Kim, Ryu, and Yoon: Is Adjacent Segment Disease More Frequent in Proximal Levels in Comparison with Distal Levels? Based on Radiological Data of at Least 2 Years Follow Up with More than 2 Level Thoracolumbar Fusions
Abstract
Objective
The purpose of this retrospective study was to determine which of the proximal adjacent segment disease (ASD) and distal ASD was more prevalent and what parameters is more related to ASD in proximal levels and distal levels after more than 2 levels fusions.
Methods
The medical records were reviewed retrospectively for 856 cases. A total of 66 cases of ASD were enrolled. On preop magnetic resonance imaging, disc degeneration was measured at the upper and lower parts of surgically treated levels and confirmed by the commonly used Pfirrmann grade. Segmental flexibility in sagittal plane was embodied in segment range of motion (ROM) obtained through flexion and extension X-ray before surgery. Coronal angle was recorded as methods Cobb’s angle including fusion levels preoperatively. For the comparison of categorical variables between two independent groups, the chi-square test and Fisher exact test were performed.
Results
Proximal ASD and distal ASD were 37/856 (4.32%) and 29/856 (3.39%), respectively. The incidence of proximal ASD was relatively high but insignificant differences. In comparison between ASD group and non ASD group, proximal Pfirmman was higher in proximal ASD and distal Pfirmman was higher in distal ASD group (p=0.005, p<0.008, respectively). However, in the ROM, proximal ROM was higher in proximal ASD, but distal ROM was not different between the two groups (p<0.0001, p=0.995, respectively). Coronal angle was not quite different in both groups (p=0.846).
Conclusion
In spite of higher frequency in ASD in proximal level in spinal fusion, it is not clear that incidence of ASD in proximal level is not higher than that of distal ASD group in more than 2 level thoracolumbar fusions. Not only Pfirrmann grade but also proximal segmental ROM is risk factor for predicting the occurrence of ASD in patients more than 2 level of thoracolumbar spine fusion operation excluding L5S1.
Key Words: Pfirrmann · Intervertebral disc degeneration · Range of motion, Articular · Segment flexibility · Adjacent segment disease · Radiographical ASD.
INTRODUCTION
Recently, the incidence of lumbar and lumbosacral spine fusion has been rapidly increasing as a treatment for degenerative diseases of spine, spinal deformity, trauma, infection, and tumors, and various complications have been reported [ 12]. Among them, adjacent segment disease (ASD) has had a significant impact on prognosis as it requires secondary surgery1 [ 5]. When the posterior fusion was performed, the percentage of ASD was 3% within 1 year, 16% within 5 years, and 36.1% within 10 years, and eight cases per 100 cases [ 9]. Reoperation due to ASD usually takes 5.2 to 7.1 years after the first operation [ 6]. The treatment of choice for ASD is typically fusion extension with additional pedicle screw fixation and rod elongation [ 13]. In general, ASD is a disease in which an increase in stress in the adjacent region after fusion results in a change in the contact surface and motion biomechanics of the nearby facet joint, resulting in degeneration of the vertebral segment [ 14]. Hilibrand and Robbins first proposed the term degenerative change of adjacent segments for radiologic changes of adjacent nodes after spinal fixation without considering clinical findings. On the other hand, ASD refers to when satisfying clinical requirements while satisfying degenerative changes of adjacent segments [ 7]. ASD requires additional intervention and ultimately adversely affects the patient. Therefore, it is important to know in advance whether there is a risk factor for ASD and to determine the extent and timing of the surgery [ 5]. There have been many studies on risk factors and it has been known that age, sex, bone quality, multi-level fusion, high body mass index, preoperative disc degeneration at adjacent levels, and intra-operative damage at adjacent levels have a major influence on ASD [ 10]. In this paper, we have narrowed the scope of the study to patients with ASD after more than 2 levels spinal fusion, which is considered as one of the risk factors mentioned above. The purpose of the study was to determine which of the proximal ASD and distal ASD was more prevalent and what correlates with ASD among the various parameters.
