Cho and Chang: Survival and Recurrence Rate after Treatment for Primary Spinal Sarcomas
Abstract
Objective
We have limited understanding on the presentation and survival of primary spinal sarcomas. The survival, recurrence rate, and related prognostic factors were investigated after treatment for primary sarcomas of the spine.
Methods
Retrospective analysis of medical records and radiological data was done for 29 patients in whom treatment was performed due to primary sarcoma of the spine from 2000 to 2010. As for treatment method, non-radical operation, radiation therapy, and chemotherapy were simultaneously or sequentially combined. Overall survival (OS), progression free survival (PFS), ambulatory function, and pain status were analyzed. In addition, factors affecting survival and recurrence were analyzed : age (≤42 or ≥43), gender, tumor histologic type, lesion location (mobile spine or rigid spine), weakness at diagnosis, pain at diagnosis, ambulation at diagnosis, initial treatment, radiation therapy, kind of irradiation, surgery, chemotherapy and distant metastasis.
Results
Median OS was 60 months, the recurrence rate was 79.3% and median PFS was 26 months. Patients with distant metastasis showed significantly shorter survival than those without metastasis. No factors were found to be significant relating to recurrence. Prognostic factor associated with walking ability was the presence of weakness at diagnosis.
Conclusion
Primary spinal sarcomas are difficult to cure and show high recurrence rate. However, the development of new treatment methods is improving survival.
Key Words: Primary spinal sarcoma · Survival · Recurrence · Prognosis.
INTRODUCTION
Sarcomas are a family of malignant tumors that arise from connective or mesenchymal tissue. Primary spinal sarcomas arise from the spine itself, usually from a structural component such as bone or cartilage 18). Their incidence is very rare. According to the American Cancer Society, they account for less than 5% of all osseous neoplasms, and less than 0.2% of all cancers 24,25). Dorfman and Czerniak 9) analyzed data on 2627 primary malignant tumors of bone including spine collected in the Surveillance, Epidemiology, and End Results (SEER) program. Their tumors were osteosarcoma (35.1%), followed by chondrosarcoma (25.8%), Ewing's sarcoma (16.0%), chondroma (8.4%), and malignant fibrous histiocytoma (MFH) (5.6%). These tumors can cause significant morbidity and mortality secondary to local invasion and destruction of adjacent structures including bone, nerves, and vascular structures, and they can metastasize to distant organs 19,24). Tremendous advancement has been made in the surgical and medical therapy of malignant primary bone tumors 19,27,34), but their spinal involvement is still associated with poor prognosis 17,22). The understanding of the epidemiology of primary spinal sarcomas has been limited to small case series and controlled trials in the treatment were impossible because of their rarity 23). These facts resulted in non-uniform approach in the treatment of the spinal sarcomas 16,27). And, a general understanding of the presentation and survival of primary spinal sarcomas is also lacking 39). For this reason the establishment of a bone tumor registry provides a valuable source of information and facilitates reasonable treatment of these tumors 16,28). It was known that primary sarcomas of the spine had low survival and high recurrence rate compared to sarcoma occurring in extremity 2,8,22,24,31,37,41). The radical or wide excision is required in sarcoma treatment, but it is difficult to perform the radical excision due to the risk of neural or vascular injuries 7,19). In addition, high dose radiation cannot be delivered to residual mass, because it may produce radiation-induced spinal cord injury 3,5,16). The purpose of this study is to investigate the survival and recurrence rate of primary spinal sarcoma patients who underwent non-radical surgery plus adjuvant therapy or nonoperative treatments. Also, prognostic factors affecting survival, recurrence, and ambulatory function were analyzed.
