INTRODUCTION
Anterior cervical discectomy and fusion has been performed on patients with cervical degenerative disc disease for the past 50 years2). Because a thorough understanding of anatomy related to surgical approach is imperative to prevent catastrophic complications, surgeons should be aware preoperatively of the anatomical variations that can be found for the vertebral artery (VA), internal carotid artery, jugular vein, recurrent laryngeal nerve, and sympathetic nerve8,9).
Although injury to the VA is rare, it can lead to devastating clinical consequences, such as permanent neurological deficit or death7,10). Many variations in the VA have been reported3,10,13). The portion of the VA between the transverse process of C-6 and the transverse process of C-2 is called the V2 segment7,10). The incidence of an anomalous V2 segment including an abnormal VA entrance, a medial location of the VA, a tortuous VA, was described in 10% of cases3,15).
Because injury to the VA can be catastrophic, many authors have emphasized the importance of preoperative imaging including computed tomography (CT) angiography or magnetic resonance imaging (MRI)10,16,17). To improve surgical safety to the subaxial cervical spine, an awareness of variability in the V2 segment of the VA is critical for a surgeon.
Among the reports on anomalies of the V2 segment, few have described the medial loop of the VA3). Moreover, no study has focused on the clinical significance of the medial loop of the VA in the V2 segment and its impact on the cervical proximal root. Therefore, we studied the medial loop of the VA associated with the proximal cervical root in the V2 segment.
MATERIALS AND METHODS
We reviewed the case records from 1000 consecutive patients who had undergone MRI evaluation of the cervical spine between January 2005 and January 2008. Patients were included in the study if they had MRI axial images from C2 to C7 and sagittal MRI sections available. However, we excluded cases of bone erosion, a widened foramen at the medial loop of the VA, bony abnormalities, tumors displacing the VA or vertebral fractures. The widened foramen was defined that the axial area of the foramen with the medial loop of the VA was larger than the area of the contralateral foramen without the medial loop of the VA. When the VA causes erosion of the vertebral body or if there is a widened foramen with medial looping of the VA, the possibility of root compression could decrease. Therefore, the presence of erosion and of a widened foramen was added to the exclusion criteria. There were 598 male and 402 female patients enrolled; ranging in age from 10 to 96 years (mean 51.4┬▒13.96).
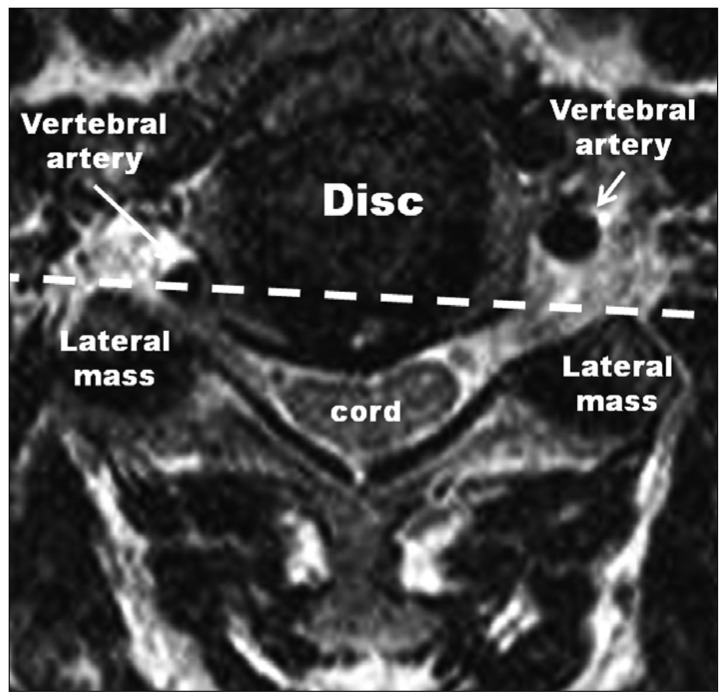
The medial loop of the V2 segment that caused cervical proximal root compression was defined from the following radiological criteria : over a third of the axial aspect of the VA located in the intervertebral foramen was inside the line between the most ventral points of the bilateral lateral mass, and the ipsilateral proximal root was deviated dorsally by the medial loop of the VA (Fig. 1). Cases in which there was bone erosion or a widened foramen caused by the medial loop of the VA was excluded.
The medical records of all cases satisfying these radiological criteria were reviewed and we evaluated the cervical radiculopathy corresponding to the presence of a medial loop of the VA.