MATERIALS AND METHODS
This study was approved by Institutional Review Board of Inha University Hospital (IRB No. 2019-05-011). Total 1217 patients who underwent more than 2 level thoracolumbar posterior fusion at a single medical center from January 2008 to December 2018 were enrolled. Because inclusion of fusion at L5/S1 segment may result in distorted outcomes in the prevalence of proximal and distal ASD, it is therefore set to exclusion criteria. Eight hundred fifty six cases were included in this study. The medical records were reviewed retrospectively for 856 cases ( Table 1).
Clinical and radiologic evaluations
ASD is a concept that includes both “radiographical ASD” and “clinical ASD”. Radiographical ASD is a term referring to radiologic change that occurs in adjacent segment. Clinical ASD refers to when there are both radiological finding and clinical symptoms of the relevant part.
The ASD group was selected according to the following radiographic ASD criteria on spine X-rays. Radiographical ASD on radiographs was defined as a reduction of ≤50% in disc height on a neutral lateral radiograph, an increase of ≥3 mm in vertebral slip on a neutral lateral radiograph, and a decrease of ≥5° in the intervertebral angle on a flexion lateral radiograph [ 11]. Degeneration of proximal and distal adjacent level following fusion was evaluated with postoperative X-ray. In order to assess the patient’s general information, the age, gender, number of fused segments, and the time to diagnose ASD since initial surgery were collected. The number of segments was classified by the number of fusion level irrespective of location, and the occurrence time was calculated monthly. Second, for all enrolled patients, lumbar lordotic angle (LLA; T12 to S1) and pelvic parameters were measured on a X-ray. The pelvic parameters included pelvic incidence (PI), pelvic tilt, and sacral slope. Finally, the disc degeneration and segment flexibility of the upper and lower parts were measured. On pre-op magnetic resonance imaging, disc degeneration was measured at the upper and lower parts of surgically treated levels and confirmed by the commonly used Pfirrmann grade.
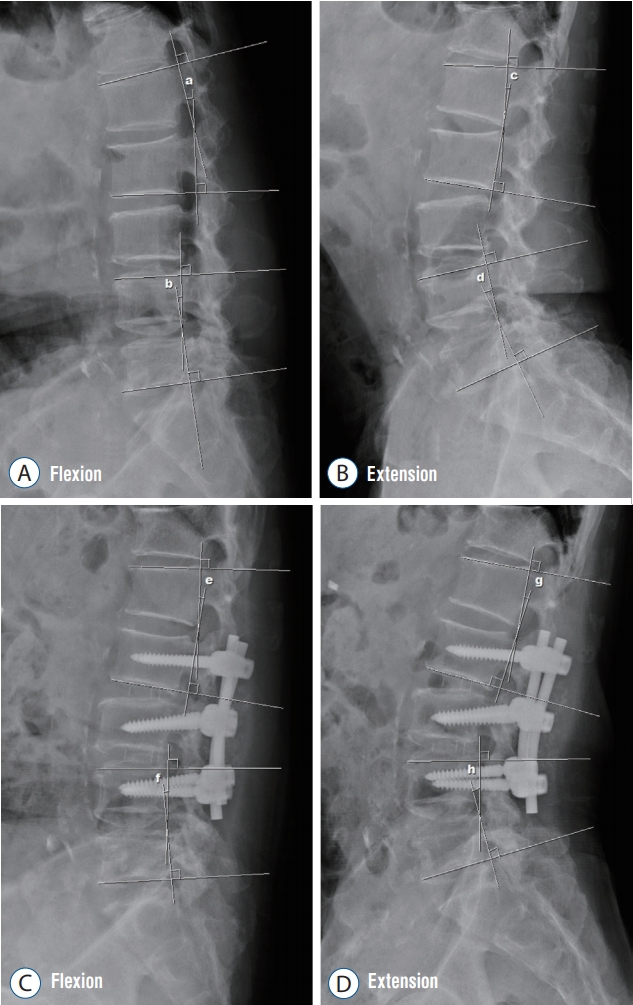
Range of motion (ROM) was embodied in segment ROM obtained through Flexion and Extension X-ray before surgery. The upper and lower Cobb’s angle of screw insertion were measured and the difference was set as ROM. The measurement of Cobb’s angle involves estimating the angle between the two tangents of the upper and lower endplates of the upper and lower end vertebra, respectively. For example, in case of L1 screw, Cobb’s angle between upper margin of T12 and lower margin of L1 are obtained in the flexion extension image. An example of the measurement is shown in Fig. 1. In addition, coronal angle was recored as methods Cobb’s angle including fusion levels preoperatively.
