UIL |
LIL |
No. of rod |
Size of rod (mm) |
BMP (mg) |
|
1 |
L2 |
L2-3 |
Right rod fracture |
L3-4 |
T3 (S) |
Ilium |
2 |
5.5 |
0 |
|
2 |
L4 |
L5-S1 |
Right rod fracture |
L3-4-5 |
T5 (S) |
Ilium |
2 |
5.5 |
302 |
|
3 |
L3 |
L5-S1 |
Both rod fracture |
L5-S1 |
T10 (S) |
Ilium |
2 |
5.5 |
0 |
|
4 |
L3 |
L4-5 |
Left rod fracture |
L5-S1 |
T9 (S). |
Ilium |
2 |
6.5 |
0 |
|
5 |
L3 |
L1-2 |
Screw pull out |
|
L1 (S) |
S1 (S) |
2 |
5.5 |
0 |
|
6 |
L2 |
L5-S1 |
Disc space collapse, halo sign |
|
T11 (S) |
S1 (S) |
2 |
5.5 |
36 |
|
7 |
L3 (picture) |
L5-S1, T11-12 |
both rod fracture, screw pull out |
L3-4-5-S1 |
T11 (S) |
Ilium |
2 |
5.5 |
72 |
|
8 |
L3 |
L5-S1 |
Left rod fracture |
L5-S1 |
T4 (S) |
Ilium |
2 |
6.5 |
12 |
|
9 |
L2 |
L2-3 |
Right rod fracture |
L3-4 |
T4 (S) |
Ilium |
3 |
5.5 |
24 |
|
10 |
L2 |
T10-11 |
Right rod fracture |
L5-S1 |
T5 (H) |
Ilium |
2 |
5.5 |
0 |
|
11 |
L3 |
T12-L1 |
Left rod fracture |
L5-S1 |
T12 (S) |
Ilium |
2 |
5.5 |
0 |
|
12 |
L4 |
T10-11 |
Left rod fracture |
|
T3 (S) |
Ilium |
2 |
6.5 |
0 |
|
13 |
L3 |
L5-S1 |
Both rod fracture |
L3-4-5-S1 |
T4 (S) |
Ilium |
3 |
5.5 |
0 |
|
14 |
L3 |
L3-4 |
Right rod fracture |
L4-5 |
T9 (S) |
S1 (S) |
2 |
5.5 |
0 |
|
15 |
L3 |
T12-L1 |
Left rod fracture |
|
T10 (S) |
Ilium |
2 |
5.5 |
25 |
|
16 |
L3 |
L5-S1 and T10-11 |
Left rod fracture |
L5-S1 |
T11 (S) |
Ilium |
2 |
5.5 |
24 |
|
17 |
L3 |
L5-S1 |
Right rod fracture |
L5-S1 |
T12 (S) |
Ilium |
2 |
5.5 |
48 |
|
18 |
L4 |
T11-12, L5-S1 |
Screw pull out, disc space collapse |
|
T11 (S) |
Ilium |
2 |
5.5 |
132 |
|
19 |
L3 |
L3-4 |
Left rod fracture |
L3-4 |
T11 (S) |
Ilium |
2 |
5.5 |
72 |
Table 3.
