Jeong, Lim, and Chae: Pediatric Stroke
Abstract
Pediatric stroke is relatively rare but may lead to significant morbidity and mortality. Along with the advance of brain imaging technology and clinical awareness, diagnosis of pediatric stroke is increasing wordwide. Pediatric stroke differs from adults in variable risk factor/etiologies, diverse and nonspecific clinical presentation depending on ages. This review will be discussed pediatric stroke focusing on their clinical presentations, diagnosis and etiologies/risk factors.
Key Words: Pediatric ┬Ę Stroke ┬Ę Clinical ┬Ę Risk factors ┬Ę Etiology ┬Ę Diagnosis.
INTRODUCTION
Stroke (focal cerebral injury with an underlying vascular basis) is typically classified into ischemic or hemorrhagic subtypes. Ischemic stroke (IS) is further subdivided into arterial ischemic stroke (AIS) and cerebral sinovenous thrombosis (CSVT). Stroke is increasingly recognized as a serious neurologic disorders of children and awareness about pediatric stoke is increasing. In western countries, the incidence of pediatric AIS is estimated at 2-3/100000 children/year during the first 5 years and 8-13/100000 from 5 to 14 years 8). Many cases occur during the perinatal or neonatal period, during which the incidence is approximately 1/4000 live birth 14). Stroke is also commonly encountered disease in the practice of pediatric neurology and among the top 10 causes of death in children, with highest rates in the 1st year of life in USA 2). Therefore, the timely appropriate diagnosis and detection of associated risk factors is very important to improve the management and modify the prognosis. However, even when stroke presents acutely, delays in diagnosis are common and appropriate treatments are difficult because pediatric stroke is relatively rare and the etiologies and associated risk factors are remarkably variable depending on ages and different from those of adults. The International Pediatric Stroke Study (IPSS) and other studies of childhood stroke reported various underlying systemic factors associated with pediatric stroke. In previous studies, preexisting risk factors have been reported in 77-79% of childhood stroke and varied depending on their ages and ethnics 11). The associated conditions are known to be congenital heart disease, vasculopathies, infection, metabolic disease, prothrombotic disorders and trauma. However, most of the previous studies have been established in European and western and few reported in Asian countries. Here, etiology and risk factors including our center experience, diagnosis of pediatric stroke particularly in arterial ischemic stroke will be focused in this review.
CLINICAL FEATURES AND DIAGNOSIS
Diagnosis of stroke in children is frequently delayed or missed, which reflect a combination of rareness, lack of awareness and complex differential diagnosis. Many studies have been reported the diagnostic delay beyond 24 hours from symptom onset 16). A high clinical suspicion, conjunction with a systematic diagnostic approach is required for timely diagnosis. The acute onset of focal neurologic deficit in children is considered to be stroke until otherwise proven. A couple of studies have reported how strokes present in children ( Table 1). AIS usually presents as a focal neurologic deficit. Hemiparesis is most common focal neurologic deficit but may be misdiagnosed as seizures or Todd's paralysis, meningitis/encephalitis, migraine, or demyelination, which are mimic strokes. Additional common focal neurologic deficits are diplopia, dysarthria, vertigo and ataxia. Seizures at the onset of stroke are common both in ischemic and hemorrhagic stroke, compared to adult. They occur in up to 50% of children, which are not restricted to any age group 24). In addition to focal neurologic deficits, non-focal and diffuse neurologic symptoms such as headache, confusion, irritability and behavioral changes are frequent especially in younger children 5,1323). Clinical presentation can be significantly different based on the child's age. The younger the child, more non-specific for their symptoms. Neonates usually present with seizures and symptoms of encephalopathy (irritability, lethargy, excessive sleeps, or poor feeding) or apnea. Focal neurologic deficits occur in less than 25% of all newborns. Toddlers can also present with nonspecific symptoms such as increased crying, drowsiness, irritability, poor feeding, vomiting and sepsis-like features. With increasing ages, stroke manifests with a clinical presentation similar to that in adults. The other typical presentation in children is fluctuation course of neurologic deficits, which are frequently brief/recurrent and may resolve as quickly as within a few hours. This should alert the clinician to the possibility of an underlying vasculopathy or thromboembolic causes.
There are many other diseases, which may mimic a stroke. Complicated migraine can cause focal neurologic deficits which typically resolve within 24 hours and usually having family history of hemiplegic migraine 23). Partial seizures can result in transient postictal paresis (Todd's palsy). Brain tumor as well as intracranial infection such as meningitis, encephalitis, and brain abscess are also considered as a differential diagnosis. Rarely alternating hemiplegia, metabolic disorders like Mitochondrial Encephalopathy, Lactic Acidosis and Stroke like episodes (MELAS) can also cause stroke like symptoms.
