Mahatthanatrakul, Kotheeranurak, Lin, Hur, Chung, Lokanath, Pakdeenit, and Kim: Do Obliquity and Position of the Oblique Lumbar Interbody Fusion Cage Influence the Degree of Indirect Decompression of Foraminal Stenosis?
Abstract
Objective
Oblique lumbar interbody fusion (OLIF) is a surgical technique that utilizes a large interbody cage to indirectly decompress neural elements. The position of the cage relative to the vertebral body could affect the degree of foraminal decompression. Previous studies determined the position of the cage using plain radiographs, with conflicting results regarding the influence of the position of the cage to the degree of neural foramen decompression. Because of the cage obliquity, computed tomography (CT) has better accuracy than plain radiograph for the measurement of the obliquely inserted cage. The objective of this study is to find the correlation between the position of the OLIF cage with the degree of indirect decompression of foraminal stenosis using CT and magnetic resonance imaging (MRI).
Methods
We review imaging of 46 patients who underwent OLIF from L2-L5 for 68 levels. Segmental lordosis (SL) was measured in a plain radiograph. The positions of the cage were measured in CT. Spinal canal cross-sectional area (SCSA), and foraminal crosssectional area (FSCA) measurements using MRI were taken into consideration.
Results
Patients’ mean age was 69.7 years. SL increases 3.0±5.1 degrees. Significant increases in SCSA (33.3%), FCSA (43.7% on the left and 45.0% on the right foramen) were found (p<0.001). Multiple linear regression analysis shows putting the cage in the more posterior position correlated with more increase of FSCA and decreases SL correction. The position of the cage does not affect the degree of the central spinal canal decompression. Obliquity of the cage does not result in different degrees of foraminal decompression between right and left side neural foramen.
Conclusion
Cage position near the posterior part of the vertebral body increases the decompression effect of the neural foramen while putting the cage in the more anterior position correlated with increases SL.
Key Words: Decompression, surgical · Lumbosacral region · Magnetic resonance imaging · Spinal fusion · Tomography, X-ray computed.
INTRODUCTION
Many factors give rise to lumbar foraminal stenosis, such as a decrease in foraminal height, translation of vertebral body, osteophytes, hypertrophy of ligamentum flavum, or bulging of annulus fibrosus [ 4, 23, 27]. Surgical management of the foraminal stenosis consists of direct or indirect decompression. The detriment of direct decompression includes neural structures injury, cerebrospinal fluid leakage, postoperative hematoma, and difficulty in revision cases [ 19]. Indirect decompression is an alternative method for decompression of the neural elements. By inserting lordotic cages with a large footprint, the surgeon can correct the coronal and sagittal deformities, and indirectly decompress the neural elements by the ligamentotaxis effect of the cage [ 1, 3, 6, 19, 20, 25]. The minimally invasive