Time-dependent radiotraphic change
|
Preop |
PO #2 M |
Detection of PS |
#1 Y after detection |
#5 Y after detection |
|
SVA (cm) |
16.9±7.4 |
2.9±5.6 |
8.5±5.8 |
9.0±6.2 |
8.9±5.8 |
|
P* (preop vs. PO) |
|
P.000 |
P.000 |
P.000 |
P.000 |
|
P* (PS vs. #1 Y/#5 Y) |
|
|
|
P.544 |
P.608 |
|
PJA (°) |
9.2±12.0 |
11.5±11.2 |
12.6±10.1 |
13.7±10.4 |
13.6±9.7 |
|
P* (preop vs. PO) |
|
P.160 |
P.162 |
P.080 |
P.082 |
|
P* (PS vs. #1 Y/#5 Y) |
|
|
|
P.379 |
P.388 |
|
TK (°) |
16.9±19.2 |
27.5±14.7 |
29.1±14.1 |
19.2±17.3 |
28.6±16.9 |
|
P* (preop vs. PO) |
|
P.001 |
P.000 |
P.003 |
P.03 |
|
P* (PS vs. #1 Y/#5 Y) |
|
|
|
P.928 |
P.771 |
|
TLK (°) |
18.2±25.7 |
8.5±17.3 |
8.3±20.9 |
9.7±20.9 |
9.9±20.0 |
|
P* (preop vs. PO) |
|
P.098 |
P.111 |
P.176 |
P.175 |
|
P* (PS vs. #1 Y/#5 Y) |
|
|
|
P.216 |
P.177 |
|
LL (°) |
-4.0±17.1 |
-43.5±15.9 |
-35.8±14.4 |
-33.6±16.1 |
-33.8±15.4 |
|
P* (preop vs. PO) |
|
P.000 |
P.000 |
P.000 |
P.000 |
|
P* (PS vs. #1 Y/#5 Y) |
|
|
|
P.051 |
P.042 |
|
PSOA (°) |
14.9±17.0 |
-19.9±13.9 |
-18.1±15.9 |
-14.2±18.9 |
-13.4±18.7 |
|
P* (preop vs. PO) |
|
P.000 |
P.000 |
P.000 |
P.000 |
|
P* (PS vs. #1 Y/#5 Y) |
|
|
|
P.089 |
P.044 |
|
PI (°) |
49.4±13.5 |
52.8±10.4 |
54.1±11.2 |
54.9±11.1 |
53.4±11.0 |
|
P* (preop vs. PO) |
|
P.102 |
P.003 |
P.006 |
P.014 |
|
P* (PS vs. #1 Y/#5 Y) |
|
|
|
P.365 |
P.303 |
Table 4.
Time-dependent clinical change
|
Preop |
PO #2 M |
Detection of PS |
#1 Y after detection |
#5 Y after detection |
|
ODI (100) |
56.9±14.2 |
34.5±14.0 |
36±13.6 |
43.1±18.1 |
40.3±16.7 |
|
P* (preop vs. PO) |
|
P.000 |
P.000 |
P.109 |
P.002 |
|
P* (PS vs. #1 Y/#5 Y) |
|
|
|
P.106 |
P.103 |
|
SRS total score (100%) |
47.2±14.1 |
70.8±12.9 |
67.4±13.6 |
65.2±14.0 |
62.9±13.9 |
|
P* (preop vs. PO) |
|
P.000 |
P.000 |
P.000 |
P.000 |
|
P* (PS vs. #1 Y/#5 Y) |
|
|
|
P.172 |
P.104 |
|
SRS pain (5) |
2.2±0.8 |
3.2±1.03 |
2.9±0.9 |
2.8±0.9 |
2.7±0.8 |
|
P* (preop vs. PO) |
|
P.000 |
P.002 |
P.015 |
P.041 |
|
P* (PS vs. #1 Y/#5 Y) |
|
|
|
P.165 |
P.061 |
|
SRS self image (5) |
2.1±0.8 |
3.5±0.7 |
3.3±0.9 |
3.0±0.8 |
30.0±0.7 |
|
P* (preop vs. PO) |
|
P.000 |
P.000 |
P.002 |
P.002 |
|
P* (PS vs. #1 Y/#5 Y) |
|
|
|
P.047 |
P.102 |
|
SRS function (5) |
2.2±0.8 |
3.1±0.7 |
3.0±0.8 |
2.8±0.9 |
2.8±0.9 |
|
P* (preop vs. PO) |
|
P.010 |
P.000 |
P.011 |
P.011 |
|
P* (PS vs. #1 Y/#5 Y) |
|
|
|
P.053 |
P.053 |
|
SRS satisfaction (5) |
2.4±0.9 |
4.0±0.9 |
3.9±1.1 |
3.8±1.0 |
3.8±1.0 |
|
P* (preop vs. PO) |
|
P.000 |
P.002 |
P.003 |
P.003 |
|
P* (PS vs. #1 Y/#5 Y) |
|
|
|
P.604 |
P.604 |
|
SRS mental health (5) |
2.9±0.9 |
3.9±0.8 |
3.7±0.8 |
3.9±0.6 |
3.6±0.5 |
|
P* (preop vs. PO) |
|
P0.002 |
P.003 |
P.001 |
P.006 |
|
P* (PS vs. #1 Y/#5 Y) |
|
|
|
P.272 |
P.272 |
Table 5.