Statistical analysis
All statistical analyses were performed using SPSS version 18.0 (SPSS Inc., Chicago, IL, USA). Descriptive data are presented as mean±standard deviation. Student t-tests were conducted to confirm intergroup differences in cases with normal distributions. For the comparison of categorical variables between two independent groups, the chi-square test and Fisher exact test were performed. All p-values less than 0.05 were considered to indicate statistical significance.
RESULTS
Demographics
Out of 856 patients except total 5S1 fusion, ASD patients were 66 cases including radiographical ASD 28 cases. Proximal ASD and distal ASD were 37/856 (4.32%) and 29/856 (3.39%), respectively ( Table 2). There was no significant difference, but the incidence of proximal ASD was high. Both groups had higher rates of women. There was no significant difference in age between the two groups. In both groups, the disease occurred at around 2 years after surgery. In scoliosis patients, there were no significant differences in proximal and distal four and three cases, respectively, in total seven cases.
Pfirmman grade and range of motion
Comparing the ROM of the ASD site and the ROM of the non-ASD site, it was confirmed that the ROM of the occurrence site was larger, which corresponds to both proximal and distal ASD (p=0.045, p<0.0001, respectively). The Pfirmman grade was also found to be larger at the site of ASD (p=0.048, p<0.0001, respectively). In comparison between ASD group and non ASD group, proximal Pfirmman was higher in proximal ASD and distal Pfirmman was higher in distal ASD group when the absolute value of Pfirmman grade was considered (p=0.005, p=0.008, respectively). However, in the ROM, proximal ROM was higher in proximal ASD, but distal ROM was not different between the two groups (p<0.0001, p=0.995, respectively). There was not a considerable difference in coronal Cobb’s angle for both groups (p=0.846).
DISCUSSION
Generally, according to previous clinical and biomechanical studies, proximal ASD has a higher prevalence rate than distal ASD [ 2]. However, according to the present study, the prevalence of proximal ASD and distal ASD was similar in cases of more than 2 level ( Table 2). However, because this study is a retrospective study, the ASD incidence may be underestimated as some patients may not follow up [ 8]. In the biomechanical study, we considered the increased prevalence of degenerative disease adjacent to the site of bony fusion as the main mechanism of ASD. In other words, depending on the nature of the degenerative disease, the incidence rate tends to increase over time. In addition, Axelsson et al. [ 3] assessed adjacent segments with the use of radiographic analysis and found hypermobility in the juxtafused segment. We have estimated that ROM can be a measure of the characteristics of hypermobility. Therefore, we considered segment ROM as a risk factor of ASD. Postoperative ASD was more prevalent with preoperative disc degeneration, which was confirmed by case study and biomechanical analysis. Although this study was limited to more than 2 levels, ASD was also more common as disc regression was severe.
Study was performed to measure the Pfirmman grade and segmental ROM of not only the deformed part of adjacent segments but also the other part. In the Pfirmann grade, the Pfirmman grade was higher in the ASD site than in the non ASD site. Segmental ROM was also found to be greater in the ASD site than in the non ASD site. The interesting thing is that although the allowable ROM values for each segment would be different, but ROM of ASD segment is greater than that of non-ASD region.