retroperitoneal anterior to psoas approach was introduced by Mayer [ 13], and the term oblique lumbar interbody fusion (OLIF) was described with emphasis on reducing psoas muscle weakness and sensory deficit, compared to trans-psoas approach [ 2, 14, 15, 18, 26, 28]. Characteristics and position of the cage were supposed to be the important surgical factors affecting the successfulness of indirect decompression after OLIF. Hypothetically, putting cages closer to the posterior border of vertebral body should increase the indirect decompression effect of the neural foramen. The primary question of this study is whether the position of the cage, measured in computed tomography (CT), is associated with indirect decompression of foraminal stenosis. The secondary outcomes are indirect decompression of the central spinal canal, lordosis correction, and different degrees of decompression when measuring with dissimilar imaging modalities.
MATERIALS AND METHODS
This study was approved by the Institutional Review Board of Seoul St. Mary's Hospital (IRB No. KC14OISI0034). Informed consent was exempted due to the retrospective nature of this study. We retrospectively reviewed patients who had undergone OLIF from June 2013 to June 2019 inclusion criteria were those aged above 18 years, who had symptomatic degenerative lumbar spinal diseases with spinal instability as demonstrated by dynamic radiograph, with at least grade one foraminal canal stenosis on magnetic resonance imaging (MRI). They underwent single or multiple level OLIF and had completed postoperative MRI. Exclusion criteria were OLIF at L5-S1 level; concomitant direct decompression; patients who also had an acute infection, fractures, previous spinal fusion, or cancer in spinal elements and cases in which postoperative MRI parameters cannot be evaluated, due to metallic artifact from spinal instruments.
Clinical outcomes were prospectively collected during the preoperative period and the follow-up period. The self-reported measurements used were the Oswestry Disability Index (ODI), numerical rating scale (NRS) for back pain, and leg pain.
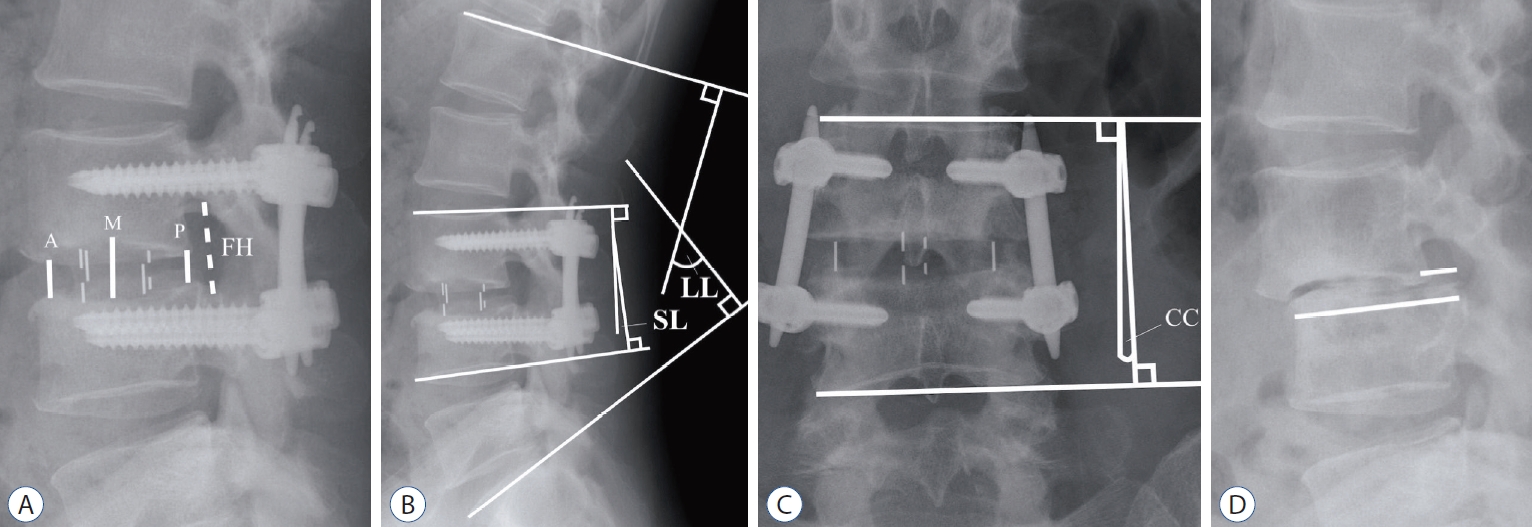
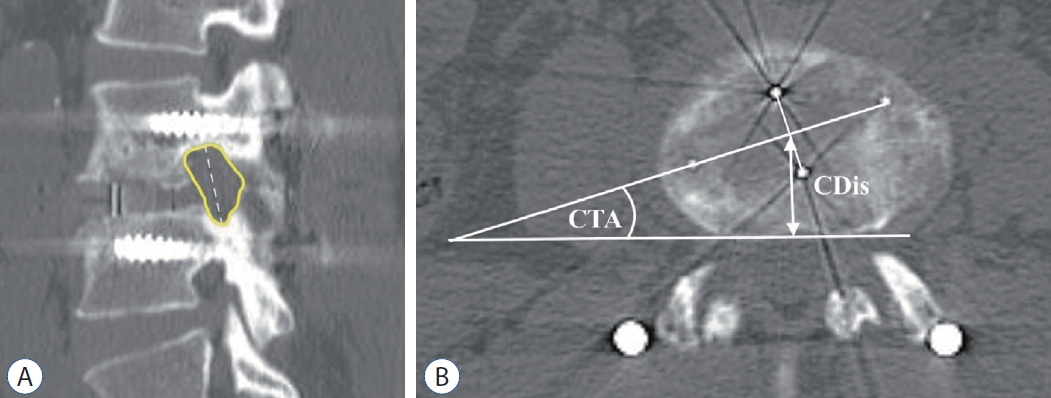
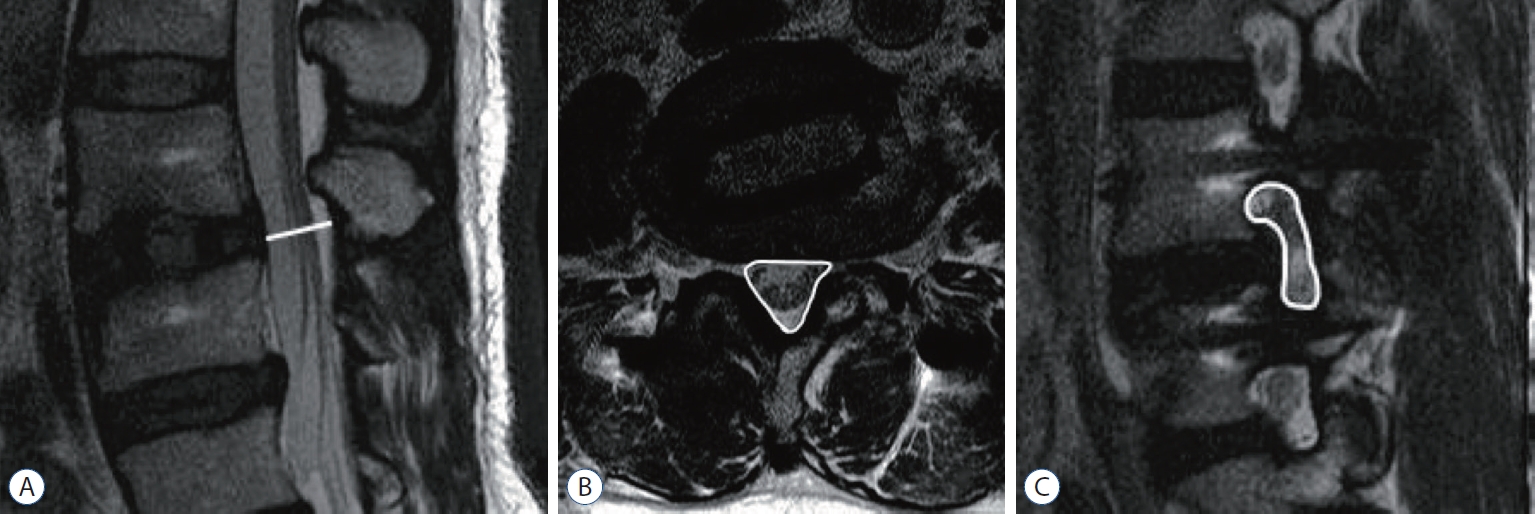
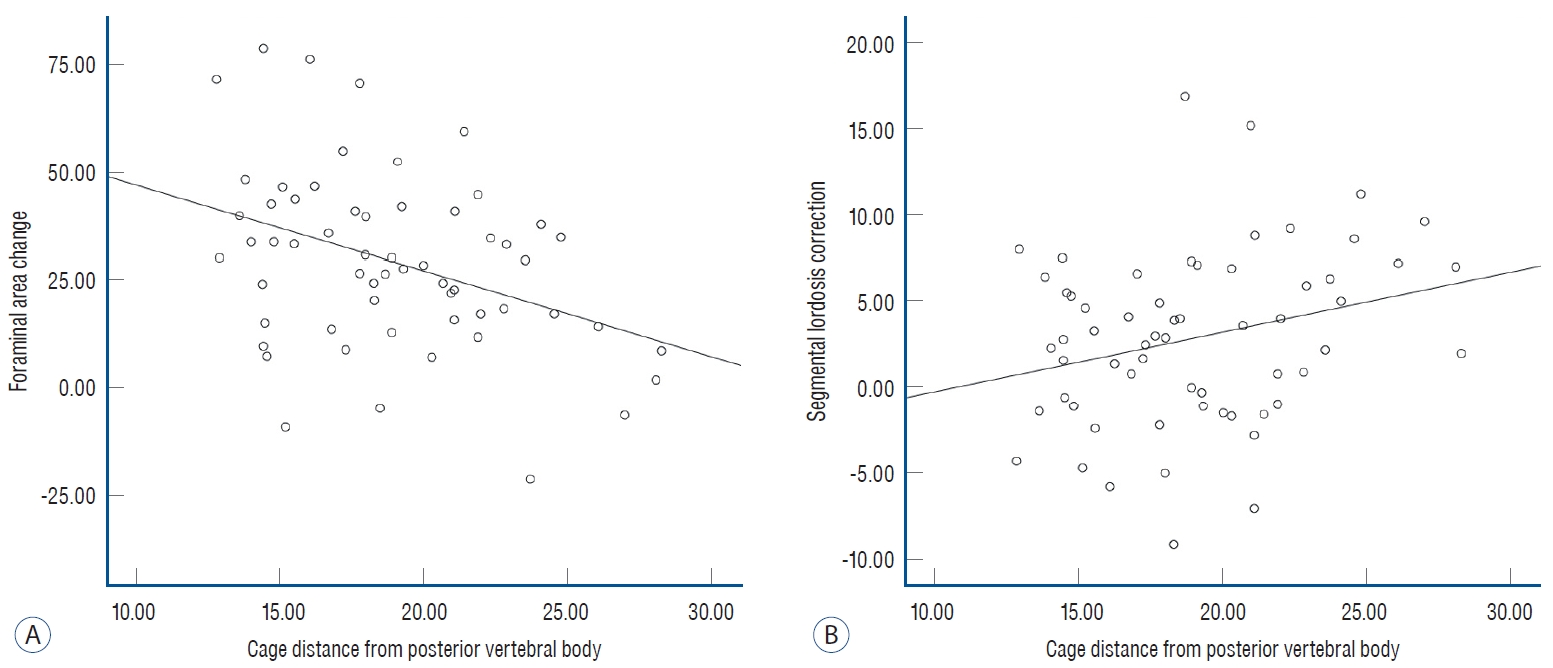
The OLIF procedures were performed in a right lateral decubitus position using the mini-open retroperitoneal anterolateral approach, as described in a previous study [ 5]. The cages (Clydesdale PEEK; Medtronic, Memphis, TN, USA) were inserted together with demineralized bone matrix (Grafton; Medtronic) or bioactive glass (Novabone; Novabone products LLC, Alachua, FL, USA) as the bone graft substitute. Posterior fixation with either percutaneous pedicle screws or mini-open cortical bone trajectory screw was carried out. Plain radiographs were taken in standing positions preoperatively and at a 1-month postoperative follow-up. The mean disc height (DH) was calculated by obtaining the average of the anterior, middle, and posterior DHs ( Fig. 1). Foraminal height (FH) was defined as the distance between the inferior border of the