Comparison of clinical outcomes according to PI and SVA
|
PI ≤60 |
PI >60 |
p-value*
|
SVA ≤11 cm |
SVA >11 cm |
p-value*
|
|
ODI (100) |
|
|
|
|
|
|
|
Preop |
57.6±14.5 |
55.5±14.7 |
0.773 |
52.0±13.1 |
59.2±14.6 |
0.318 |
|
PO #2 M |
33.6±14.3 |
42.8±12.0 |
0.192 |
29.36±14.5 |
39.8±13.0 |
0.133 |
|
Detection of PS |
33.1±10.0 |
45.0±17.8 |
0.079 |
30.0±10.2 |
40.0±14.2 |
0.140 |
|
#1 Y after detection |
39.4±18.0 |
51.0±16.9 |
0.205 |
30.54±13.5 |
48.9±17.3 |
0.035 |
|
#5 Y after detection |
36.7±15.7 |
48.0±17.5 |
0.180 |
28.3±11.9 |
45.8±15.9 |
0.029 |
|
SRS total score (100%) |
|
|
|
|
|
|
|
Preop |
47.8±13.7 |
49.2±16.3 |
0.853 |
54.8±17.6 |
45.3±11.8 |
0.179 |
|
PO #2 M |
66.8±13.9 |
64.5±11.8 |
0.727 |
73.4±17.1 |
62.7±9.5 |
0.096 |
|
Detection of PS |
68.8±13.8 |
64.5±13.9 |
0.537 |
79.7±8.8 |
61.7±11.7 |
0.004 |
|
#1 Y after detection |
67.7±12.9 |
58.9±15.7 |
0.215 |
74.5±14.7 |
60.5±11.8 |
0.041 |
|
#5 Y after detection |
65.1±12.9 |
58.1±16.1 |
0.321 |
73.9±12.6 |
57.8±11.7 |
0.015 |
|
SRS pain (5) |
|
|
|
|
|
|
|
Preop |
2.2±.8 |
2.1±0.9 |
0.759 |
2.6±0.8 |
2.0±0.8 |
0.182 |
|
PO #2 M |
3.4±1.1 |
2.8±0.7 |
0.207 |
3.5±1.3 |
3.1±0.8 |
0.464 |
|
Detection of PS |
3.2±0.9 |
2.4±0.7 |
0.081 |
3.6±0.8 |
2.6±0.8 |
0.042 |
|
#1 Y after detection |
3.0±0.9 |
2.3±0.8 |
0.106 |
3.3±1.0 |
2.5±0.8 |
0.092 |
|
#5 Y after detection |
2.8±0.8 |
2.2±0.8 |
0.142 |
3.2±0.9 |
2.4±0.7 |
0.040 |
|
SRS self image (5) |
|
|
|
|
|
|
|
Preop |
2.0 ±0.8 |
2.0±0.8 |
0.970 |
2.4±0.9 |
1.9±0.7 |
0.207 |
|
PO #2 M |
3.2±0.7 |
3.2±0.7 |
0.969 |
3.6±0.9 |
3.0±0.5 |
0.085 |
|
Detection of PS |
3.3±0.8 |
3.2±1.1 |
0.314 |
4.1±0.3 |
2.8±0.7 |
0.001 |
|
#1 Y after detection |
3.1±0.7 |
2.7±0.9 |
0.646 |
3.5±0.4 |
2.7±0.8 |
0.037 |
|
#5 Y after detection |
3.0±0.7 |
2.7±0.8 |
0.592 |
3.5±0.4 |
2.7±0.7 |
0.034 |
|
SRS function (5) |
|
|
|
|
|
|
|
Preop |
2.2±0.7 |
2.3±0.9 |
0.748 |
2.8±0.7 |
1.9±0.6 |
0.021 |
|
PO #2 M |
2.96±0.7 |
2.6±0.6 |
0.154 |
3.1±0.7 |
2.7±0.7 |
0.249 |
|
Detection of PS |
3.0±0.8 |
2.8±0.9 |
0.933 |
3.6±0.4 |
2.6±0.7 |
0.019 |
|
#1 Y after detection |
2.8±0.9 |
2.5±0.8 |
0.586 |
3.4±0.7 |
2.4±0.9 |
0.040 |
|
#5 Y after detection |
2.8±0.9 |
2.5±0.8 |
0.586 |
3.4±0.7 |
2.4±0.9 |
0.040 |
|
SRS satisfaction (5) |
|
|
|
|
|
|
|
Preop |
2.3±0.8 |
2.7±1.2 |
0.400 |
2.9±1.2 |
2.1±0.8 |
0.111 |
|
PO #2 M |
4.0±0.6 |
3.6±1.5 |
0.453 |
4.3±0.4 |
3.7±1.1 |
0.178 |
|
Detection of PS |
3.7±1.2 |
4.1±0.7 |
0.552 |
4.3±0.6 |
3.6±1.2 |
0.268 |
|
#1 Y after detection |
3.8±0.9 |
3.5±1.1 |
0.481 |
4.0±1.3 |
3.6±0.8 |
0.354 |
|
#5 Y after detection |
3.8±0.9 |
3.5±1.1 |
0.481 |
4.0±1.3 |
3.6±0.8 |
0.354 |
|
SRS mental health (5) |
|
|
|
|
|
|
|
Preop |
2.8±0.9 |
2.9±0.9 |
0.974 |