There was no statistically significant difference in LLA (T12 to S1) and pelvic parameters between ASD group and non ASD group. In the Pfirmann grade, the Pfirmman grade was higher in ASD group than in non-ASD group. Segmental ROM was also found to be higher in the area with ASD than in the area without ASD. In proximal ROM, proximal ASD group was larger than non ASD group ( Table 3). However, distal ROM had similar values in distal ASD group and non ASD group ( Table 4). In conclusion, it is difficult to estimate the distal ROM values as a predictor of distal ASD. Overall, if distal ASD occurs, there is a high probability that distal segmental ROM is higher than proximal segmental ROM, but it is unreasonable to predict distal ASD as the absolute value of distal segmental ROM. In patients who underwent thoracolumbar fusion, there is a limitation of flexion and extension motions in distal segment. This is because the distal segment is located between the sacral segment and the fused segment after surgery, even though the preoperative ROM of the distal segment is large. However, since the proximal segment has no limitation of flexion extension after surgery, the bending moment of proximal segment is relatively larger than that of distal segment. For this reason, it seems that distal segmental ROM and distal ASD are low in correlation. From this perspective, further biomechanical study may be needed.
In conclusion, although it is not known whether ASD will occur or not, the comparison of Pfirmman grade and segmental ROM of the proximal part and distal part before surgery shows that there is a high probability of ASD at the larger value.
There is no absolute reference value of ROM for each segment, and it is difficult to predict ASD only by the ROM value. However, the significance of this paper is that the extent of proximal segmental ROM was associated with the presence of proximal ASD. Furthermore, proximal segmental ROM is a good indicator of determining fusion level, as the level of surgery is extended when the proximal segmental ROM is large.
Previous studies related to the association between ASD and the ROM of the segment have been made in the cervical spine. In 2016, Ahn et al.1) examined to find out the radiologic findings and risk factors related to ASD after anterior cervical discectomy and fusion. At 36 months postoperatively, the difference for upper cervical ROM value from the preoperative one significantly increased in the ASD group than non-ASD group. Upper segment range of motion (USROM) and lower segment range of motion (LSROM) increased in both groups as time passed after surgery. The mean USROM and LSROM changes tended to be greater in the ASD group than the nonASD group. It remains unclear whether this change represents a true iatrogenic post-operative complication or a progression of the natural history of spondylosis [ 1]. There is another study of ROM changes of adjacent segment after posterior fusion. In 2015, Bisschop et al. [ 4] studied the ROM and stiffness of adjacent lumbar spinal segments along with ASD following laminectomy and fusion, utilizing 12 human lumbar cadaveric spines. With instrumentation, the ROM at the adjacent segment was reduced (-12.9%) compared with that before surgery [ 4]. The limitations of this study are the lack of population and the distorted nature of the prevalence seen in the retrospective study. In the future, we expect a follow-up study that can provide a standard that the risk of ASD increases if the ROM value is more than a certain size by specifying the absolute value of ROM for each segment. Although the population was small, proximal ASD tended to be more frequent as the lumbar lordotic angle was small. This suggests that the greater the PI value than the lumbar lordotic angle, the more proximal junctional kyphosis occurs. Objective research on this may also be meaningful.
CONCLUSION
It is found that not only Pfirrmann but also proximal segmental ROM is known as a risk factor for predicting the occurrence of ASD in patients more than 2 level of thoracolumbar spine fusion operation excluding 5S1. Among the proximal segment and the distal segment, the segment with a larger ROM value tended to have a higher risk of developing ASD, so that segmental ROM is a good indicator for predicting the extent of surgery or predicting ASD.
Fig. 1.
