INTRODUCTION
Spinal schwannomas are benign tumors arising from the sheath of the spinal nerve roots and occasionally occur in the cauda equina. Tumors in the cauda equina often attain considerable size without painful symptoms, because of the mobility of the roots and the wide intradural space2). Giant schwannomas of the cauda equina that involve many nerve roots are rare2,6). Those that occur, however, are usually observed in an intrasacral region, and are rarely ossified6,17). We describe here an unusual case of giant schwannoma of the cauda equina with dystrophic calcification, which was completely removed without any neurological deterioration.
CASE REPORT
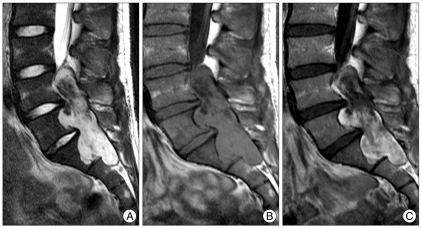
A 21-year-old man presented with a 12-month history of urinary dysfunction and numbness over the buttocks and posterior thigh area. Because of aggravation of the numbness, he was first examined at a military hospital. A cauda equina tumor was suspected, and the patient was referred to our institution. Neurological examination revealed hypesthesia below the buttocks, but motor function was intact. Urodynamic examination and anal sphincter manometry showed mild functional impairment. Plain radiography demonstrated scalloping of the posterior surface of the vertebral bodies from L4 to the sacrum. An increased in the intrapedicular distance at L4-L5 was also noted. Magnetic resonance (MR) imaging showed a giant cauda equina tumor extending from L4 to the sacrum, with extension into the left L5-S1 and S1-S2 neural foramina. The tumor showed low signal intensity on T1-weighted images, a high signal intensity on T2-weighted images, and enhancement on gadolinium-enhanced T1-weighted images (Fig. 1). The preoperative diagnosis was a benign giant cauda equina tumor. Computed tomographic (CT) scan showed a large calcified mass in the enlarged spinal canal and neural foramen (Fig. 2). CT-guided needle biopsy of the sacrum showed that the mass was a benign mesenchymal tumor.
The patient underwent surgery with monitoring using free-running and triggered electromyogram (EMG) of the tibialis anterior, gastrocnemius, abductor hallucis, and anal sphincter muscle. Following a posterior midline incision, a laminoplastic laminotomy of L3-L5 and a laminectomy at S1-S2 were performed. The sacral laminae were thin and adherent to the dura matter. The tumor was located primarily in the extradural space, and dystrophic calcification was observed within the mass (Fig. 3). The tumor, dura matter, and nerve roots could be separated, although the spinal nerve roots involved in the tumor were paper-thin. Because the nerve root corresponding to the tumor origin could be defined, the tumor was totally resected, with monitoring of non-functioning nerve roots using both free-running and triggered EMG. The posterior surfaces of the vertebral bodies were deeply eroded, but the dura matter was intact and covered the surface of the eroded vertebral bodies. The resected laminae were fixed by insertion of miniplates and screws. Because the patient had good bone quality and a stable vertebral column, further spinopelvic reconstruction was not performed. Histologic examination of the resected tumor revealed that it was a schwannoma. Total operating time was 6 hours and blood loss was estimated to be 750 mL.
The postoperative course was uneventful and the patient experienced significant relief of urinary dysfunction. Sensation and sphincter function gradually improved. After one week of bed rest, the patient was permitted to walk using a hard brace and walker. At the most recent follow-up, his urinary and anal sphincter dysfunction almost disappeared, and the hypesthesia in both buttocks was mild. He walks smoothly without a cane or any aid. MR and plain imaging 3 years after surgery showed no evidence of any residual tumor, vertebral fracture, or instability (Fig. 4).
DISCUSSION
Giant schwannomas of the cauda equina of the spinal canal, with pedicle erosion and/or widening of the neural foramen, have been described6,10,14,15). However, because of dystrophic calcification, an accurate preoperative diagnosis was difficult in the present patient. Scalloping of the posterior surface of the vertebral bodies strongly suggested a disease of long-standing etiology. Although we suspected that the symptoms were attributable to a slow-growing tumor, such as a schwannoma, such tumors are rarely calcified or ossified. Thus, these situations led us to perform CT-guided needle biopsy. Our preoperative differential diagnoses included ganglioneuroma and schwannoma of the ancient type, both of them are benign mesenchymal tumors.
By searching the English language literature using the terms 'schwannoma', 'cauda equina', 'giant', and 'tumor' since 1960, we identified reports describing 29 patients with giant cauda equina schwannomas. After excluding five patients, four with malignant peripheral nerve sheath tumors and one without enough clinical information, 24 patients remained, including the patient described here. Table 1 summarizes data on patients with giant schwannoma of the cauda equina1,4,6,10,14,17,19), including seven with intrasacral schwannoma8,9,11,13,15,16,18) and one with intraosseous schwannoma3) arising from nerves within bones. Only one patient with a giant cauda equina schwannoma associated with a small ossification has been reported to date6). Thus, to the best of our knowledge, a giant schwannoma in the cauda equina accompanied by dystrophic calcification has not been previously reported.
Complete excision, taking care not to damage nerves, is the recommended treatment for such locally aggressive benign tumors, as partial resection carries a risk of local recurrence and re-operation is much more difficult and dangerous than the primary operation4,14,16). However, tumors located in the lumbar spine region are usually incompletely excised because complete removal may risk the sacrifice of many nerve roots5). An earlier review found that complete excision of such tumors frequently results in neurologic deterioration6). In contrast, others have reported that the involved nerve roots were nonfunctional at the time of surgery and that the risk of neurologic deficit after sacrifice of such these roots was thus small2,4,7). Although the tumor described here was extensive in size, it involved only two nerve roots, which were shown to be non-functional at the time of surgery by both free-running and triggered EMG. This tumor could therefore be completely excised, with sacrifice of the (non-functional) roots giving rise to the tumor.
Giant schwannoma of the cauda equina often results in considerable vertebral erosion12). In some previous reports, spinal fusion with instrumentation was performed after resecting a giant schwannoma to prevent vertebral fracture4,6). We found that one-third of reported patients who underwent complete removal of giant schwannomas of the cauda equina required spinal reconstruction because of spinal instability. The patient described here had good bone quality, with a stable vertical column, and required only a laminoplasty using miniplates and screws. Moreover, the patient requested less invasive surgery. Fortunately, no vertebral fracture or instability has been seen in to three years postoperatively.