2.8±0.9 |
2.9±0.9 |
0.943 |
|
PO #2 M |
3.3±0.7 |
3.4±1.0 |
0.786 |
3.9±0.6 |
3.1±0.7 |
0.058 |
|
Detection of PS |
3.6±0.8 |
3.9±0.6 |
0.401 |
4.2±0.4 |
3.4±0.7 |
0.034 |
|
#1 Y after detection |
3.9±0.6 |
3.7±0.5 |
0.458 |
4.1±0.6 |
3.7±0.6 |
0.212 |
|
#5 Y after detection |
3.6±0.5 |
3.3±0.2 |
0.269 |
3.5±0.4 |
3.5±0.5 |
0.968 |
References
1. Auerbach JD, Lenke LG, Bridwell KH, Sehn JK, Milby AH, Bumpass D, et al : Major complications and comparison between 3-column osteotomy techniques in 105 consecutive spinal deformity procedures. Spine (Phila Pa 1976) 37 : 1198-1210, 2012   2. Bridwell KH, Lewis SJ, Edwards C, Lenke LG, Iffrig TM, Berra A, et al : Complications and outcomes of pedicle subtraction osteotomies for fixed sagittal imbalance. Spine (Phila Pa 1976) 28 : 2093-2101, 2003   3. Bridwell KH, Lewis SJ, Lenke LG, Baldus C, Blanke K, et al : Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. J Bone Joint Surg Am 85-A : 454-463, 2003  4. Bridwell KH, Lewis SJ, Rinella A, Lenke LG, Baldus C, Blanke K : Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. Surgical technique. J Bone Joint Surg Am 86 : 44-50, 2004   5. Cobb JR : Outline for the study of scoliosis. In: instructional course lectures, J Am Acad Orthop Surg 261-275, 1948
6. Dickson DD, Lenke LG, Bridwell KH, Koester LA : Risk factors for and assessment of symptomatic pseudarthrosis after lumbar pedicle subtraction osteotomy in adult spinal deformity. Spine (Phila Pa 1976) 39 : 1190-1195, 2014   7. Dvorak MF, Kwon BK, Fisher CG, Eiserloh HL 3rd, Boyd M, Wing PC : Effectiveness of titanium mesh cylindrical cages in anterior column reconstruction after thoracic and lumbar vertebral body resection. Spine (Phila Pa 1976) 28 : 902-908, 2003   8. Fairbank JC, Pynsent PB : The oswestry disability index. Spine (Phila Pa 1976) 25 : 2940-2952; discussion 2952, 2000   9. Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F : The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 30 : 2024-2029, 2005   10. Gupta MC, Kebaish K, Blondel B, Klineberg E : Spinal osteotomies for rigid deformities. Neurosurg Clin N Am 24 : 203-211, 2013   11. Haher TR, Gorup JM, Shin TM, Homel P, Merola AA, Grogan DP, et al : Results of the scoliosis research society instrument for evaluation of surgical outcome in adolescent idiopathic scoliosis. A multicenter study of 244 patients. Spine (Phila Pa 1976) 24 : 1435-1440, 1999   12. Hassanzadeh H, Jain A, El Dafrawy MH, Ain MC, Mesfin A, Skolasky RL, et al : Three-column osteotomies in the treatment of spinal deformity in adult patients 60 years old and older: outcome and complications. Spine (Phila Pa 1976) 38 : 726-731, 2013   13. Helenius I, Serlo J, Pajulo O : The