RESULTS
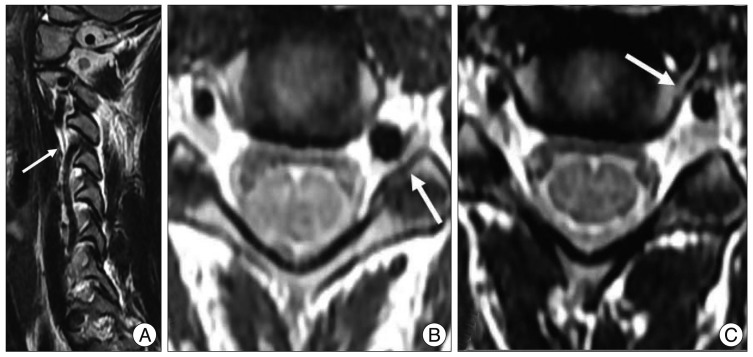
In six patients (0.6%), the VA formed a medial loop causing proximal cervical root compression (Table 1). Only one patient (Case 1) had been involved in a minor road traffic accident, after which she began to experience a tingling sensation in the left arm. On neurological examination, there was a sensory disturbance in the left C4 dermatome associated with a positive Spurling sign. An MRI scan was performed revealing a medial VA loop without an enlarged foramen. This had compressed the C4 root because of a tortuous VA on the left side (Fig. 2). The patient had experienced no previous symptoms related to the cervical lesion and complained of a tingling sensation of less than 4 points on a visual analogue scale. Therefore, physiotherapy and therapy with non-steroid anti-inflammatory agents were started. The patient stopped complaining of the tingling sensation in the left arm at the second follow-up visit 2 weeks after therapy initiation. On follow-up 3 months later, there was no symptom related to the cervical spine.
The other five cases with a medial loop of the VA had no related symptoms such as equilateral cervical radiculopathy (Fig. 3). All five cases (83%) had a left-sided medial loop. In Case 5, the VA with a medial loop was the dominant artery and other cases did not have a dominant artery. In three cases (Case 1, 3 and 5), the medial loops were located at the level of C3-4 : in two cases, it was at C4-5 and in one case it was at C5-6.
DISCUSSION
The medical literature mentions several anatomical variations in the VA3,12,14). An abnormal course of the VA can cause vessel injury related to serious consequences during cervical surgery. Therefore, authors have emphasized that preoperative MRI or CT scans should be conducted to avoid inadvertent tearing during an anterior or lateral approach to the cervical spine3,10). Abnormal levels of entrances of the VA into the C3, C4, C5 and C7 vertebrae and medial loops of the VA, with and without bony erosion were typical abnormalities at the V2 segment1,3,12,13,15). The incidence of an abnormal entrance of the VA was reported in 5-7% of cases13).
The V2 portion of the VA is relatively straight and it is usually located in the extraforaminal area. The medial loops of the VA can course ventromedially to the vertebral body and can develop medially and laterally to some degree, without direct contact with the cervical root3). However, when the degree of looping becomes more convoulted, a tortuous vessel could form at the V2 segment with or without enlargement of the transverse foramen, erosion of the vertebral body, or root compression3,5,6). There are a few reports on a medial loop of the VA and the incidence ranged between 2.0 and 5.6%3,10). In the present study, the incidence (0.6%) was less than in other reports. This was because we excluded cases with bony erosion or an enlarged foramen caused by the VA and included one case with proximal root compression. One report related to anatomical variations of the VA stated that the incidence of a medial loop of the VA protruding into the proximal part of the intervertebral foramen was 0.8%3). Reports based on cadaveric and imaging studies only emphasized the importance of preoperative investigations and only two reports described spontaneous cervical radiculopathy4,11). However, none of the cases in the present study developed symptoms spontaneously. Case 1 had radiculopathy that developed after minor trauma. In axial MRI images, the medial loop of the VA was located in the proximal portion of the foramen and caused compression of the cervical root. The lesion did not cause spontaneous cervical radiculopathy in the present study. This was probably because the VA could not exert a strong pulsatory effect on the proximal root and there might be a remaining space for the root based three-dimensional constructions. In two other reports with cervical radiculopathy associated with the medial loop of the VA, the symptoms were treated with either conservative or surgical approaches4,11). In the present study, the cervical radiculopathy was resolved after conservative treatment.
It is more effective to investigate the foraminal area in oblique images than that in sagittal images. Therefore, a future study will use this approach. It will also be necessary to reveal any concordant radiculopathy using nerve conduction studies. Based on this and the other aforementioned cases, the medial loop of the VA might be a cause of cervical radiculopathy. In future studies, we should use three-dimensional CT scans of the foramen of the cervical spine for evaluating the VA.
CONCLUSION
It is rare that the medial loop of the VA in the V2 segment causes compression of the proximal cervical root without leading to bony erosion and an enlarged foramen. Thus, the presence of a medial loop of the VA might lead to cervical radiculopathy and requires critical consideration during surgery.