ETIOLOGIES/RISK FACTORS
Etiologies/risk factors in childhood stroke differ from those in adult stroke 11). The etiologies/risk factors identified in adult cases are primarily related to arrhythmias and obstructive atherosclerotic arteriopathies; in contrast, these are rarely thought to be related to childhood stroke. The International Pediatric Stroke Study (IPSS) and other studies of childhood stroke reported various underlying systemic factors. Approximately 50-80% children with AIS have at least one identifiable risk factor for stroke and multiple risk factors often present in as many a 25% of children with stroke 3,711). According to the largest study by the IPSS of 493 children with stroke in 10 countries, risk factor variability can be influenced by geography, ethnicity, age at presentation and the availability of medical resources 11). In neonatal stroke, dehydration, infection and congenital heart disease are more commonly associated compared to older children 13). Arteriopathies and congenital heart disease (CHD) are commonly associated from 20-50% of AIS in children in developed countries 1,10). Studies in Saudi Arabia and Northern India reported infectious etiologies to be the most common risk factor for stroke in tertiary centers, with similar findings in Beijing, China, and Turkey. In referral centers located in areas with a large African or Mediterranean population, hemoglobinopathies including sickle cell disease (SCD) may be the most common cause 15,1718,1920). In East Asian countries, MMD is the most common etiologies in pediatric stroke 9). Inherited metabolic diseases such as mitochondrial encephalopathies, Fabrys disease, Menke's disease, organic academia, urea cycle defects and homocystinuia can result in acute focal neurological deficits and stroke-like episodes. In cases of radiological evidence of infarction that is not confined to a known vascular territory, metabolic causes may be a consideration 6,2122). For assessment of etiologies and risk factors, there are no clearly established guidelines in pediatric stroke. Laboratory assessment including a variety of nonspecific blood tests and more specific tests searching for specific causes of stroke, such as coagulopathies, hematologic disorders or vasculitides are suggested ( Table 2).
DATA FROM TERTIARY CENTERS IN KOREA
We reviewed our cohort of 185 patients with pediatric stroke, who was confirmed as stroke by magnetic resonance imaging at our center, between January 2002 and June 2013, to analyze the risk factors/etiologies and their clinical outcomes based on stroke type and ages. Cases of neonatal and perinatal stroke were excluded. Other childhood cerebrovascular disorders that were excluded included transient ischemic attack without infarction, hypotensive watershed injury, reversible hypertensive leukoen-cephalopathy, diffuse hypoxic encephalopathies, and asymptomatic infarction.
Stroke was classified into AIS, CSVT, metabolic stroke (MS), and hemorrhagic stroke. MS results from energy failure caused by metabolic conditions such as mitochondrial disease, organic acidemias, and single-gene diseases. Risk factors for AIS were subdivided into four groups : arteriopathy, cardiac disease, prothrombotic condition, and hematologic disease.
Among 185 patients, male dominance was more prominent in adolescence (sex ratio, 3.5 : 1) than it was in preadolescence. The mean age at diagnosis was 6.5 years.
Most patients (n=149, 81%) had two of more symptoms at onset. One hundred seventy-four patients (94%) presented with focal neurological signs : paresis (n=132, 71%), seizure (n=71, 38%), speech impairment, paresthesia, and other focal neurological deficits. Diffuse signs were documented in 102 patients (55%) : headache (n=50, 27%), altered mentality (n=34, 18%), lethargy, nausea/vomiting, dizziness, and other diffuse signs. Ninety-one patients (49%) had both focal and diffuse signs (mixed signs).
There were 156 (156/185, 84.3%) patients with AIS, nine patients with CSVT, nine patients with MS, and 11 patients with HS. Presumptive risk factors were identified in 154 patients (83%).
In AIS, most common risk factors were arteriopathy, followed by cardiac disease, prothrombotic condition, and hematologic disease. Arteriopathy (n=83) includes MMD; CNS infection; inflammatory vasculopathy; systemic vasculitis; arterial dissection; other noninflammatory vasculopathies. Twenty-three patients had underlying cardiac diseases; congenital heart disease, infective endocarditis, arrhythmia, myocarditis, cardiomyopathy, and left atrial myxoma. Prothrombotic condition (n=14) includes methylenetetrahydrofolate reductase (MTHFR) gene mutation, antiphospholipid syndrome (APS) and chemotherapy. Hematologic disorders were detected on a single case basis in six patients; leukemia, iron-deficiency anemia, hemophagocytic lymphohistiocytosis, hemolytic uremic syndrome, thrombotic thrombocytopenic purpura, and suprasellar craniopharyngioma. CSVT was identified in nine patients : severe dehydration (n=3); infection (n=3); prothrombotic condition (n=3) such as APS, MTHFR gene mutation, and L-asparaginase. Nine patients were newly diagnosed as having mitochondrial disease : eight patients had mitochondrial encephalopathy with lactic acidosis and stroke-like episodes (MELAS), and were confirmed to have the mitochondrial DNA 3243 point mutation. Hemorrhagic stroke affected 11 patients. There were arteriovenous malformation, MMD, arterial aneurysm, arterial dissection, mycotic embolism, MTHFR gene mutation, and Evans syndrome.