pedicle of the upper level to the superior border of the pedicle of the lower level vertebra. Segmental lordosis (SL) was defined as an angle between the upper endplate of the superior level vertebra and the lower endplate of the lower level vertebra. Lumbar lordosis (LL) was defined as an angle between the lines parallel to an upper endplate of the L1 vertebral body and S1 vertebral body. Spondylolisthesis slip percentage was calculated by the slip distance divided by upper vertebral endplate distance. CT scans were taken in supine positions preoperatively, and between 6 to 12 months postoperatively for evaluation of fusion. FH and foraminal cross-sectional area (FSCA) were measured in the sagittal image in the middle zone of neural foramens. The position of the cage was measured by drawing the line at the posterior of the vertebral body and draw a perpendicular line to the middle of the cage. The trajectory of an interbody cage (cage trajectory angle) was defined as an angle between a line along the length of the cage and a line at the posterior of the vertebral body ( Fig. 2). MRIs were taken in supine position preoperatively and immediate postoperative period (within 3 days) to evaluate the adequacy of decompression. Spinal canal width was measured in sagittal T2-weighted MRI at the broadest cut ( Fig. 3). Spinal canal cross-sectional area (SCSA) was measured in axial T2-weighted image MRI. FSCA was measured in sagittal T2-weighted MRI in the middle zone of the neural foramen. Foraminal stenosis was graded, according to Lee et al. [ 10]. All measurements were done on the picture archives communication system, MaroView 4.5 (Marotech, Seoul, Korea).
Statistical analysis
The normality of data was tested by the Shapiro-Wilk test. Normally distributed data were reported as the mean±standard deviation. Non-parametric data were reported as median (interquartile range, IQR). Differences between preoperative and postoperative parameters and between different imaging modalities were compared by the paired t-test. The relationship between MRI parameters and cage position was tested by linear regression analysis. Independent variables with a p-value <0.10 in simple linear regression were further analyzed in a multiple linear regression model. Statistical significance was considered if the p-value <0.05. All tests were two-tailed. Statistical analysis was done using IBM SPSS version 21 (IBM Corp., Armonk, NY, USA).
RESULTS
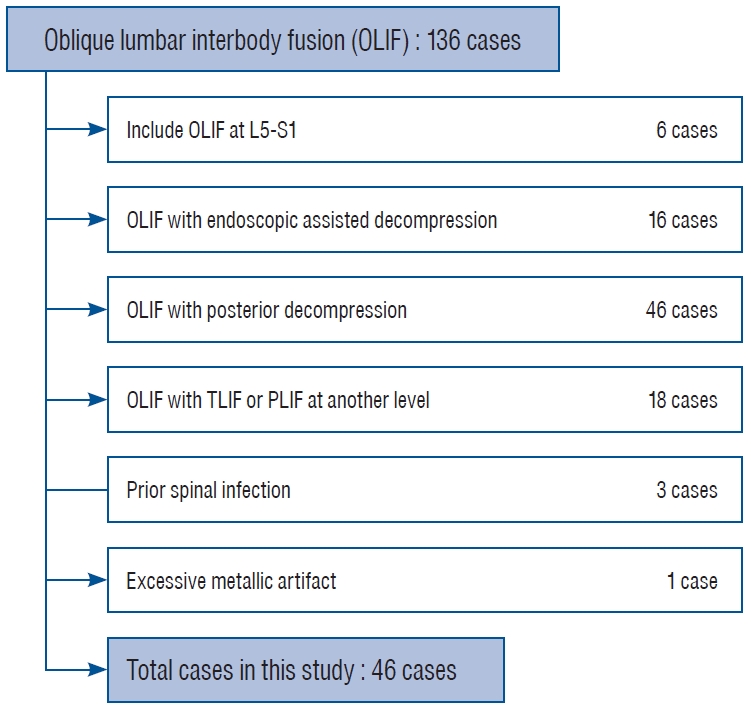
A total of 136 patients met the inclusion criteria. Ninety patients were excluded according to the exclusion criteria ( Fig. 4). The total number of patients left in this study was 46. The mean age of the patients was 69.7±9.0 years. Demographic data and the diagnosis are presented in Table 1. Cage parameters are detailed in Table 2. Posterior fixations were done with pedicle screws in 59 levels and with cortical bone trajectory screws in 9 levels. The median follow-up period was 12 months (IQR, 8.25; range, 6 to 41 months) postoperative NRS for back pain, leg pain, and ODI were significantly improved ( Table 3).