MATERIALS AND METHODS
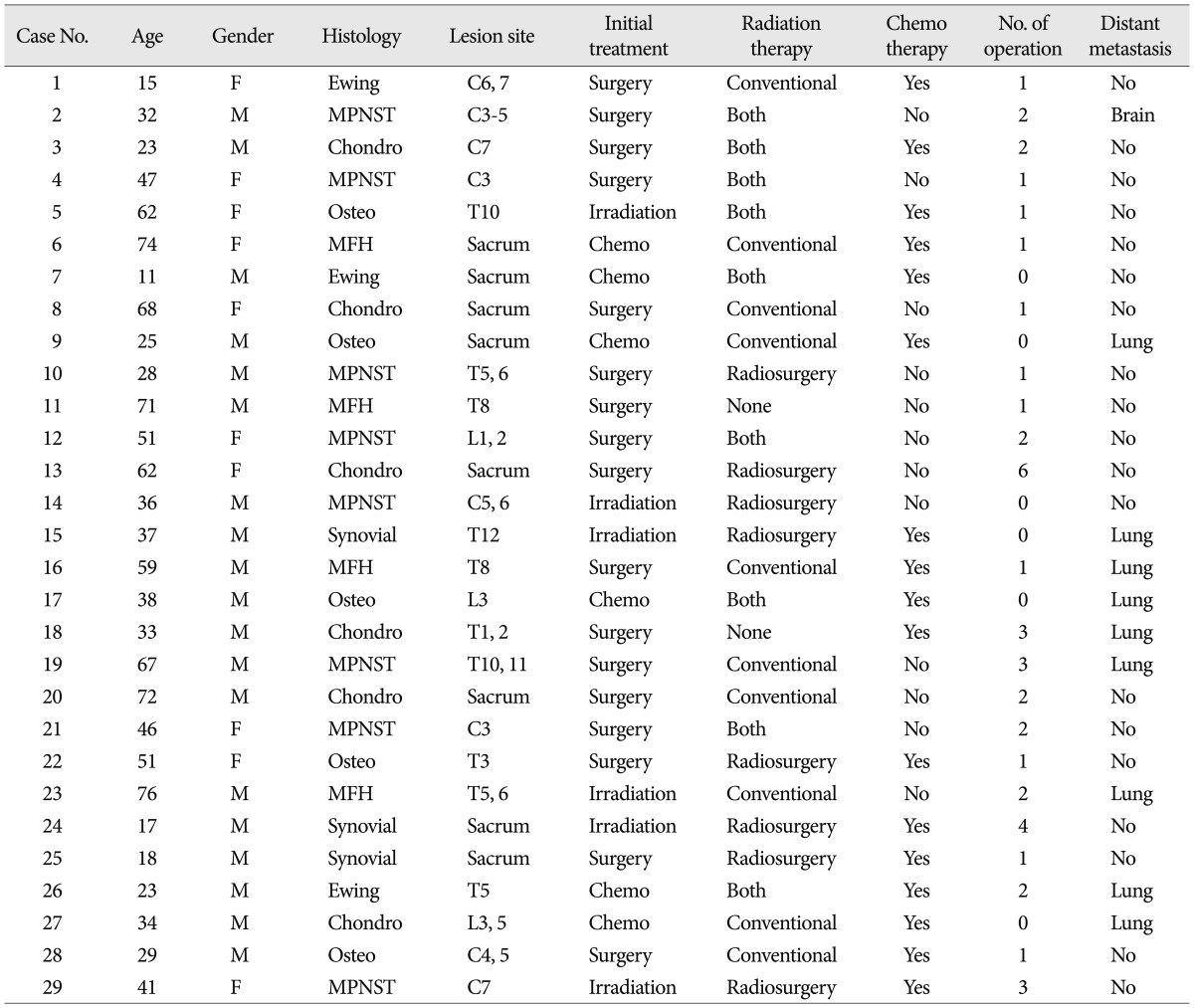
Study cohort was the patients who were treated in our hospital due to primary spinal sarcomas from January 2000 to December 2010. The total number of patients was 29, and their medical records and radiologic images were analyzed retrospectively. The number of male patients was 19 and that of female patients 10. The average age of patients was 42.9 years old (range, 11 to 76 years). With regard to tumor histology, malignant peripheral nerve sheath tumor (MPNST, 8 patients) was the most prevalent, and other tumors included chondrosarcoma (6 patients), osteosarcoma (5 patients), MFH (4 patients), Ewing sarcoma and synovial sarcoma (each 3 patients). Regarding lesion location, 21 patients had a tumor on mobile spine (8 lesion in cervical, 10 in thoracic and, 3 in lumbar spine), while 8 patients had a tumor on rigid spine (sacrum). With regard to the lesion multiplicity, 17 patients had a single lesion where the tumor was confined to one segment at diagnosis, and 12 patients had multiple level involvement. Ten patients showed distant metastasis during follow-up, and 3 patients had metastasis at diagnosis. The time for the development of distant metastasis was, on the average, 24 months. The site of distant metastasis was lung in 9 patients and brain in one patient. Demographic data in our study cohort were summarized in Table 1. Twenty-seven patients complained of pain and 14 patients had motor weakness at the time of diagnosis. Twenty-six patients could walk at diagnosis, and 15 patients could walk also at the last follow-up. Among 14 patients who could not ambulate, 10 patients could not walk due to neurologic deficit and remaining 4 patients could not walk due to intractable pain. The period for which ambulatory function was maintained was average 46 months, 13 patients could walk longer than 46 months, whereas 16 patients shorter than 46 months.
In initial treatment, surgery was chosen in 17 patients, irradiation in 6 patients, and chemotherapy in 6 patients. A total of 23 patients received the surgical treatment during the follow-up. Operations were performed 44 times in a total of 23 patients and 12 patients received the surgery two or more times. As for surgical procedure, all the operations were subtotal or partial removal of tumors, not radical excision. Adjuvant treatments were conducted after subtotal removal. Complications related to surgery occurred in 7 cases. There were 4 cases of wound infection, one case of screw malposition, one case of hypoglossal nerve palsy, and one case of pulmonary complication. Every patient recovered from these complications without sequelae. As for radiation therapy, 27 patients received radiation therapy (RT) during the treatment period. Conventional RT was given to 10 patients, 8 patients received stereotactic radiosurgery, and 9 patients received both of them. Anticancer chemotherapy was performed in 17 patients.
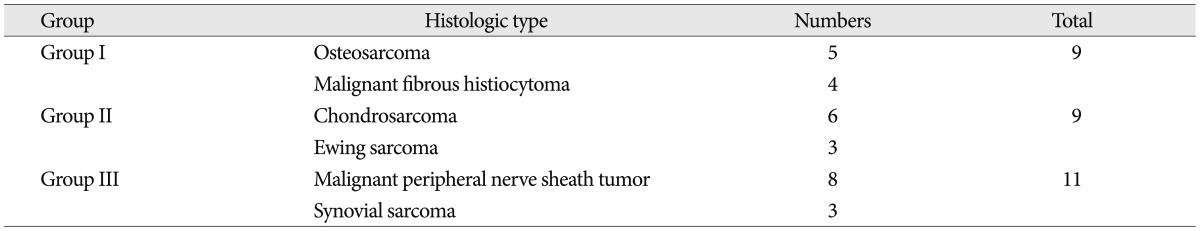
Tumor was classified into 3 groups based on the histologic types ( Table 2). Osteosarcoma and MFH, being known to have similar clinical behavior, belonged to first group (group I). Ewing' sarcoma and chondrosarcoma which were reported to have long survival belonged to the second group (group II). The remaining MPNST and synovial sarcoma were included into the third group (group III). In this study, we sought to determine overall survival (OS) and progression free survival (PFS) in primary sarcoma of spine, and to document pain level changes and ambulatory status during follow-up. Thirteen prognostic factors affecting survival, systemic recurrence and ambulatory function were analyzed : age (≤42 or ≥43), gender, tumor histologic type (osteosarcoma and MFH, or Chondrosarcoma and Ewing sarcoma, or MPNST and synovial sarcoma), lesion location (mobile spine or rigid spine), weakness at diagnosis, pain at diagnosis, ambulation at diagnosis, initial treatment method, radiation therapy, kind of irradiation, surgery, chemotherapy and distant metastasis.