incidence and outcomes of vertebral column resection in paediatric patients: a population-based, multicentre, follow-up study. J Bone Joint Surg Br 94 : 950-955, 2012   14. Kim YC, Lenke LG, Hyun SJ, Lee JH, Koester LA, Blanke KM : Results of revision surgery after pedicle subtraction osteotomy for fixed sagittal imbalance with pseudarthrosis at the prior osteotomy site or elsewhere: minimum 5 years post-revision. Spine (Phila Pa 1976) 39 : 1817-1828, 2014   15. Kim YJ, Bridwell KH, Lenke LG, Cheh G, Baldus C : Results of lumbar pedicle subtraction osteotomies for fixed sagittal imbalance: a minimum 5-year follow-up study. Spine (Phila Pa 1976) 32 : 2189-2197, 2007   16. Le Huec JC, Cogniet A, Demezon H, Rigal J, Saddiki R, Aunoble S : Insufficient restoration of lumbar lordosis and FBI index following pedicle subtraction osteotomy is an indicator of likely mechanical complication. Eur Spine J 24 Suppl 1 : S112-S120, 2015   17. Lenke LG, Sides BA, Koester LA, Hensley M, Blanke KM : Vertebral column resection for the treatment of severe spinal deformity. Clin Orthop Relat Res 468 : 687-699, 2010   18. O’Shaughnessy BA, Kuklo TR, Hsieh PC, Yang BP, Koski TR, Ondra SL : Thoracic pedicle subtraction osteotomy for fixed sagittal spinal deformity. Spine (Phila Pa 1976) 34 : 2893-2899, 2009   19. Rose PS, Bridwell KH, Lenke LG, Cronen GA, Mulconrey DS, Buchowski JM, et al : Role of pelvic incidence, thoracic kyphosis, and patient factors on sagittal plane correction following pedicle subtraction osteotomy. Spine (Phila pa 1976) 34 : 785-791, 2009   20. Schwab F, Patel A, Ungar B, Farcy JP, Lafage V : Adult spinal deformitypostoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 35 : 2224-2231, 2010   21. Smith JS, Shaffrey CI, Ames CP, Demakakos J, Fu KM, Keshavarzi S, et al : Assessment of symptomatic rod fracture after posterior instrumented fusion for adult spinal deformity. Neurosurgery 71 : 862-867, 2012    22. Smith JS, Shaffrey E, Klineberg E, Shaffrey CI, Lafage V, Schwab FJ, et al : Prospective multicenter assessment of risk factors for rod fracture following surgery for adult spinal deformity. J Neurosurg Spine 21 : 994-1003, 2014   23. Sponseller PD, Jain A, Lenke LG, Shah SA, Sucato DJ, Emans JB, et al : Vertebral column resection in children with neuromuscular spine deformity. Spine (Phila PA 1976) 37 : E655-E661, 2012   24. Suk SI, Chung ER, Kim JH, Kim SS, Lee JS, Choi WK : Posterior vertebral column resection for severe rigid scoliosis. Spine (Phila Pa 1976) 30 : 1682-1687, 2005   25. Suk SI, Kim JH, Kim WJ, Lee SM, Chung ER, Nah KH : Posterior vertebral column resection for severe spinal deformities. Spine (Phila Pa 1976) 27 : 2374-2382, 2002  
|
|