INTRODUCTION
Traumatic brain injury (TBI) is the most frequent reason for neurosurgical consultation in the emergency room. Minor or mild TBI is common in elderly patients, many of whom are treated on anticoagulant. The common practice is to discharge these patients if computed tomography (CT) of the brain is normal. However, a small subgroup of these patients may experience a delayed intracranial bleeding2,4).
Here, we describe a patient on anticoagulant therapy that developed an acute subdural haematoma (SDH) 48 hours after a mild head injury. We also briefly review the pertinent literature and discuss the pathogenesis of delayed onset. Furthermore, this case report wishes to raise the awareness among emergency department physicians and neurosurgeons that treat elderly anticoagulated patients, for a possible delayed onset of intracranial haematoma, even if the initial assessment is normal.
CASE REPORT
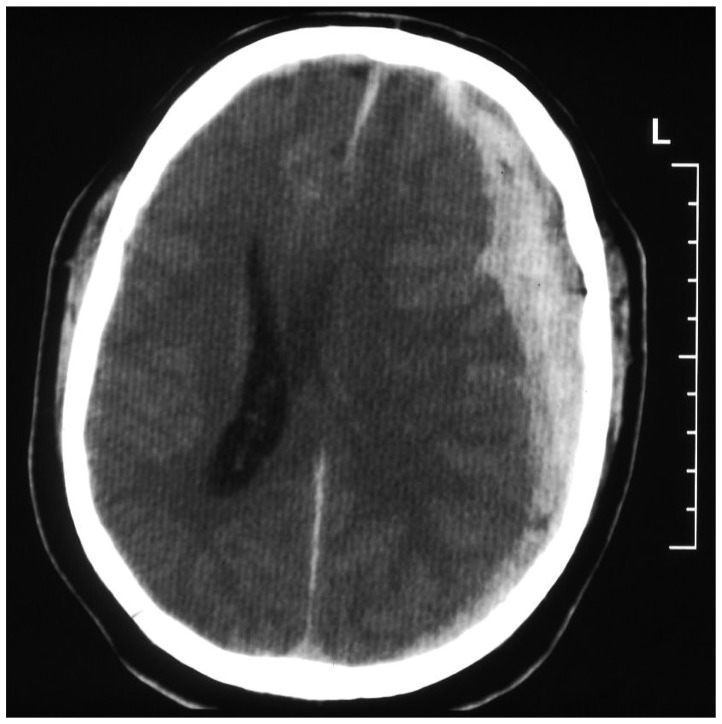
A 66-year-old male presented to the emergency department after a fall and a mild head trauma. He had no history of loss of consciousness or posttraumatic amnesia. The patient had a history of atrial fibrillation and was on acenocoumarol (Sintromآ®). His neurological examination was intact. Initial CT scan of the brain was without any sign of intracranial hemorrhage or cranial fracture (Fig. 1). The laboratory workup revealed an International Normalized Ratio (INR) of 2.5. After an 8-hour observation period, he was discharged home.
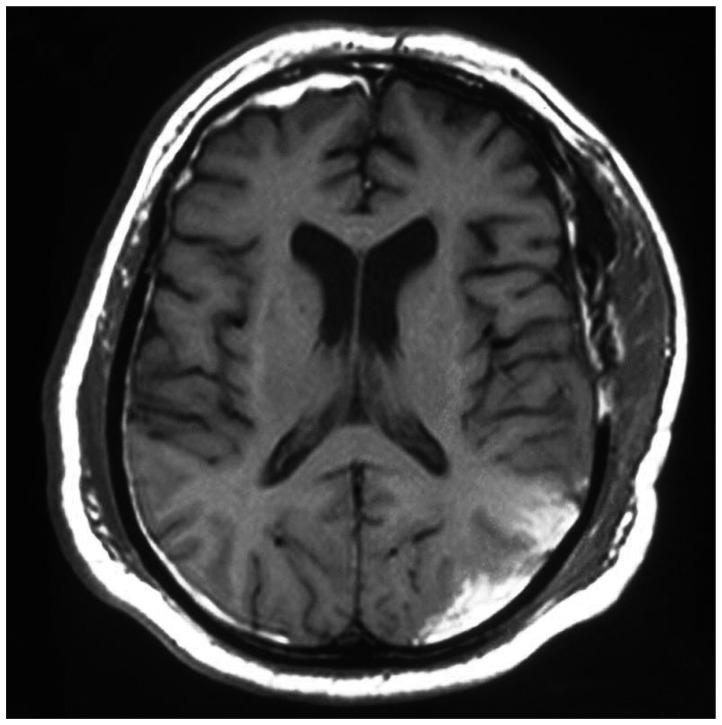
Forty-eight hours later the patient was transferred to the emergency room with a decreased level of consciousness and vomiting. On neurological examination he had a score of 9/15 on the Glasgow Coma Scale (E2V2M5) and a dilated left pupil unresponsive to light. A CT scan of the brain revealed a large left acute SDH with midline shift (Fig. 2). The patient underwent a craniotomy with evacuation of a large subdural clot. The point of the haemorrhage was some bridging veins to the transverse sinus, which were promptly coagulated. Postoperatively, the left pupil became small and reactive and a CT scan demonstrated complete removal of SDH. The patient progressively improved and one month after the operation he was discharged for further physiotherapy (Fig. 3). Six months later the patient has a Glasgow Outcome Score of 3.