Survival analysis was performed by using the log-rank test. Survival curves were created by using the Kaplan-Meier life-table analysis. Chi-square and Fisher exact tests were used for categorical variables and Student's t test were used for continuous and ordinal variables, as appropriate. A p value 0.05 (two-tailed) was considered significant. The data were compiled and analyzed with the software package SPSS, version 14.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
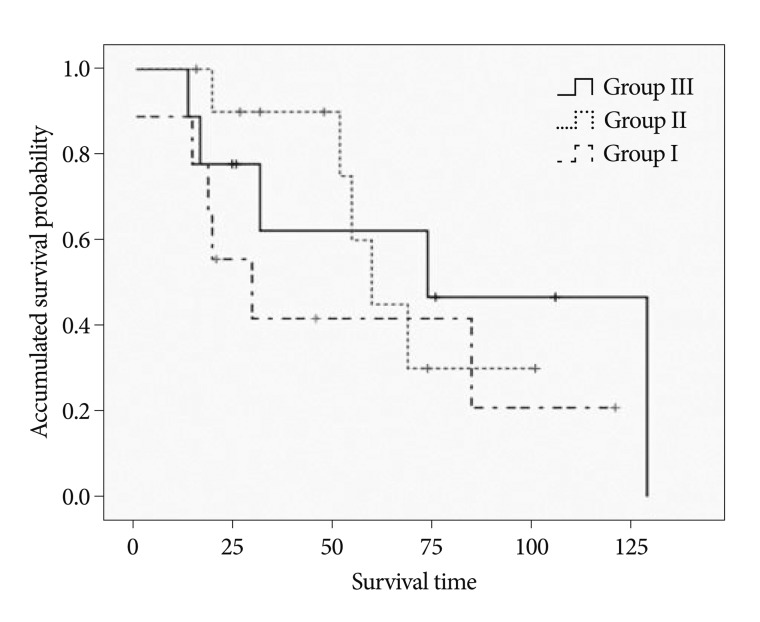
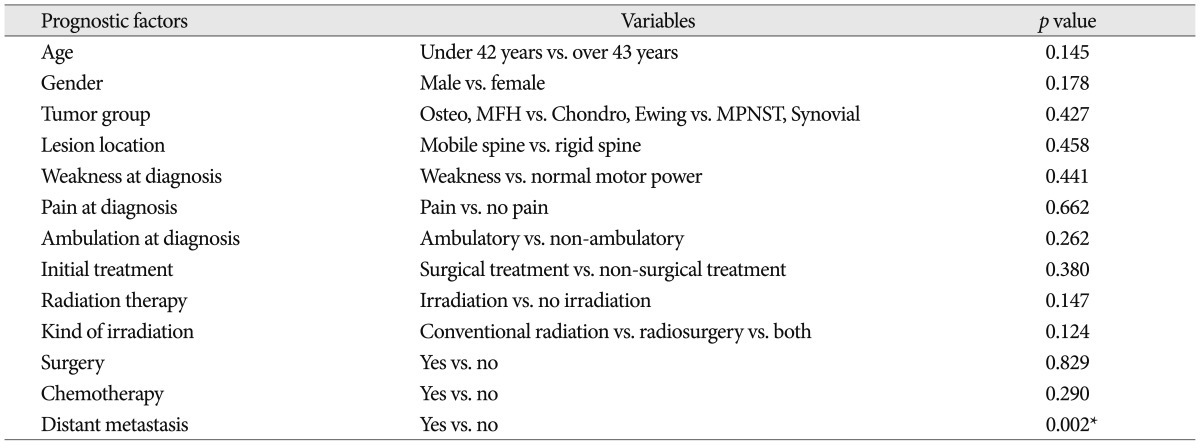
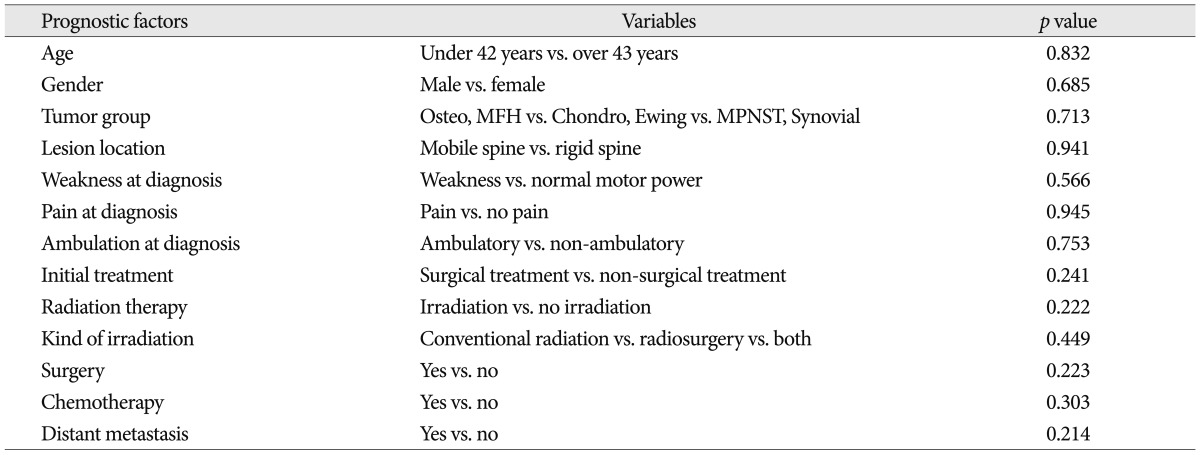
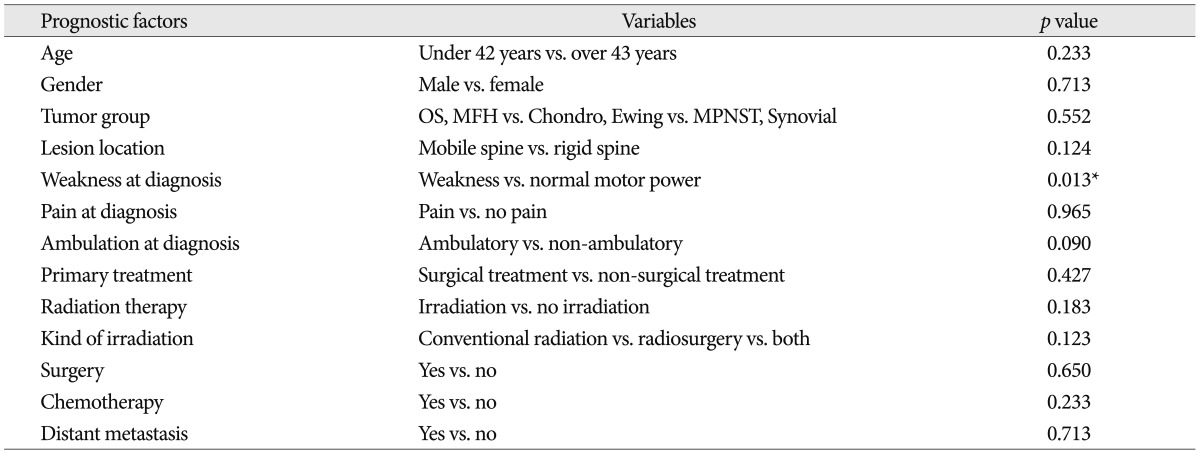
Median of OS in the study cohort was 60 months [95% confidence interval (CI), 33.17-86.83 months]. The OS was different depending on the histologic type ( Fig. 1). Osteocarcoma and MFH group showed the shortest survival of 30 months (95% CI, 5.59-54.40 months). In group II (MPNST and synovial sarcoma group) median survival was estimated to be 60 months. Ewing sarcoma and chondrosarcoma group, which was known to have the longest survival, showed median survival of 74 months (95% CI, 16.07-131.93 months). However, there was no statistical significance among three groups. Among total 29 patients, 13 patients were alive at the last follow-up and 16 patients died. Fourteen patients died of the disease progression and two patients the medical condition unrelated to tumor progression such as sepsis or acute renal failure. Statistically significant prognostic factors associated with survival were the presence of distant metastasis ( Table 3). The patients with distant metastasis, whose median survival was 30 months (95% CI, 7.23-52.77 months) showed significantly shorter survival than the cases without metastasis whose median survival was 85 months (95% CI, 57.29-112.71 months; p=0.002) ( Fig. 2). Twenty-three out of 29 patients experienced the recurrence during the follow-up. The recurrence rate was 79.3% on follow-up. The recurrence implies not only the local recurrence at the tumor site but also the systemic recurrence including the distant metastasis. PFS of patients was 26 months (95% CI, 14.09-37.91 months). After 26 months, the recurrence or progression was shown in most patients. There were no statistically significant prognostic factors associated with recurrence ( Table 4). Among 27 patients who complained of pain at the time of diagnosis, pain improvement was achieved in 23 patients after the treatment. No change in pain score was seen in remaining four patients. Pain status was evaluated with visual analogue scale (VAS). Pain was determined to be controlled when post-treatment VAS decreased by more than two points or the amount of pain medication was reduced. At initial diagnosis, mean value of VAS was 8.44±1.25 points before treatment. Mean VAS fell to 4.56±2.10 points after the treatment with 3.89±2.08 point decrease (p=0.001). Pain score of patients who underwent the surgical treatment was measured upon the first follow-up after the surgery. Pain score of patients who received non-surgical treatments was measured within a month upon the completion of initial treatment. Likewise, pain was reduced after the initial treatment, but the pain increased again with recurrence after 27 months. There were no statistically significant prognostic factors associated with the pain control.