Radiographic parameters
Table 4 shows the comparison between preoperative and postoperative imaging parameters. In the level that used the cages with 6-degree lordosis, SL increased from 6.5±6.6 degrees to 9.4±5.9 degrees. With a 12-degree lordosis cage, SL increased from 9.5±5.8 degrees to 12.3±6.3 degrees. The increment of SL was the same between the levels that used a 6 or 12-degree cage ( p=0.92). LL increased by 5.5±6.8 degrees in the single level OLIF group (95% confidence interval [CI], 2.4 to 8.1 degrees) and 8.2±7.0 degrees in multiple level OLIF group (95% CI, 2.9 to 12.4 degrees) without statistical differences between groups ( p=0.23). In the single level OLIF group, utilization of 6-degree lordosis cage or 12-degree lordosis cage resulted in similar LL change (5.4±7.2 degrees and 5.8±5.3 degrees respectively, p=0.91).
CT parameters
The left and right FSCA increased by 19.5% and 15.6% in the postoperative CT scan ( Table 4). There was no statistical difference between the left and right side FH and FSCA gain postoperatively ( p=0.12 and 0.40).
MRI parameters
Spinal canal width increased by 28.8%, SCSA increased by 33.3% compared to preoperative MRI. The left and the right FSCA increased by 43.7% and 45.0%, respectively. Percentage change of the left and the right FSCA did not become different ( p=0.87). Foraminal stenosis grades were unchanged in 57 foramens, decreased 1 grade in 46 foramens, decreased 2 grades in 18 foramens, increased 1 grade in three foramens, and unmeasurable due to the metallic artifact in 12 foramens. The median of foraminal stenosis grade was reduced from grade 2 to grade 1 ( Table 4). SCSA was unmeasurable due to the metallic artifact in 3 levels (6%). The rate of the metallic artifact was not different between fixation by pedicle screws or cortical bone trajectory screws ( p=0.50). Linear regression analysis showed no correlation between cage parameters and SCSA increment ( Table 5). Factors associated with SCSA increment were anterior DH gained and preoperative SCSA. Table 6 demonstrated that cage distance and preoperative FSCA were inversely associated with postoperative FSCA increment while DH change was not associated with postoperative FSCA increment in the multiple linear regression analysis. Anterior implantation of the cage is associated with a greater amount of SL correction ( Table 7). Linear correlation between cage position and foraminal stenosis decompression, and SL correction was shown in Fig. 5.
DISCUSSION
Clinical and radiographic parameters among different imaging modalities
The lateral lumbar interbody fusion (LLIF) could be done by trans-psoas approach or ante-psoas approach. These approaches had proved to adequately decompress the central canal, lateral recess, and neural foramen [ 1, 6- 8, 16, 19, 21, 22, 25]. Radiographic parameters showing the indirect decompression by OLIF in our study were similar to previous studies on LLIF, which were measured by the same imaging modality [ 6, 19, 21]. However, our study demonstrated a 30-46% difference in the FSCA decompression between the measurements using CT and MRI. The MRI study after LLIF by Park et al. [ 21] also found that the increment in the FSCA was 69.5%, which was higher than an average increase of 32.5% to 38.9% using plain radiograph or CT [ 9]. The disparity in the FSCA change reflects the effect of indirect decompression on soft tissues, which were more challenging to detect on CT. This difference between imaging modalities should be considered when comparing results between studies, especially in systematic review and meta-analysis. The effectiveness of indirect decompression is reflected in postoperative outcomes as 51% improvement in ODI and 73% improvement in NRS for back pain and 67% for leg pain. However, the correlation could not be found between radiographic parameters and clinical outcomes; the finding consistent with previous studies [ 3, 6, 17, 24].
Effects of cage parameters on foraminal stenosis
The factors that influence the indirect decompression of neural foramen are still controversial [ 9, 21, 22]. Park et al. [ 21] and Lin et al. [ 12] reported that putting LLIF cage into anterior 1/3 or middle 1/3 of the vertebral body resulted in the similar FSCA decompression. Limthongkul et al. [ 11] divide LLIF cage positions into anterior and posterior groups and also found insignificant differences between groups. The utilization of plain radiographs and dividing cage positions into groups from the aforementioned studies may be inadequate to detect the actual difference. Our study measures the cage position using axial CT, which can pinpoint the center position of the OLIF cages, so we can demonstrate that putting the cage closer to the posterior part of the vertebral body correlated with better FSCA decompression. Surgeons performing OLIF usually use the corridor between the aorta and psoas muscle and implement the orthogonal maneuver to reduced the cage trajectory angle but the final position of the cage may not parallel to the posterior vertebral body. The oblique position of the cage means the right end of the cage is closer to the neural foramens than the left end, which may result in the asymmetric decompression of neural foramens. Sato et al. [ 24] reported that, after OLIF, there were 39% and 21% increments of right and left FSCA respectively. However, they did not report the degree of the obliquity of the cage in their series. Limthongkul et al. [ 11] reported that putting OLIF cages obliquely at 6 degrees does not affect the differences between right and left neural foramen decompression. Our study suggested that even the cages were oblique at the mean of 14 degrees, both sides of the neural foramen could be equally decompressed ( Table 4).
Factor associated with central spinal canal decompression
Indirect decompression of the central spinal canal by OLIF had been studied extensively by correlating the distraction of the intervertebral disc with SCSA decompression [ 12, 21, 24]. Our finding that expansion of DH associated with an increment in central canal decompression was supported by previous studies. The multivariate analysis showed that cage morphology and position were not associated with the percentage change of SCSA, similar conclusions were reported [ 11, 12, 21].
Effects of cage parameters on SL
Position of the cage in the anterior part of the vertebral body associated with greater correction of SL [ 12, 21]. Our study has similar results and also suggested that each 1 mm of cage position further from the posterior part of the vertebral body correlated with a better 0.3 degree of SL correction.
Limitations
Limitations of this study are small sample sizes and retrospective review nature. The MRIs, done at the immediate postoperative, could overestimate the efficacy of the indirect decompression because late cage subsidence may occur and could result in decreased central and neural foramen. CTs and MRIs from our study were also not done at the same time, making a parallax in the comparison between these two modalities.
CONCLUSION
Cage position associated with the degree of SL correction and decompression of foraminal stenosis, but not associated with central canal decompression. Surgeons performing OLIF should balance the amount of lordosis correction needed and the necessity to decompress the foraminal canal. Differences between measurement methods should be considered when comparing the degree of decompression from different studies.
Fig. 1.
