INTRODUCTION
Extensive soft tissue defects accompanied by infectious spondylitis are rare clinically. In these cases, medical/surgical therapy that involves debridement of the dead tissue and treatment with antibiotics can take a long time to carry out and a considerable length of time may elapse before the patient recovers, with this lengthy period of recovery adversely influencing the clinical outcome of patients. In addition, management of massive soft tissue defects and chronic wounds are major challenges. Various reports have proposed techniques of managing complex back wounds1,8,10). Published methods for treating the complex back wound of paraplegia patients are not specific and detailed enough to apply to general clinical practice6,14). It is even hard to find a case of a complex back wound of a paraplegic patient that is associated with a spinal infection in the literature. In this case, to treat the complex back wound that involved an extensive soft tissue defect associated with spinal infection, we tried a muscle flap technique that is mainly used in the plastic surgery field and not in neurosurgery in this hospital. The reverse latissimus dorsi muscle flap (RLDMF) was our final choice for this patient. This muscle flap technique allowed us to fill up the extensive soft tissue defect, thereby reducing the dead space, and maintain the paraspinal vasculature. The objective of this report was to evaluate the efficacy of filling up the defect using RLDMF in the treatment of severe infectious spondylitis. We observed that 6 months after the operation, the patient showed no sign of recurrence of infection and the back wounds had completely healed without any complication or sequela.
CASE REPORT
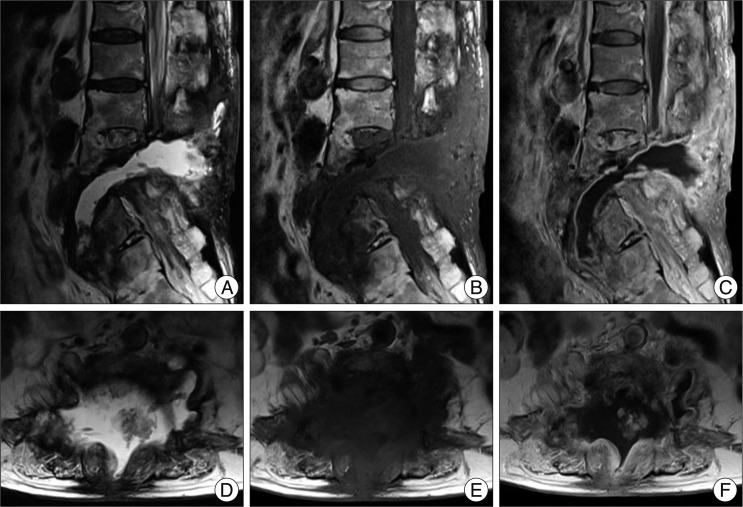
A 68-year-old woman with a previous history of paraplegia after traumatic spinal epidural hemorrhage from a ruptured L3 arteriovenous fistula (AVF) was admitted to our institute with high fever above 38в„ғ and severe back pain. About 10 days earlier, she suffered a superficial burn to her back and was admitted into the local hospital because of acute renal failure due to rhabdomyolysis. On neurologic examination, the patient was alert but mildly disoriented. Examination of the motor system revealed intact muscle strength in the upper extremity and flaccid paraplegia with areflexia. An examination of the sensory system revealed that all sensory modalities had decreased below the T10 dermatome level. An abdominal computed tomography scan demonstrated a suspicious pyogenic spondylitis of multiple lumbar spines with multiple perivertebral abscess formation and fluid collections around the pyriform muscles and parasacral area. A drainage catheter was inserted by a radiologist and the patient was admitted into the infectious diseases ward for antibiotic therapy. Empirical antibiotic therapy with ampicillin and sulbactam was started. On culture of aspirated fluid, methicillin-sensitive Staphylococcus aureus was identified. Thus, the antibiotic was changed to nafcillin. Drug fever developed after nafcillin was given, so the antibiotic was changed to cefazolin. This antibiotic was maintained until the culture of the draining catheter was identified. On culture of the draining catheter, methicillin-resistant Staphylococcus aureus and Pseudomonas aeruginosa were identified. Therefore, the antibiotic was changed to a combined vancomycin and ciprofloxacin regimen. After 14 days on that regimen, the antibiotic was changed to teicoplanin because the patient developed a skin rash. Despite conservative therapy using the appropriate antibiotics for 3 months and surgical drainage being performed twice, the spondylitis of her lumbar spine was not controlled. We thought that the fluid collection in the dead space between the intra-/inter-muscular area and the scar of the previously embolized AVF was the main source of infection recurrence (Fig. 1). We believed that by filling the dead space, we would be able to control the spondylitis. Therefore, we designed a staged operation.