As a whole, median period during which ambulatory function was maintained was 54 months (95% CI, 43.33-104.67 months). Statistically significant prognostic factor associated with post-treatment ambulatory function was the presence of weakness at initial diagnosis ( Table 5). Among patients who did not show motor weakness at initial diagnosis, patients who maintained the walking ability at the last follow-up were 86.7%, which is twice as much as patients who had weakness at initial diagnosis (42.9%) ( p=0.013) ( Fig. 3).
DISCUSSION
Treatments for primary spinal sarcomas involve a multi-modality approach consisting of surgery, radiation therapy and chemotherapy 12,30). The experience in the treatment of extremity sarcomas have been applied to cases of spinal sarcomas 3). Although great advances have been achieved in the treatment, oncological outcome in spinal sarcomas is worse than that of soft tissue sarcomas in extremities 20,33,40). In extremity sarcomas, many reports on survival and recurrence are available 2,31,36,37). Vasileios et al. 37) reported that 5-year survival rate of MFH patients was 66% and the recurrence and the metastasis rates were 31%. Tural et al. 36) reported that the recurrence rate was 23% and 5-year survival rate was 72% through retrospective study of adult Ewing sarcoma patients. According to Stanelle et al.' 31)s paper, it was reported that 73% of 5-year survival rate, 65% of 10-year survival rate in synovial sarcoma and 41% of recurrence rate of this disease. Arndt et al. 2) reported 65% of 5-year survival rate in osteosarcoma. In our study, 5-year survival rate was 41%, 61% and 45% in osteosarcoma/MFH group, chondrosarcoma/Ewing sarcoma group and MPNST/synovial sarcoma group, respectively. These data show the outcome is better in extremity sarcomas than in spinal sarcomas. Since primary spinal sarcomas are very rare diseases 24,25), the standard treatment method has not been established 28,34,38,39). However, treatment for osteosarcoma and chondrosarcoma is being conducted in uniform fashion. In cases of osteosarcoma, preoperative chemotherapy and radical surgery is usually performed 1,2,4,5). Preoperative chemotherapy enables the tumor size to be reduced. Postoperative adjuvant chemotherapy is sometimes done when indicated. In chondrosarcoma, chemotherapy or radiation therapy is rarely indicated and the sole effective treatment is operative resection 14,15,21,32). Improvement in surgical approach to the entire vertebral column has made it technically feasible to resect tumors involving the spine at all levels, and the development of new instrumentation systems has enabled surgeons to reconstruct entire vertebral segments after resection 27,34). But, the proximity of the dural sac, aorta, vena cava, and esophagus makes it difficult to achieve adequate negative surgical margins 19). The en bloc resection of a spinal segment is a relatively recent concept, which is different from a complete piecemeal corpectomy 7). It is recognized that, with rare exceptions, the rate of local recurrence depends on the adequacy of the resection, even when adjuvant therapy is used 6,20,28,39). The histological types of sarcomas were identified and confirmed by a pathologist at M.D. Anderson Cancer Center. Soft tissue sarcomas were further dichotomized as either high (G2) or low (G1) grade according to the classification of Enneking et al. 10) Low-grade tumors are well differentiated, have few mitoses, and moderate cytologic atypia. High grade lesions are characterized by poor differentiation, a high cell/matrix