Radiographic measurements. A : Anterior (A) middle (M) and posterior (P) disc height and foraminal height (FH). B : Segmental lordosis (SL) and lumbar lordosis (LL). C : Coronal Cobb’s angle (CC). D : Spondylolisthesis slip percentage was calculated from slip distance divided by the width of the lower vertebral body. 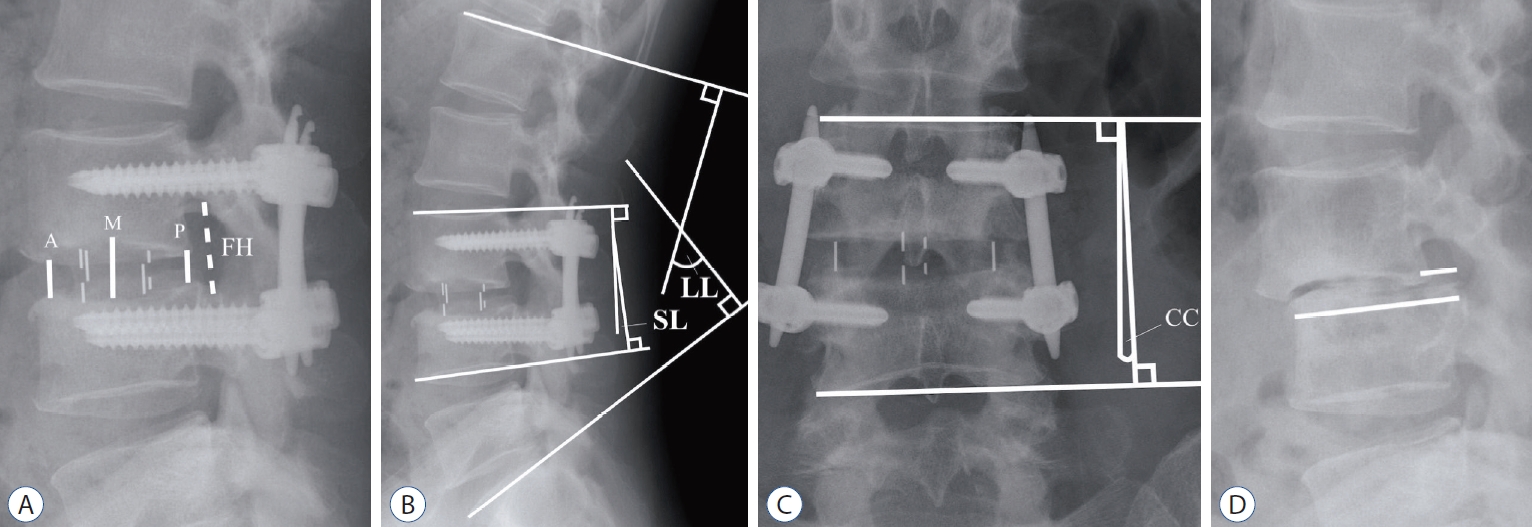
Fig. 2.
Computed tomography measurements. A : Foraminal cross-sectional area and foraminal height (FH). B : Cage distance (CDis) and cage trajectory angle (CTA). 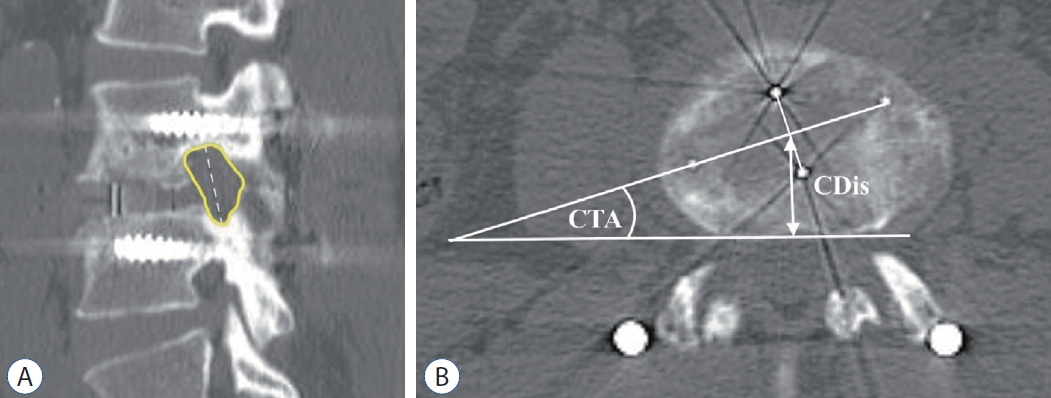
Fig. 3.
Magnetic resonance imaging measurements. A : Spinal canal width. B : Spinal canal cross-sectional area. C : Foraminal cross-sectional area. 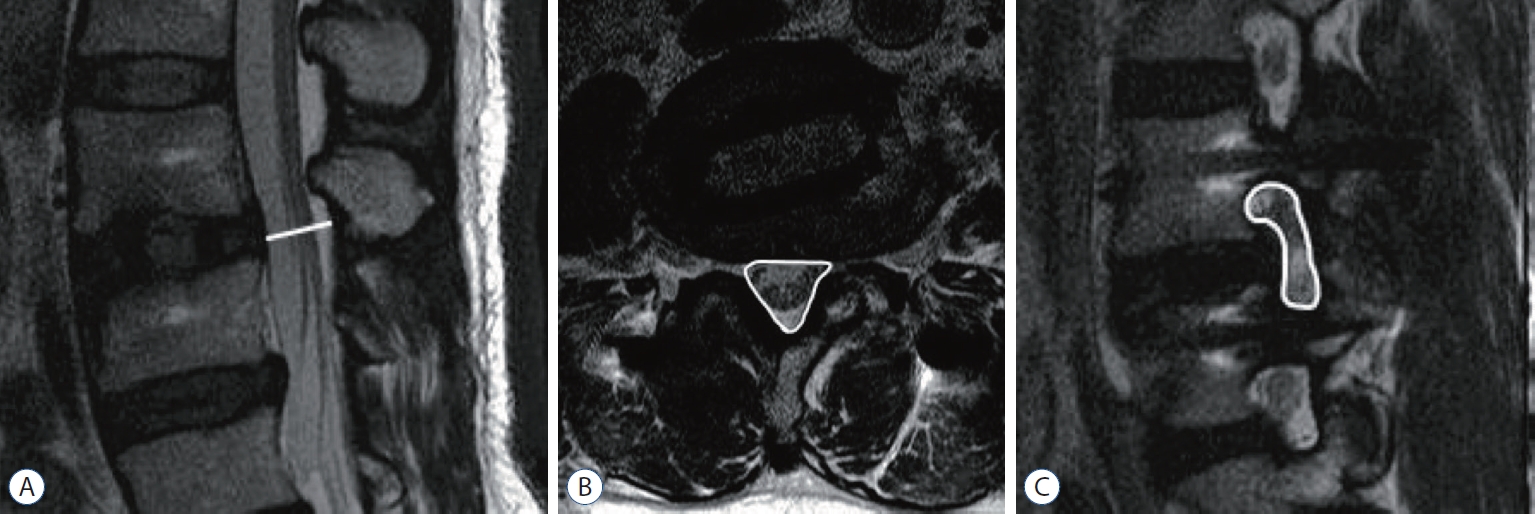
Fig. 4.