Pre (A and B) and postoperative (C and D) flexion-extension views of the lumbar spine. The upper and lower endplate Cobb's angles were used. The difference (c-a) and difference (d-b) were set as preoperative proximal ROM and preoperative distal ROM, respectively. Likewise, postoperative proximal ROM is the difference (g-e) and postoperative distal ROM is difference (h-f). ROM : range of motion. 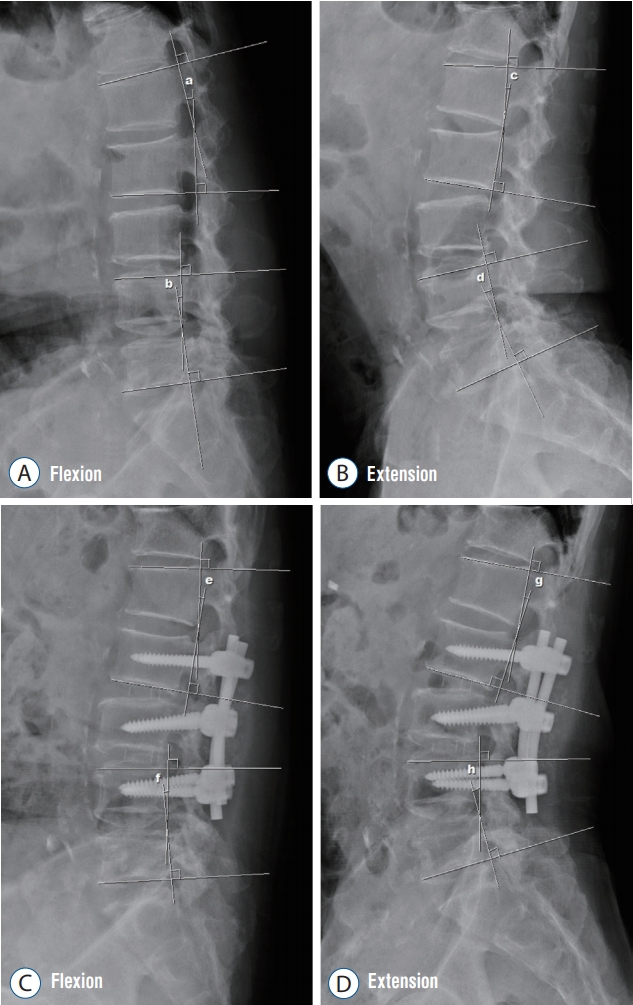
Table 1.
Baseline characteristics for total 856 patients who underwent multi-level lumbar spinal fusion
|
Value (n=856) |
|
Age (years) |
61.28±13.24 |
|
M : F |
271 : 585 |
|
2 level fusion |
623 (72.78) |
|
3 level fusion |
101 (11.80) |
|
4 level fusion |
44 (5.14) |
|
More than 5 level fusion |
88 (10.28) |
|
Proximal ASD |
37/856 (4.32) |
|
Distal ASD |
29/856 (3.39) |
|
Concurrent proximal & distal ASD |
2 |
Table 2.
Demographic characteristics of the proximal ASD group and the distal ASD group
|
Proximal ASD |
Distal ASD |
p-value |
|
Patient |
37/856 (4.32) |
29/856 (3.39) |
|
|
Age (years) |
66.84±9.04 |
65.28±14.96 |
0.602 |
|
M : F |
14 : 23 |
8 : 21 |
0.381 |
|
2 level fusion |
20 |
9 |
0.277 |
|
3 level fusion |
11 |
13 |
|
|
4 level fusion |
1 |
1 |
|
|
5 more level fusion |
5 |
6 |
|
|
Follow up (months) |
42.36±18.89 |
41.17±22.44 |
0.816 |
Table 3.
Comparison of disc degeneration, range of motion between proximal ASD group and non ASD group
|
Proximal ASD |
Non-ASD |
p-value |
|
Lumbar lordotic angle (°) |
37.24±9.35 |
39.13±10.02 |
0.882 |
|
Pelvic incidence (°) |
50.52±6.86 |
55.23±8.84 |
0.698 |
|
Pelvic tilt (°) |
18.78±4.79 |
16.02±5.46 |
0.722 |
|
Sacral slope (°) |
31.80±4.86 |
39.12±10.03 |
0.356 |
|
Proximal flexion angle (°) |
4.93±5.81 |
3.41±2.97 |
0.207 |
|
Proximal extension angle (°) |
11.14±6.44 |
6.37±3.1 |
0.001*
|
|
Proximal range of motion (°) |
6.24±4.12 |
2.95±2.01 |
<0.0001*
|
|
Proximal Pfirrmann grade |
3.57±0.77 |
3.00±0.8 |
0.005*
|
Table 4.