ratio, and a high mitotic rate, necrosis, and microvascular invasion 1,2,34,41). Tumor growth and progression are variable depending on the differences in the grade of differentiation. In addition, these histological differences produce the differences in the susceptibility to radiation and the reactivity to chemotherapy, and affect the selection of adjuvant treatment. Therefore, it is thought that survival rate is various depending on histologic type. A number of studies have attempted to identify prognostic factors for survival in primary sarcomas of the spine 8,22,23). Damron et al. 8) investigated the survival and epidemiologic data from the National Cancer database of the American College of Surgeons. Their data included both extremity and spinal sarcomas. They reported that 5-year survival rate was 53.9% for osteosarcoma, 75.2% for chondrosarcoma, and 50.6% for Ewing's sarcoma. Mukherjee et al. 24) analyzed overall survival and prognostic factors affecting survival time in malignant primary osseous spinal tumors. They searched the SEER database to identify all registered cases of Ewing sarcoma, osteosarcoma and chondrosarcoma to assess histology specific survival during the period from 1973 to 2003. Total study patients were identified as 579 with chondrosarcomas, 430 with osteosarcoma, and 469 with Ewing sarcomas. Overall median survival was histology-specific (osteosarcoma, 11 months; Ewing sarcoma, 26 months; chondrosarcoma, 37 months) and significantly worse in patients with distant metastasis at presentation for all tumor types. Schoenfeld et al. 29) performed a retrospective review of cases of osteosarcoma involving the spine treated. The median overall survival for all patients was 29.5 months. Local recurrence developed in 27%, and metastasis occurred in 62%. In our study, overall survival was 30 months in the osteosarcoma and MFH group and 72 months in the Ewing' sarcoma and chondrosarcoma group, which were quite different from those from Mukherjee et al.'s study. However, their study analyzed the data obtained from last 30 years, but our study analyzed the data from recent 10 years. Two-fold increase in survival is observed between previous 30 years and recent 10 years. The reasons for the increase in survival can be summarized as follows 6,11,13,19,27,33-35); 1) early detection, 2) close follow-up, and 3) development of advanced treatment modalities - en bloc resection technique, effective chemotherapeutic agents, and sophisticated radiation delivery technique. The development of advanced diagnostic techniques leads to early detection of the disease, which implies that most of patients are diagnosed without distant metastasis 11,13,34). This fact can be applied to recurrence detection. Close follow-up results in early detection of recurrence, leading to survival prolongation. Technical improvement in treatment modalities increased the survival. In surgical method, en-bloc spondylectomy enabled more extensive resection of the spinal lesions 27). Rao et al. 27) compared survival rates in en-bloc spondylectomy and intralesional resection for patients with spinal sarcoma (including metastatic sarcoma). Patients undergoing en-bloc resection had a median survival of 26.2 months, and those with intralesional resection had a median survival of 18.6 months. Teng et al. 35) conducted similar research targeting the patients with MFH of the spine. Compared to the 14 months median survival in debulking surgery