Flow chart of the patient cohort. TLIF : transforaminal lumbar interbody fusion, PLIF : posterior lumbar interbodyfusion. 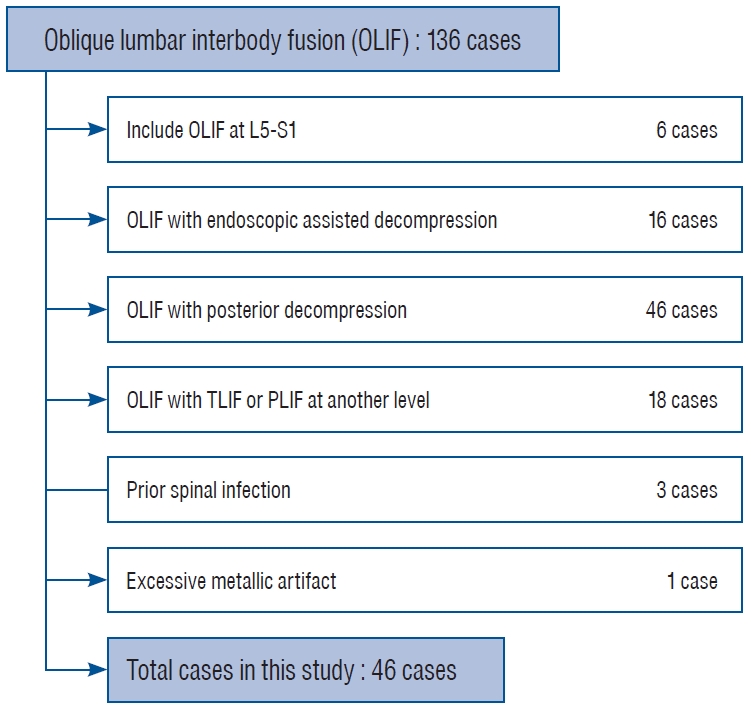
Fig. 5.
Linear regression show association between cage position and foraminal stenosis decompression (A) and segmental lordosis correction (B). 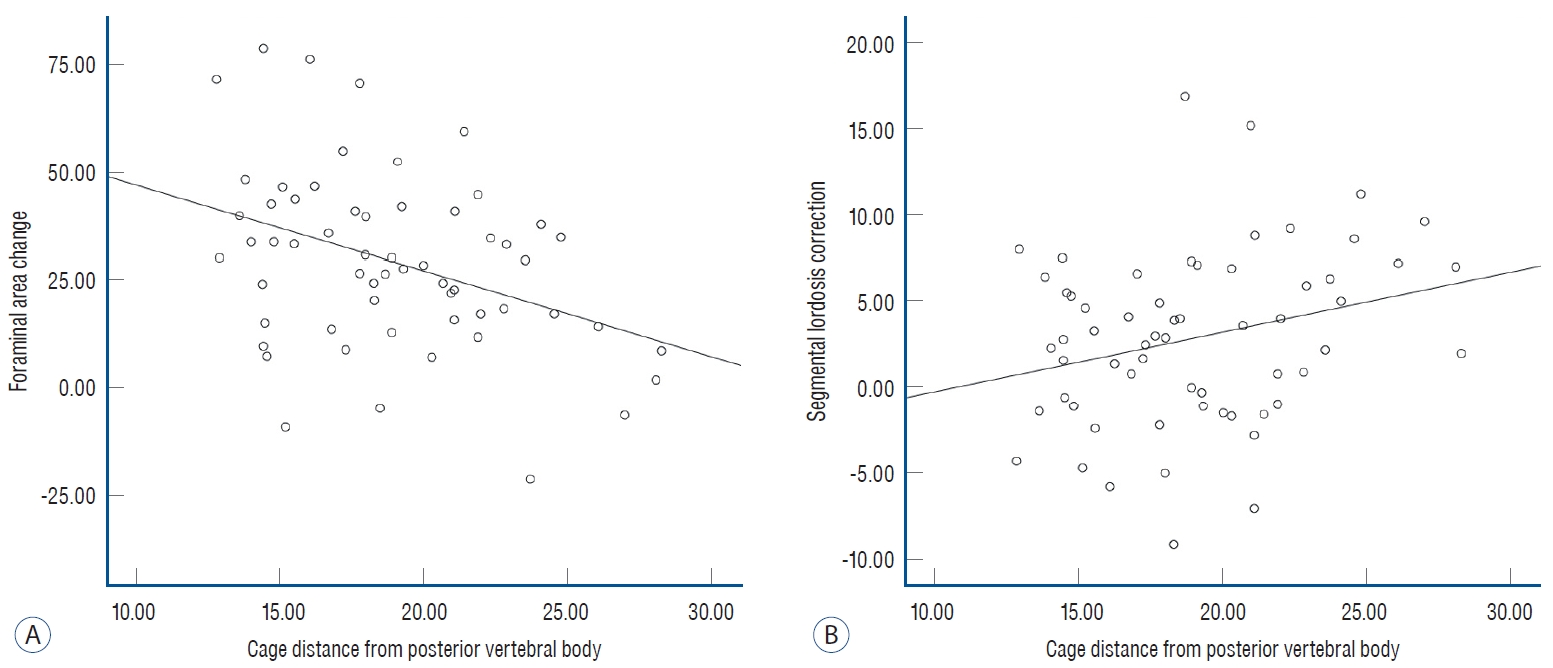
Table 1.
|
Parameter |
Value (n=46) |
|
Age (years) |
69.7±9.0 (49 to 88) |
|
Male/female |
17/29 |
|
Body mass index (kg/m2) |
24.8±4.0 |
|
Single level |
30 |
|
Multi-level |
16 |
|
2 level |
10 |
|
3 level |
6 |
|
Total operated level |
68 |
|
L2-3 |
15 |
|
L3-4 |
26 |
|
L4-5 |
27 |
|
Diagnosis |
|
|
Spondylolisthesis |
16 |
|
Adjacent segment disease |
8 |
|
Central canal and foraminal stenosis |
12 |
|
Foraminal stenosis |
7 |
|
Degenerative scoliosis |
3 |
Table 2.
Interbody cage configuration and position
|
Parameter |
Value |
|
Cage width |
|
|
18 |
55 |
|
22 |
13 |
|
Cage height |
|
|
8 |
1 |
|
10 |
25 |
|
12 |
35 |
|
14 |
7 |
|
Cage length |
|
|
45 |
25 |
|
50 |
34 |
|
55 |
9 |
|
Cage angle |
|
|
6 |
57 |
|
12 |
11 |
|
Cage distance (mm) |
19.0±3.9 |
|
Cage trajectory angle (degree) |
13.8±6.7 |
Table 3.