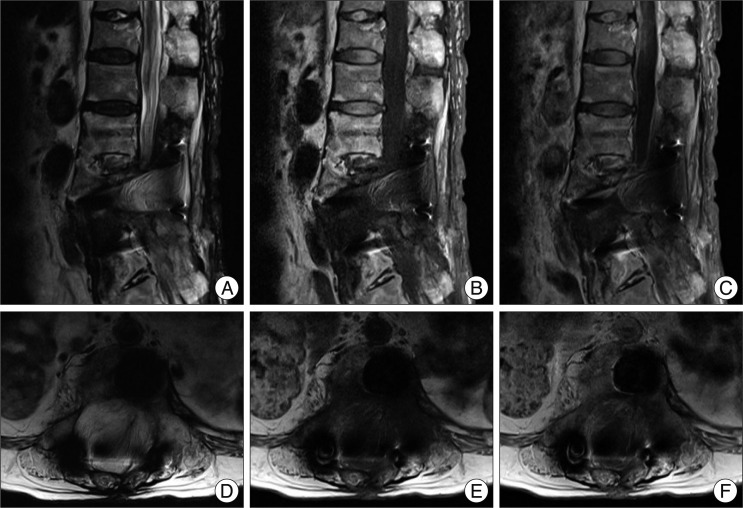
First, we performed multiple posterior screw fixations from L1 to the sacrum with wide debridement of infected soft tissue and obliteration of dead space using RLDMF (Fig. 2). Second, we performed anterior column reconstruction with an expandable mesh cage via an anterolateral reptroperitoneal approach to correct deformity and bone fusion. After the staged operation and antibiotic therapy, the multiple infectious spondylitis completely resolved without recurrence (Fig. 3) and there were no signs of spinal instability or pseudoarthrosis (Fig. 4).
DISCUSSION
Conservative management of pyogenic spondylitis is the traditionally used approach5). In certain pyogenic spondylitis cases, surgical treatment is strongly indicated, but invasive surgeries often cause various problems. When the patient's general condition is poor, less invasive treatment is required. The standard management of infectious spondylodiscitis with spinal epidural abscess has been surgical debridement with or without operative stabilization, followed by prolonged antibiotic treatment7). Nevertheless traditional surgical treatment for pyogenic spondylitis has the disadvantage of increased morbidity caused by the extensive exposure of the wound in the presence of infection. Unsuccessful conservative treatment may aggravate the disease course and also prolong hospital stay.
Percutaneous suction aspiration with drainage is another effective alternative for not only mild to moderate spondylodiscitis but also for early-stage pyogenic spondylodiscitis. Nagata et al.12), indicated that the main advantages of the technique were its reduced invasiveness compared with open surgery, and the almost immediate symptomatic relief it provided. Indications for this technique are considered to include the following : 1) no improvement in the condition of the patient despite use of antibiotic agents and immobilization for at least 1 month; 2) the presence of only a single affected intervertebral disc; 3) the location of the involved vertebra in the lower thoracic or lumbar spine; 4) the absence of any major neurological deficit; and 5) the absence of radiographically documented marked destructive changes in the affected vertebral body. But this treatment is not indicated in severe pyogenic spondylodiscitis in which abscess formation or marked bone destruction or extensive soft tissue defect is associated with a potential risk of neurological complications, such as existed in our case. In addition, the procedure failed to improve symptoms in one patient in whom marked destructive changes were apparent on radiography, and open surgery involving an implantation was necessary in that case.
In the presence of instrumentation, providing preemptive soft tissue reconstruction at the time of the initial spinal surgery can help minimize potentially serious wound complications. For management of wound complications that have developed, aggressive debridement and coverage with well-vascularized tissue can allow for expedient wound healing while maintaining stabilized instrumentation.
In extensive soft tissue defects accompanied by infectious spondylitis, such as in our case, the conventional approach using serial wound debridement and antibiotic administration could take a considerable period to complete, and is usually only successful in cases of mild infections. In more severe cases of infection with an extensive soft tissue defect, marked skin and muscle reactive fibrosis adjacent to the wound makes using paraspinous muscle flaps to close the defect difficult, if dissection is possible in the first place. Moreover, even if they can be dissected, they often are of insufficient volume to fill these wide and deep wounds. In this situation, pedicled latissimus dorsi muscle flaps have proven to be the most reliable method of treatment. Generally, the muscles of the back can be classified into 3 groups : superficial, intermediate, and deep groups. The superficial muscles such as the latissimus dorsi muscle are often valuable sources for a secondary flap in paraspinous muscle reconstruction as soft tissue defects are usually deep and extensive or require a skin island4). The pedicled latissimus dorsi flap proved to be a valuable and reliable tool to treat large and deep back wound infections with extensive soft tissue defects. It can be used as a musculocutaneous advancement or rotation flap when laterally based (thoracodorsal vessels), or as a muscular turnover flap, when medially based (paraspinous perforators). This versatility enabled the latissimus dorsi flap arc of rotation to reach midline spine defects from high thoracic through lower lumbar levels. And as the procedure is simple and the blood circulation stable during this operation, it is thought to be an effective reconstruction method for extensive soft tissue defects accompanied by infectious spondylitis.
It is true that literature has been published on methods of operative defect closure in the case of complex back wounds. However, since the data available is limited and the numbers of cases are relatively small in these studies, any comparison between the use of the pedicled latissimus dorsi flap and other methods such as the use of free flaps2,6), perforator flaps9), or tissue expansion13), combined methods3), paraspinous muscle flaps10) and superior gluteal muscle flaps15) are precluded. Use of the RLDMF, which was attempted in our patient, is a reliable method of treatment of infectious spondylitis with an extensive soft tissue defect11).