group, that of the en-bloc resection group was 25 months. Both studies showed that en-bloc spondylectomy could improve tumor control and survival rate. In addition, the radiation therapy such as stereotactic radiosurgery and tomotherapy was developed and diversified, excellent local tumor control could be achieved without radiation injury to adjacent spinal cord 6,19,33). It would be the best to compare the survival period based on each histologic type. However, it was impossible to compare individual histology, because the number of patients in each group was low. Thus, we grouped tumors with similar clinical characteristics and compared them. Although MFH is different from osteosarcoma in pathological finding (no tumor bone production), it is considered to be similar in clinical course and response to chemotherapy 26). Therefore, These two tumors were included in the same group. Even if no significant difference was found in three groups, we assume that if more cases could be collected enough to compare individual histologic type, meaningful difference might be produced.
CONCLUSION
Primary spinal sarcomas are a mixed disease entity composed of several different histologic types. Treatment for them is challenging and not fully established. Present analysis showed that overall survival was 60 months, which is varying depending on histology and recurrence rate is so high. Close follow-up is required because recurrence could be within two or three years from initial diagnosis. The advancement in diagnostic and therapeutic techniques is gradually improving survival.
References
1. Allison DC, Carney SC, Ahlmann ER, Hendifar A, Chawla S, Fedenko A, et al : A meta-analysis of osteosarcoma outcomes in the modern medical era. Sarcoma 2012, 2012 : 704872,     2. Arndt CA, Rose PS, Folpe AL, Laack NN : Common musculoskeletal tumors of childhood and adolescence. Mayo Clin Proc 2012, 87 : 475-487,    3. Ballo MT, Zagars GK, Cormier JN, Hunt KK, Feig BW, Patel SR, et al : Interval between surgery and radiotherapy : effect on local control of soft tissue sarcoma. Int J Radiat Oncol Biol Phys 2004, 58 : 1461-1467,   4. Bernthal NM, Federman N, Eilber FR, Nelson SD, Eckardt JJ, Eilber FC, et al : Long-term results (>25 years) of a randomized, prospective clinical trial evaluating chemotherapy in patients with high-grade, operable osteosarcoma. Cancer 2012, 118 : 5888-5893,   5. Bölling T, Hardes J, Dirksen U : Management of bone tumours in paediatric oncology. Clin Oncol (R Coll Radiol) 2013, 25 : 19-26,   6. Castelli J, Thariat J, Benezery K, Courdi A, Chanalet S, Paquis P, et al : [Spinals and paraspinals tumors treated by CyberKnife : feasibility and efficacy]. Cancer Radiother 2010, 14 : 5-10,   7. Chaichana KL, Parker SL, Mukherjee D, Cheng JS, Gokaslan ZL, McGirt MJ : Assessment of the extent of surgical resection as a predictor of survival in patients with primary osseous spinal neoplasms. Clin Neurosurg 2011, 58 : 117-121,   8. Damron TA, Ward WG, Stewart A : Osteosarcoma, chondrosarcoma, and Ewing's sarcoma : National Cancer Data Base Report. Clin Orthop Relat Res 2007, 459 : 40-47,   9. Dorfman HD, Czerniak B : Bone cancers. Cancer 1995, 75( 1 Suppl):203-210,   10. Enneking WF, Spanier SS, Goodman MA : A system for the surgical staging of musculoskeletal sarcoma. 