Clinical outcome after surgery
|
Preoperative |
Last follow-up |
Difference |
Change percentage |
p-value |
|
ODI |
51.1 (19.7) |
23.9 (17.8) |
27.9 (25.4) |
55.4 (34.7) |
<0.001 |
|
NRS back pain |
6.0 (2.0) |
2.0 (3.0) |
5.0 (4.0) |
75.0 (50.0) |
<0.001 |
|
NRS leg pain |
6.5 (3.0) |
2.0 (3.0) |
5.0 (4.0) |
71.4 (57.2) |
<0.001 |
Table 4.
Preoperative and postoperative imaging parameters
|
Preoperative |
Postoperative |
Difference |
p-value |
|
Radiographic parameters |
|
|
|
|
|
|
Anterior disc height (mm) |
7.2±2.5 |
11.5±1.9 |
4.3±2.6 |
<0.001 |
|
Middle disc height (mm) |
8.2±2.9 |
12.6±1.8 |
4.4±2.6 |
<0.001 |
|
Posterior disc height (mm) |
5.8±1.9 |
9.3±2.0 |
3.4±2.3 |
<0.001 |
|
Mean disc height (mm) |
7.1±2.0 |
11.1±1.4 |
4.0±1.9 |
<0.001 |
|
Foraminal height (mm) |
17.2±3.3 |
21.6±2.9 |
4.3±2.9 |
<0.001 |
|
Segmental lordosis (degree) |
7.0±6.9 |
9.9±6.0 |
3.0±5.1 |
<0.001 |
|
Lumbar lordosis (degree) |
32.8±14.2 |
39.2±12.9 |
6.5±6.9 |
<0.001 |
|
Slip percentage (%) |
8.1±7.3 |
3.8±4.5 |
4.3±5.2 |
<0.001 |
|
Coronal cobb’s angle (degree) |
4.0±3.7 |
1.6±1.7 |
2.4±3.5 |
<0.001 |
|
CT scan parameters |
|
|
|
|
|
Left foraminal height (mm) |
16.0±2.8 |
17.8±2.2 |
1.8±2.5 |
<0.001 |
|
Right foraminal height (mm) |
15.9±2.9 |
18.3±2.5 |
2.5±3.1 |
0.009 |
|
Left foraminal area (mm2) |
107.1±29.2 |
128.0±32.0 |
20.9±29.1 |
<0.001 |
|
Right foraminal area (mm2) |
109.8±28.7 |
126.9±27.4 |
17.1±22.4 |
<0.001 |
|
MRI parameters |
|
|
|
|
|
Spinal canal width (mm) |
7.8±3.1 |
10.1±3.1 |
2.2±2.0 |
<0.001 |
|
SCSA (mm2) |
105.2±51.0 |
142.9±57.8 |
35.7±27.5 |
<0.001 |
|
Left foraminal area (mm2) |
63.3±28.1 |
89.6±29.5 |
27.2±26.4 |
<0.001 |
|
Right foraminal area (mm2) |
62.0±25.4 |
91.0±29.5 |
28.2±24.8 |
<0.001 |
|
Foraminal stenosis grade |
|
|
|
<0.001 |
|
Grade 0 |
|
|
|
|
|
Left |
0 |
4 |
|
|
|
Right |
0 |
1 |
|
|
|
Grade 1 |
|
|
|
|
|
Left |
24 |
38 |
|
|
|
Right |
19 |
39 |
|
|
|
Grade 2 |
|
|
|
|
|
Left |
17 |
14 |
|
|
|
Right |
25 |
15 |
|
|
|
Grade 3 |
|
|
|
|
|
Left |
27 |
6 |
|
|
|
Right |
24 |
7 |
|
|
Table 5.
Linear regression analysis of the correlation between spinal canal cross-sectional area change and other factors
|
Single linear regression
|
Multiple linear regression
|
|
B |
SE |
p-value |
B |
SE |
Beta |
p-value |
|
Cage width |
1.89 |
4.99 |
0.70 |
|
|
|
|
|
Cage height |
2.50 |
5.90 |
0.67 |
|
|
|
|
|
Cage angle |
2.79 |
3.54 |
0.43 |
|
|
|
|
|
Cage distance |
1.61 |
2.13 |
0.45 |
|
|
|
|
|
Cage trajectory angle |
0.01 |
1.25 |
0.99 |
|
|
|
|
|
Anterior disc height gain |
6.63 |
2.92 |
0.027*
|
6.80 |
2.53 |
0.29 |
0.009*
|
|
Middle disc height gain |
-1.20 |
3.50 |
0.73 |
|
|
|
|
|
Posterior disc height gain |
-0.88 |
3.52 |
0.80 |
|
|
|
|
|
Preoperative SCSA |
-0.60 |
0.14 |
<0.001*
|
-0.61 |
0.13 |
-0.49 |
<0.001*
|
|
Spondylolisthesis reduction |
1.34 |
1.56 |
0.39 |
|
|
|
|
|
(Constant) |
|
|
|
82.65 |
18.60 |
|
<0.001*
|
Table 6.
Linear regression analysis of the correlation between foraminal area change and other factors
|
Single linear regression
|
Multiple linear regression
|
|
B |
SE |
p-value |
B |
SE |
Beta |
p-value |
|
Cage width |
-2.32 |
1.59 |
0.15 |
|
|
|
|
|
Cage height |
-2.36 |
1.89 |
0.22 |
|
|
|
|
|
Cage angle |
-1.24 |
1.14 |
0.28 |
|
|
|
|
|
Cage distance |
-2.00 |
0.64 |
0.003*
|
-1.69 |
0.61 |
-0.32 |
0.008*
|
|
Cage trajectory angle |
0.21 |
0.40 |
0.60 |
|
|
|
|
|
Disc height gain |
2.59 |
1.10 |
0.02*
|
1.99 |
1.05 |
0.221 |
0.06 |
|
Preoperative FA |
-0.30 |
0.11 |
0.007*
|
-0.24 |
0.11 |
-0.26 |
0.03*
|
|
(Constant) |
|
|
|
67.32 |
14.00 |
|
<0.001*
|
Table 7.
