INTRODUCTION
Ganglion cyst usually originates from vertebral facet joints like synovial cyst8). The terms "ganglion cyst" and "synovial cyst" have similar clinical and radiographic features and are considered an extrusion of the synovium through a capsular defect from a degenerative or unstable facet joint. Usually, they are asymptomatic but it may cause symptoms if it compromise the surrounding thecal sac or nerve roots13,18).
CASE REPORT
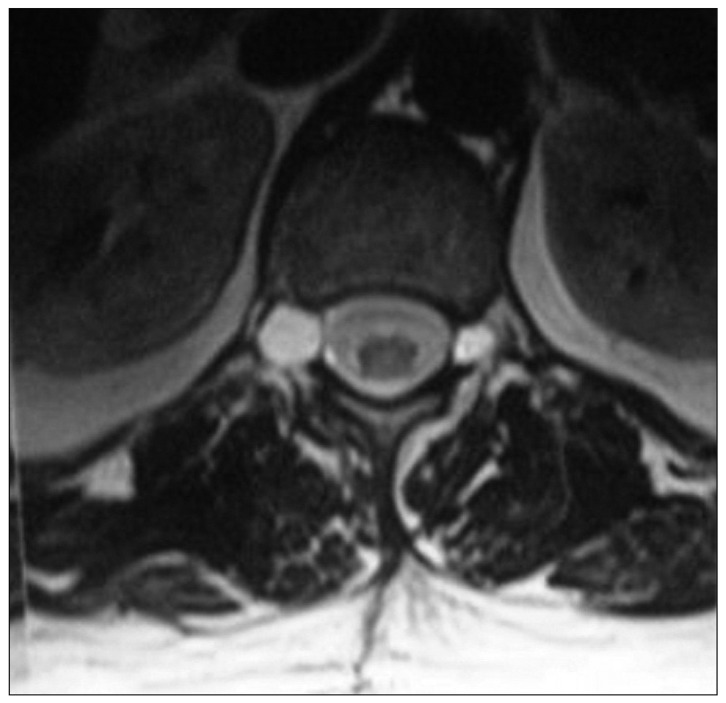
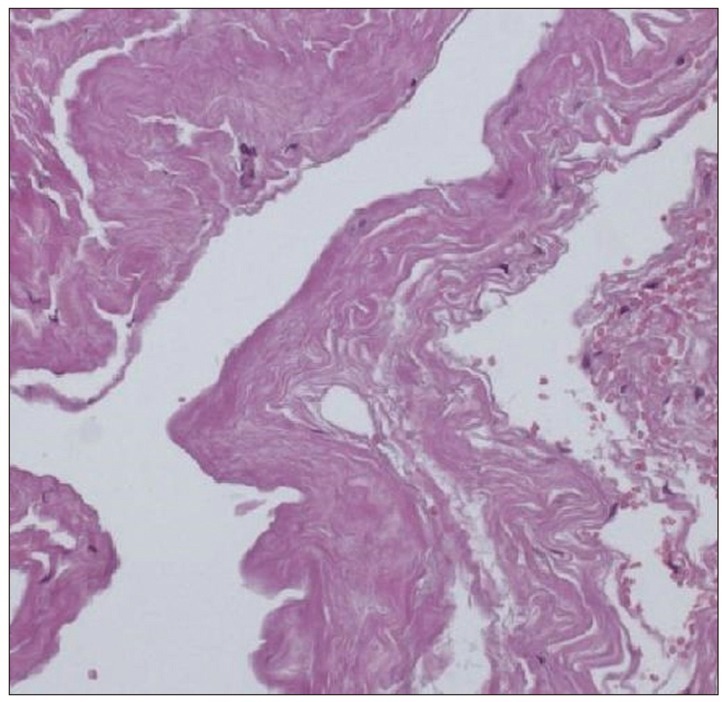
A 53-year-old female suffered from severe bilateral groin pain and dysesthesia for three months. She had this intermittent pain for 12 years, but the symptoms became worsening in the last three months. The visual analog scale score for pain was 8 out of 10. The pain was not relieved by conservative treatment. Her medical history was unremarkable. Her neurological examination was normal but she was suffering so much groin pain while walking. Thoracic magnetic resonance imaging (MRI) revealed bilateral, well circumscribed extradural, intraforaminal masses in continuity with the right and left apophyseal joints at Th12-L1 level (Fig. 1). Sagittal T2-weighted thoracolomber MRI revealed the bilateral roots compression caused by this cystic lesion cystic lesions at Th12-L1 level (Fig. 2). The patient underwent bilateral hemi-laminectomy and flavectomy at the Th12 level. Using the operative microscope, following exposure the foramens, bilateral cystic masses, emerging from the facet joints and compressing the dural sac and nerve roots were removed. The cysts were adhered tightly to the first lumbar dorsal root ganglion. The histopathological findings were consistent with ganglion cyst (Fig. 3). The patient made an excellent post-operative recovery with full resolution of preoperative symptoms.
DISCUSSION
The terms intraspinal ganglion and synovial cysts are used interchangeably, but the presence or absence of a synovial lining membrane is the distinguishing feature. These two entities are more likely different endpoints of the same etiopathologic process. They have similar clinical and radiographic features and are considered an extrusion of the synovium through a capsular defect from a degenerative or unstable facet joint. The ganglion/synovial cysts generally arise from facet joint but they may arise also from ligamentum flavum, posterior longitudinal ligament, annulus fibrosis and disc itself3,8,17). The majority of ganglion cysts in the lumbar spine occur at L4-L5 level and occasionally at L5-S1 and L3-L41,8,9,14). Intraforaminal cysts at Th12-L1 level and bilateral formation are very rare6). Cysts in the cervical spine and thoracic spine are also more rare2,4,10).
The pathogenesis of ganglion cysts is the subject of considerable controversy in the literature, but the most accepted etiology is the herniation of synovial tissue and its content from the articular cavity through a defect in the wall of the articular capsule3). The possible causative factors include repetitive trauma, spondylolysthesis, facet artrosis, myxoid degeneration, proliferation of mesenchymal cells, and increased hyaluronidase production. Increased stress placed on the mobile segment of the vertebrae may precipitate the development of the ganglion cyst15).
The clinical presentation of a ganglion cyst depends on its site, size and relationship with surrounding structures. Ganglion cysts usually are asymptomatic due to mostly located on the dorsal aspect of facet joints. According to its location, ganglion cyst may cause neurogenic claudication, cauda equine syndrome or radicular pain13). Acute radicular pain may be associated with intracystic haemorrhage and can result from acute cyst distention or compression of a nervous element8). Surgical treatment is recommended if it is causing intractable pain and/or neurological deficit12). The use of newer imaging modalities such as CT and MRI increased the frequency of preoperative diagnosis of this pathology that could once be identified during surgery1,5). MRI is the modality of choice for the diagnosis of ganglion cysts11,16). Ganglion cysts appear high signal intensity lesions with a fibrous capsule on T2 weighted image. In the differential diagnosis, extruded or sequestered disc fragment, cyst of the ligamentum flavum, perineural cyst, schwannoma, menengioma, metastasis, arachnoid cysts and rheumatoid pannus should be considered1,3,7).
CONCLUSION
The ganglion cyst occurs mostly in the dorsolateral trunk and arise with the greatest frequency in the lumbar spine and less frequently in the cervical and thoracic spine. They may cause symtoms if they located in the intervertebral foramens and compromise dorsal root ganglion. This is an uncommon case that ganglion cyst is located at Th12-L1 intervertebral foramens, bilaterally.