1980. Clin Orthop Relat Res 2003, 4-18,  11. Hillner BE, Siegel BA, Liu D, Shields AF, Gareen IF, Hanna L, et al : Impact of positron emission tomography/computed tomography and positron emission tomography (PET) alone on expected management of patients with cancer : initial results from the National Oncologic PET Registry. J Clin Oncol 2008, 26 : 2155-2161,   12. Hsu W, Kosztowski TA, Zaidi HA, Dorsi M, Gokaslan ZL, Wolinsky JP : Multidisciplinary management of primary tumors of the vertebral column. Curr Treat Options Oncol 2009, 10 : 107-125,   13. Ilaslan H, Sundaram M, Unni KK, Shives TC : Primary vertebral osteosarcoma : imaging findings. Radiology 2004, 230 : 697-702,   14. Katonis P, Alpantaki K, Michail K, Lianoudakis S, Christoforakis Z, Tzanakakis G, et al : Spinal chondrosarcoma : a review. Sarcoma 2011, 2011 : 378957,     15. Kawahara N, Tomita K, Murakami H, Demura S, Yoshioka K, Miyazaki T : Total excision of a recurrent chondrosarcoma of the thoracic spine : a case report of a seven-year-old boy with fifteen years follow-up. Spine (Phila Pa 1976) 2010, 35 : E481-E487,   16. Kelley SP, Ashford RU, Rao AS, Dickson RA : Primary bone tumours of the spine : a 42-year survey from the Leeds Regional Bone Tumour Registry. Eur Spine J 2007, 16 : 405-409,   17. Kim SH, Bak KH, Kim DW, Kang TH : Primary intramedullary spinal sarcoma : a case report and review of the current literatures. J Korean Neurosurg Soc 2010, 48 : 448-451,    18. Klimo P Jr, Codd PJ, Grier H, Goumnerova LC : Primary pediatric intraspinal sarcomas. Report of 3 cases. J Neurosurg Pediatr 2009, 4 : 222-229,   19. Levine AM, Coleman C, Horasek S : Stereotactic radiosurgery for the treatment of primary sarcomas and sarcoma metastases of the spine. Neurosurgery 2009, 64( 2 Suppl):A54-A59,   20. Lewis VO : What's new in musculoskeletal oncology. J Bone Joint Surg Am 2009, 91 : 1546-1556,   21. Lloret I, Server A, Bjerkehagen B : Primary spinal chondrosarcoma : radiologic findings with pathologic correlation. Acta Radiol 2006, 47 : 77-84,   22. McGirt MJ, Gokaslan ZL, Chaichana KL : Preoperative grading scale to predict survival in patients undergoing resection of malignant primary osseous spinal neoplasms. Spine J 2011, 11 : 190-196,   23. Mukherjee D, Chaichana KL, Adogwa O, Gokaslan Z, Aaronson O, Cheng JS, et al : Association of extent of local tumor invasion and survival in patients with malignant primary osseous spinal neoplasms from the surveillance, epidemiology, and end results (SEER) database. World Neurosurg 2011, 76 : 580-585,   24. Mukherjee D, Chaichana KL, Gokaslan ZL, Aaronson O, Cheng JS, McGirt MJ : Survival of patients with malignant primary osseous spinal neoplasms : results from the Surveillance, Epidemiology, and End Results (SEER) database from 1973 to 2003. J Neurosurg Spine 2011, 14 : 143-150,   25. Pickle LW, Hao Y, Jemal A, Zou Z, Tiwari RC, Ward E, et al : A new method of estimating United States and state-level cancer incidence counts for the current calendar year. CA Cancer J Clin 2007, 57 : 30-42,   26. Pobirci DD, Bogdan F, Pobirci O, Petcu CA, Roşca E : Study of malignant fibrous histiocytoma : clinical, statistic and histopatological interrelation. Rom J Morphol Embryol 2011, 52( 1 Suppl):385-388,  27. Rao G, Suki D, Chakrabarti I, Feiz-Erfan I, Mody MG, McCutcheon IE, et al : Surgical management of primary and metastatic sarcoma of the mobile spine. J Neurosurg Spine 2008, 9 : 120-128,   28. Schaser KD, Melcher I, Luzzati A, Disch AC : Bone sarcoma of the spine. Recent Results Cancer Res 2009, 179 : 141-167,   29. Schoenfeld AJ, Hornicek FJ, Pedlow FX, Kobayashi