Linear regression analysis of the correlation between segmental lordosis change and other factors
|
Single linear regression
|
Multiple linear regression
|
|
B |
SE |
p-value |
B |
SE |
Beta |
p-value |
|
Cage width |
0.31 |
0.39 |
0.44 |
|
|
|
|
|
Cage height |
-0.15 |
0.47 |
0.75 |
|
|
|
|
|
Cage angle |
-0.03 |
0.28 |
0.92 |
|
|
|
|
|
Cage distance |
0.34 |
0.16 |
0.04*
|
0.30 |
0.14 |
0.24 |
0.03*
|
|
Disc height gain |
-0.40 |
0.27 |
0.15 |
|
|
|
|
|
Preoperative segmental lordosis |
-0.39 |
0.08 |
<0.001*
|
-0.38 |
0.08 |
-0.52 |
<0.001*
|
|
(Constant) |
|
|
|
-0.21 |
2.78 |
|
0.94 |
References
1. Castellvi AE, Nienke TW, Marulanda GA, Murtagh RD, Santoni BG : Indirect decompression of lumbar stenosis with transpsoas interbody cages and percutaneous posterior instrumentation. Clin Orthop Relat Res 472 : 1784-1791, 2014    2. Davis TT, Hynes RA, Fung DA, Spann SW, MacMillan M, Kwon B, et al : Retroperitoneal oblique corridor to the L2-S1 intervertebral discs in the lateral position: an anatomic study. J Neurosurg Spine 21 : 785-793, 2014   3. Fujibayashi S, Hynes RA, Otsuki B, Kimura H, Takemoto M, Matsuda S : Effect of indirect neural decompression through oblique lateral interbody fusion for degenerative lumbar disease. Spine (Phila Pa 1976) 40 : E175-E182, 2015   4. Jenis LG, An HS : Spine update. Lumbar foraminal stenosis. Spine (Phila Pa 1976) 25 : 389-394, 2000  6. Kepler CK, Sharma AK, Huang RC, Meredith DS, Girardi FP, Cammisa FP Jr, et al : Indirect foraminal decompression after lateral transpsoas interbody fusion. J Neurosurg Spine 16 : 329-333, 2012   7. Kim JS, Choi WG, Lee SH : Minimally invasive anterior lumbar interbody fusion followed by percutaneous pedicle screw fixation for isthmic spondylolisthesis: minimum 5-year follow-up. Spine J 10 : 404-409, 2010   8. Kim JS, Kang BU, Lee SH, Jung B, Choi YG, Jeon SH, et al : Mini-transforaminal lumbar interbody fusion versus anterior lumbar interbody fusion augmented by percutaneous pedicle screw fixation: a comparison of surgical outcomes in adult low-grade isthmic spondylolisthesis. J Spinal Disord Tech 22 : 114-121, 2009   9. Lang G, Perrech M, Navarro-Ramirez R, Hussain I, Pennicooke B, Maryam F, et al : Potential and limitations of neural decompression in extreme lateral interbody fusion-a systematic review. World Neurosurgery 101 : 99-113, 2017   10. Lee S, Lee JW, Yeom JS, Kim KJ, Kim HJ, Chung SK, et al : A practical MRI grading system for lumbar foraminal stenosis. AJR Am J Roentgenol 194 : 1095-1098, 2010   11. Limthongkul W, Tanasansomboon T, Yingsakmongkol W, Tanaviriyachai T, Radcliff K, Singhatanadgige W : Indirect decompression effect to central canal and ligamentum flavum after extreme lateral lumbar interbody fusion and oblique lumbar interbody fusion. Spine (Phila Pa 1976) 45 : E1077-E1084, 2020   12. Lin GX, Rui G, Sharma S, Mahatthanatrakul A, Kim JS : The correlation of intraoperative distraction of intervertebral disc with the postoperative canal and foramen expansion following oblique lumbar interbody fusion. Eur Spine J 30 : 151-163, 2021   13. Mayer HM : A new microsurgical technique for minimally invasive anterior lumbar interbody fusion. Spine (Phila Pa 1976) 22 : 691-699; discussion 700, 1997   14. Mehren C, Mayer HM, Zandanell C, Siepe CJ, Korge A : The oblique anterolateral approach to the lumbar spine provides access to the lumbar spine with few early complications. Clin Orthop Relat Res 474 : 2020-2027, 2016    15. Miscusi M, Ramieri A, Forcato S, Giuffrè M, Trungu S, Cimatti M, et al : Comparison of pure lateral and oblique lateral inter-body fusion for treatment of lumbar degenerative disk disease: a multicentric cohort study. Eur Spine J 27( Suppl 2):222-228, 2018  16. Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ : Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg 1 : 2-18, 2015   17. Nakashima H, Kanemura T, Satake K, Ishikawa Y, Ouchida J, Segi N, et al : Indirect decompression on MRI chronologically progresses after immediate postlateral lumbar interbody fusion: the results from a minimum of 2 years follow-up. Spine (Phila Pa 1976) 44 : E1411-E1418, 2019   18. Ohtori S, Orita S, Yamauchi K, Eguchi Y, Ochiai N, Kishida S, et al : Miniopen anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for lumbar spinal degeneration disease. Yonsei Med J 56 : 1051-1059, 2015    19. Oliveira L, Marchi L, Coutinho E, Pimenta L : A radiographic assessment of the ability of the extreme lateral interbody fusion procedure to indirectly decompress the neural elements. Spine (Phila Pa 1976) 35( 26 Suppl):S331-S337, 2010   20. Ozgur BM, Aryan HE, Pimenta L, Taylor WR : Extreme lateral interbody fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J 6 : 435-443, 2006   21. Park SJ, Lee CS, Chung SS, Kang SS, Park HJ, Kim SH : The ideal cage position for achieving both indirect neural decompression and segmental angle restoration in lateral lumbar interbody fusion (LLIF). Clin Spine Surg 30 : E784-E790, 2017   22. Rao PJ, Maharaj MM, Phan K, Lakshan Abeygunasekara M, Mobbs RJ : Indirect foraminal decompression after anterior lumbar interbody fusion: a prospective radiographic study using a new pedicle-to-pedicle technique. Spine J 15 : 817-824, 2015   23. Rauschning W : Normal and pathologic anatomy of the lumbar root canals. Spine (Phila Pa 1976) 12 : 1008-1019, 1987   24. Sato J, Ohtori S, Orita S, Yamauchi K, Eguchi Y, Ochiai N, et al : Radiographic evaluation of indirect decompression of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for degenerated lumbar spondylolisthesis. Eur Spine J 26 : 671-678, 2017   25. Sembrano JN, Horazdovsky RD, Sharma AK, Yson SC, Santos ERG, Polly DW Jr : Do lordotic cages provide better segmental lordosis versus nonlordotic cages in lateral lumbar interbody fusion (LLIF)? Clin Spine Surg 30 : E338-E343, 2017   26. Silvestre C, Mac-Thiong JM, Hilmi R, Roussouly P : Complications and morbidities of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lumbar interbody fusion in 179 patients. Asian Spine J 6 : 89-97, 2012    27. Singh V, Montgomery SR, Aghdasi B, Inoue H, Wang JC, Daubs MD : Factors affecting dynamic foraminal stenosis in the lumbar spine. Spine J 13 : 1080-1087, 2013   28. Woods KR, Billys JB, Hynes RA : Technical description of oblique lateral interbody fusion at L1-L5 (OLIF25) and at L5-S1 (OLIF51) and evaluation of complication and fusion rates. Spine J 17 : 545-553, 2017  
|
|