Comparison of disc degeneration, range of motion between distal ASD group and non ASD group
|
Distal ASD |
Non-ASD |
p-value |
|
Lumbar lordotic angle (°) |
34.19±11.23 |
39.13±10.02 |
0.783 |
|
Pelvic incidence (°) |
49.63±8.19 |
55.23±8.84 |
0.643 |
|
Pelvic tilt (°) |
14.26±6.37 |
16.02±5.46 |
0.831 |
|
Sacral slope (°) |
34.54±9.28 |
39.12±10.03 |
0.718 |
|
Distal flexion angle (°) |
6.44±4.35 |
12.45±7.15 |
<0.0001 |
|
Distal extension angle (°) |
12.24±5.66 |
18.26±8.58 |
0.002*
|
|
Distal range of motion (°) |
5.79±3.22 |
5.80±4.89 |
0.995 |
|
Distal Pfirrmann grade (°) |
3.69±0.47 |
3.16±0.96 |
0.008*
|
References
3. Axelsson P, Johnsson R, Strömqvist B, Arvidsson M, Herrlin K : Posterolateral lumbar fusion. Outcome of 71 consecutive operations after 4 (2-7) years. Acta Orthop Scand 65 : 309-314, 1994   4. Bisschop A, Holewijn RM, Kingma I, Stadhouder A, Vergroesen PP, van der Veen AJ, et al : The effects of single-level instrumented lumbar laminectomy on adjacent spinal biomechanics. Global Spine J 5 : 39-48, 2015   5. Chen WJ, Lai PL, Niu CC, Chen LH, Fu TS, Wong CB : Surgical treatment of adjacent instability after lumbar spine fusion. Spine (Phila Pa 1976) 26 : E519-E524, 2001   6. Guyer RD, Patterson M, Ohnmeiss DD : Failed back surgery syndrome: diagnostic evaluation. J Am Acad Orthop Surg 14 : 534-543, 2006   7. Hilibrand AS, Robbins M : Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J 4( 6 Suppl):190S-194S, 2004   8. Lawrence BD, Wang J, Arnold PM, Hermsmeyer J, Norvell DC, Brodke DS : Predicting the risk of adjacent segment pathology after lumbar fusion: a systematic review. Spine (Phila Pa 1976) 37( 22 Suppl):S123-S132, 2012   10. Majid K, Fischgrund JS : Degenerative lumbar spondylolisthesis: trends in management. J Am Acad Orthop Surg 16 : 208-215, 2008   11. Nakashima H, Kawakami N, Tsuji T, Ohara T, Suzuki Y, Saito T, et al : Adjacent segment disease after posterior lumbar interbody fusion: based on cases with a minimum of 10 years of follow-up. Spine (Phila Pa 1976) 40 : E831-E841, 2015  12. Rajaee SS, Bae HW, Kanim LE, Delamarter RB : Spinal fusion in the United States: analysis of trends from 1998 to 2008. Spine (Phila Pa 1976) 37 : 67-76, 2012   13. Ryu DS, Park JY, Kuh SU, Chin DK, Kim KS, Cho YE, et al : Surgical outcomes after segmental limited surgery for adjacent segment disease: the consequences of makeshift surgery. World Neurosurg 110 : e258-e265, 2018   14. Schlegel JD, Smith JA, Schleusener RL : Lumbar motion segment pathology adjacent to thoracolumbar, lumbar, and lumbosacral fusions. Spine (Phila Pa 1976) 21 : 970-981, 1996   15. Zhang C, Berven SH, Fortin M, Weber MH : Adjacent segment degeneration versus disease after lumbar spine fusion for degenerative pathology: a systematic review with meta-analysis of the literature. Clin Spine Surg 29 : 21-29, 2016  
|
|