DISCUSSION
This case is another example of the very low risk of delayed subdural haematoma after minor head injury in patients, who are treated with anticoagulants. Some reports of delayed haematomas after minor head injury in adults, with a negative initial CT scan, have already been described. However, the incidence has turned out to be extremely low (<0.02%). It is generally accepted that elderly TBI patients are at greater risk for clinically important brain injury. Furtherrmore, oral anticoagulation is associated with a significant risk of intracranial bleeding, even after a minor head trauma2,3).
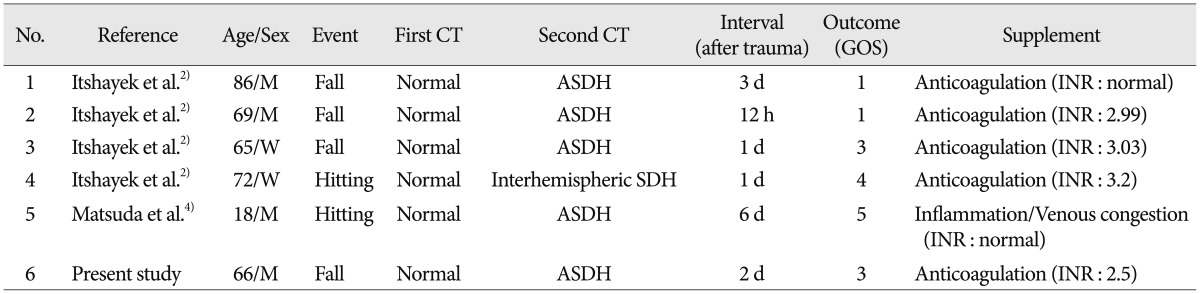
There have been previously five well-documented reports of delayed subdural haematoma after TBI2,5). The clinical and radiologic characteristics are summarized in Table 1.
As it is shown in the above table the outcome is mostly poor (5/6). More specifically, there were two deaths, two patients remained with severe and one with moderate disability, while one had a good recovery. The time interval to the subsequent scanning varied from 12 hours to 6 days.
There have been proposed several hypotheses regarding the pathogenesis of delayed intracranial haematomas. One commonly discussed mechanism for the development of acute SDH is the rupture of bridging veins, which empty into the dural sinuses. As the veins cross the subdural space, they have little supporting structure, and are therefore more vulnerable to injury at this point. In elderly patients with cerebral atrophy, bridging veins are stretched and transverse a greater distance in the subdural space. Doherty suggests that rupture of these veins is the mechanism for delayed SDH in patients with trauma-induced hypotension and cerebral edema. In addition, there is a delayed tamponade effect since the atrophied brain is shrunken away from the inner table of the skull. In these patients with hypotension, delayed bleeding may develop as blood pressure returns to normal after resuscitation1).
Matsuda et al.4) suggest, that inflammation or vasoparalysis resulting from local hypoxia after a head trauma may increase the permeability of the vessels and may form coalescent small perivascular haemorrhages. In this case, the patient had been straining to tighten a bolt of his football helmet when he suffered the acute subdural hemorrhage. This Valsalva maneuver might have caused increased intracranial pressure, hypercapnia, and subsequent venous congestion, resulting in subdural hemorrhage because of a rupture of coalescent vessels.
In our patient, it was found intraoperatively that the cause of the subdural hematoma was the tearing of some bridging veins to the transverse sinus. It is believed that these bridging veins were damaged by the primary injury and 48-hours later, a Valsalva maneuver and a temporary increase of the ICP could have caused the tearing of the bridging veins and the subsequent development of the haematoma.
Therefore, an overnight observation period and a negative first CT scan do not entirely eliminate the possibility that the patient will later develop an intracranial haematoma. This possibility, according to the persisting literature, seems to be greater for the patients over the age of 65, who are under anticoagulant therapy. The NICE guidelines6) state that it is safe to discharge the abovementioned patients if imaging is normal. However, as it was explained above, these patients may be then exposed to comparatively high risks of delayed deterioration.
Currently, there are no specific guidelines regarding the anticoagulated patients with a negative initial CT scan4). One recent paper from Menditto et al.5) also underlines the need for reevaluation of the current guidelines after a head injury on patients receiving anticoagulant therapy. They suggest a 24-hour observation period for all the patients under anticoagulants followed by a second CT scan. This protocol will identify most occurrences of delayed intracranial bleeding. However, two patients developed a delayed intracranial haemmorhage after the 24-hour observation period. Both of them had an INR greater than 3.0 and age over 65 years old.
Based on the current literature and on our experience we propose a modification of this protocol. We suggest all the patients receiving anticoagulants to be hospitalized for 24 hours followed by a second CT scan. For the subgroup of patients over the age of 65 and with an INR greater than 2.5, we suggest to extend the observation period to 48 hours followed by a CT scan. As long as we cannot prevent primary injuries, we should not fail to prevent fatal deterioration if at all possible.
CONCLUSION
Our case report underlines the need, that physicians and neurosurgeons should maintain a high level of vigilance in anticoagulated patients, after a mild TBI, due to a possible delayed onset of intracranial haematoma, even if the initial assessment is normal. We recommend that all anticoagulated patients, who experience a head injury, should be hospitalized for a 24-hour neurological observation followed by a second CT scan. For the subgroup of patients over the age of 65 and with an INR greater than 2.5, we suggest to extend the observation period to 48 hours followed by a CT scan.