W, Garcia RT, DeLaney TF, et al : Osteosarcoma of the spine : experience in 26 patients treated at the Massachusetts General Hospital. Spine J 2010, 10 : 708-714,   30. Sciubba DM, Okuno SH, Dekutoski MB, Gokaslan ZL : Ewing and osteogenic sarcoma : evidence for multidisciplinary management. Spine (Phila Pa 1976) 2009, 34( 22 Suppl):S58-S68,   31. Stanelle EJ, Christison-Lagay ER, Healey JH, Singer S, Meyers PA, La Quaglia MP : Pediatric and adolescent synovial sarcoma : multivariate analysis of prognostic factors and survival outcomes. Ann Surg Oncol 2013, 20 : 73-79,   32. Stuckey RM, Marco RA : Chondrosarcoma of the mobile spine and sacrum. Sarcoma 2011, 2011 : 274281,     33. Sundaresan N, Boriani S, Rothman A, Holtzman R : Tumors of the osseous spine. J Neurooncol 2004, 69 : 273-290,   34. Sundaresan N, Rosen G, Boriani S : Primary malignant tumors of the spine. Orthop Clin North Am 2009, 40 : 21-36,   35. Teng H, Xinghai Y, Wei H, Huang Q, Xiao J, Zhang C : Malignant fibrous histiocytoma of the spine : a series of 13 clinical case reports and review of 17 published cases. Spine (Phila Pa 1976) 2011, 36 : E1453-E1462,   36. Tural D, Molinas Mandel N, Dervisoglu S, Oner Dincbas F, Koca S, Colpan Oksuz D, et al : Extraskeletal Ewing's sarcoma family of tumors in adults : prognostic factors and clinical outcome. Jpn J Clin Oncol 2012, 42 : 420-426,   37. Vasileios KA, Eward WC, Brigman BE : Surgical treatment and prognosis in patients with high-grade soft tissue malignant fibrous histiocytoma of the extremities. Arch Orthop Trauma Surg 2012, 132 : 955-961,   38. von Eisenhart-Rothe R, Toepfer A, Salzmann M, Schauwecker J, Gollwitzer H, Rechl H : [Primary malignant bone tumors]. Orthopade 2011, 40 : 1121-1142,   39. Wang VY, Potts M, Chou D : Sarcoma and the spinal column. Neurosurg Clin N Am 2008, 19 : 71-80,   40. Weber KL : What's new in musculoskeletal oncology. J Bone Joint Surg Am 2005, 87 : 1400-1410,   41. Wisanuyotin T, Radapat K, Sirichativapee W, Paholpak P, Kosuwon W, Sumnanoont C, et al : Prognostic factors and clinical outcomes in synovial sarcoma of the extremities. Asia Pac J Clin Oncol 2013, 9 : 80-85,  
Fig. 1
Kaplan-Meier estimated survival in patients with primary sarcoma of the spine according to histologic type. Median values of survival were 30 months (group I), 60 months (group II), and 74 months (group III). There was no statistical significance among three groups (p=0.427). 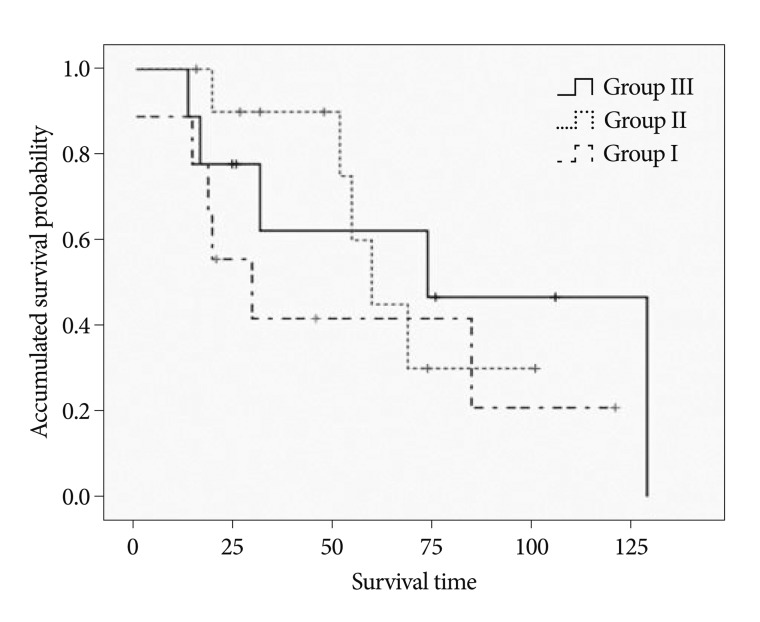
Fig. 2
The survival difference between group with distant metastasis and group without metastasis. Median values were 30 months (metastasis) and 85 months (no metastasis) (p=0.002). 
Fig. 3
The rate of patients who maintain ambulatory function at the last follow-up. In patients who did not have weakness at initial diagnosis, 86.7% of patients could walk at the last follow-up. However, in patients who had weakness at initial diagnosis, 42.9% could maintain ambulatory function at the last follow-up (p=0.013). 
Table 1
Demographic data in 29 patients of primary spinal sarcomas 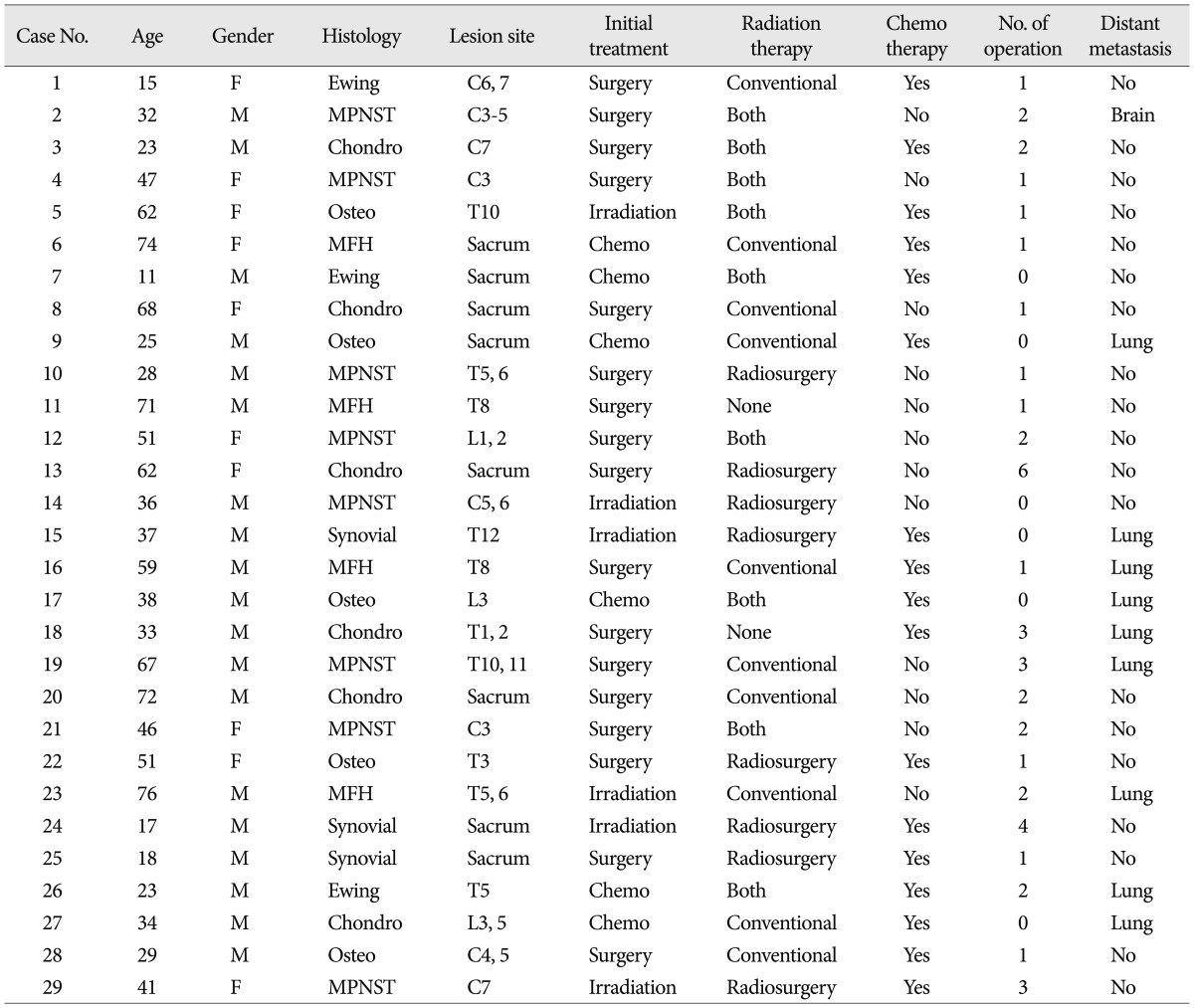
Table 2
Histologic types of primary spinal sarcomas 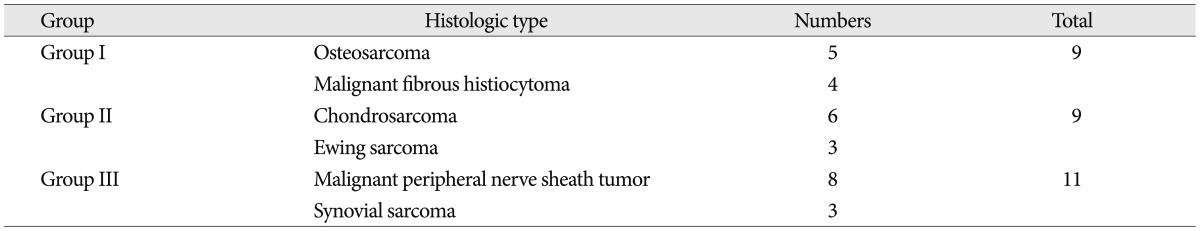
Table 3
Prognostic factors relating to survival 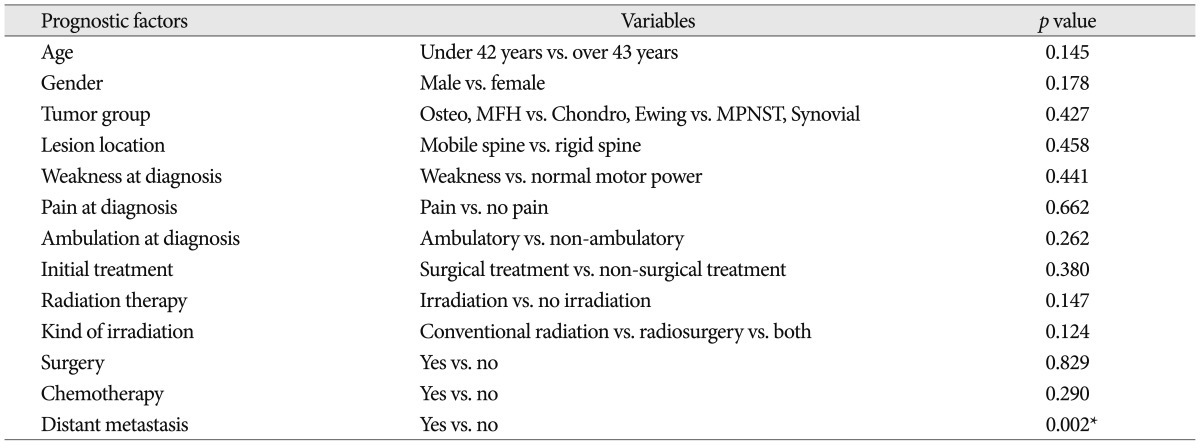
Table 4
Prognostic factors relating to recurrence 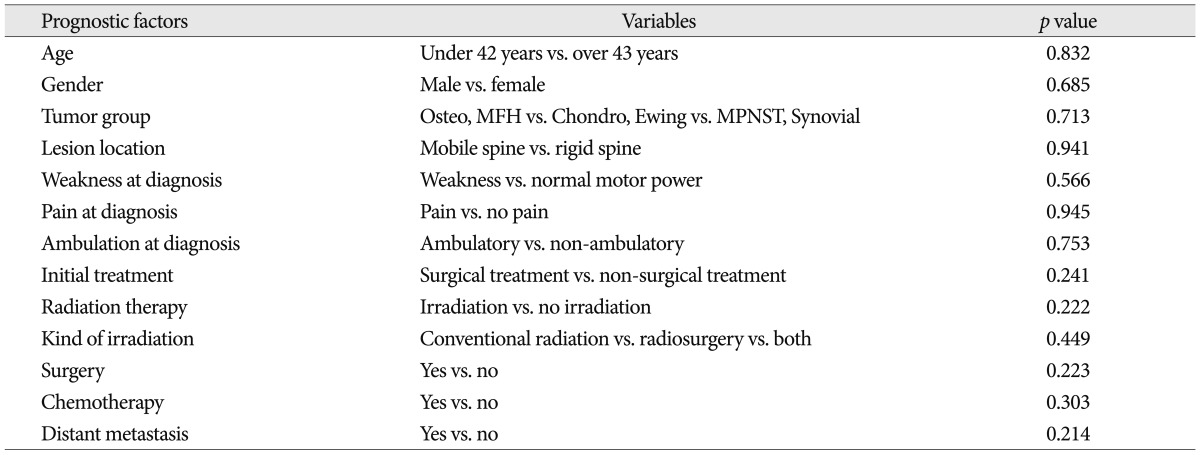
Table 5
Prognostic factors relating to ambulatory function 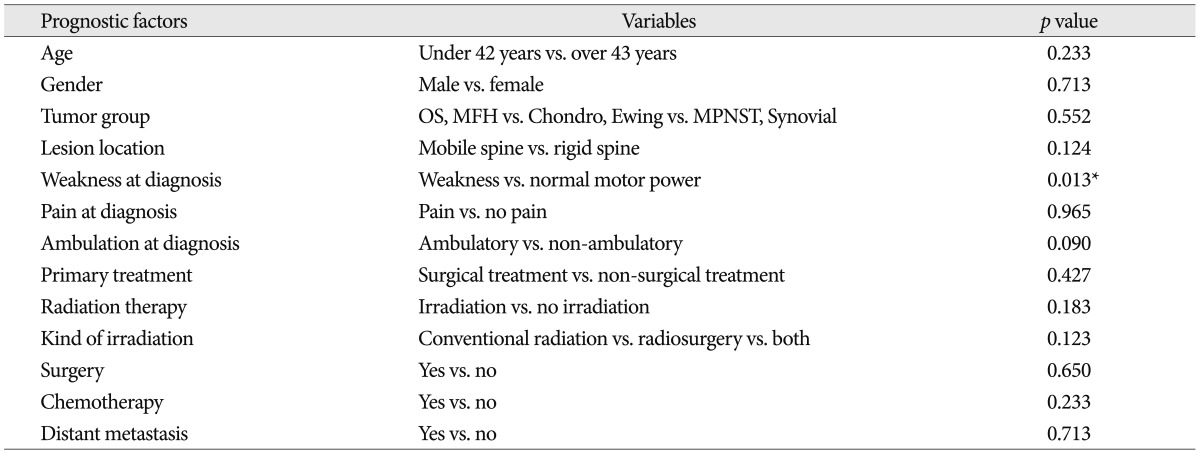
|
|