Table 3 summarizes the risk factor by stroke types, including previous publication by Lee et al. 9). The most common single etiology was MMD in both centers.
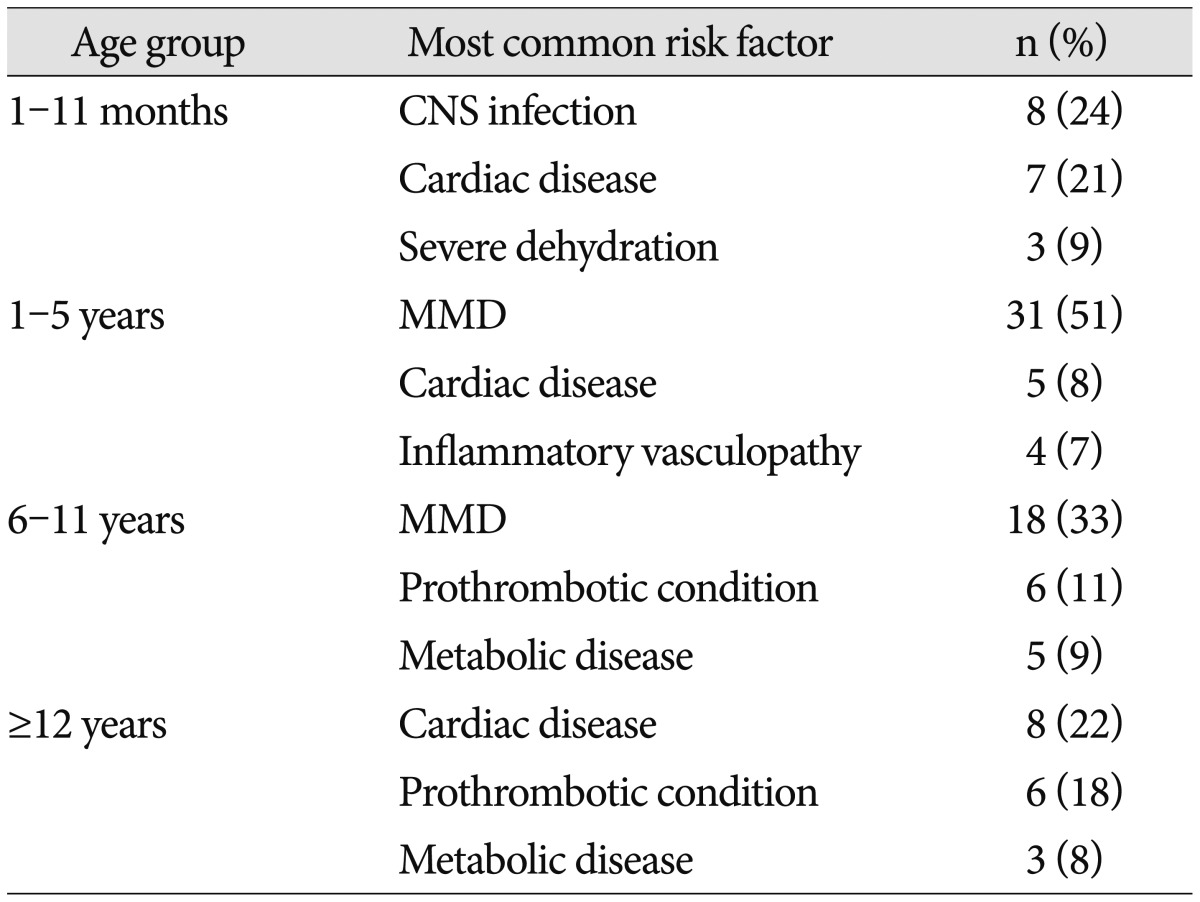
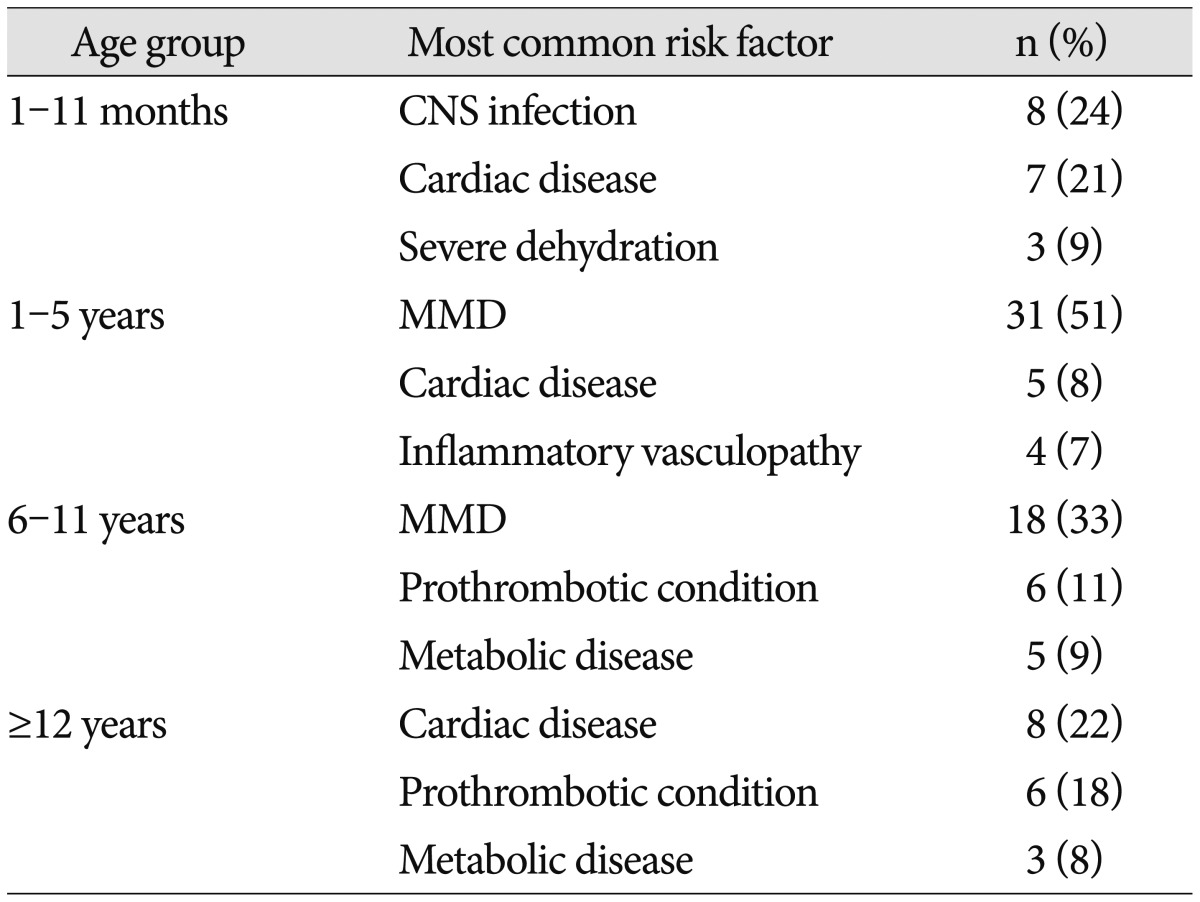
The most common etiology/risk factors are different according to ages in pediatric stroke. Stroke in children under 1 year of age is more likely to be associated with CNS infection, whereas older children were more likely to have vascular diseases including MMD. Cardiac diseases are relatively associated with all age groups ( Table 4).
CONCLUSION
Pediatric stroke is an importance cause of disability and mortality. However, since the incidence is still low, risk factors are variable according to ethnic groups and ages and etiologies are different, the symptoms are more non-specific compare to adults, it remains a challenge to early diagnosis and appropriate management.
Therefore, high suspicion is important for pediatric neurologists and early recognition, diagnosis, and appropriate treatment based on etiologies/risk factor can significantly improve the clinical outcome and quality of life.
References
1. Bowers KJ, Deveber GA, Ferriero DM, Roach ES, Vexler ZS, Maria BL : Cerebrovascular disease in children : recent advances in diagnosis and management. J Child Neurol 2011, 26 : 1074-1100,    2. C├Īrdenas JF, Rho JM, Kirton A : Pediatric stroke. Childs Nerv Syst 2011, 27 : 1375-1390,   3. deVeber G, Roach ES, Riela AR, Wiznitzer M : Stroke in children : recognition, treatment, and future directions. Semin Pediatr Neurol 2000, 7 : 309-317,   4. Earley CJ, Kittner SJ, Feeser BR, Gardner J, Epstein A, Wozniak MA, et al : Stroke in children and sickle-cell disease : Baltimore-Washington Cooperative Young Stroke Study. Neurology 1998, 51 : 169-176,   5. Freundlich CL, Cervantes-Arslanian AM, Dorfman DH : Pediatric stroke. Emerg Med Clin North Am 2012, 30 : 805-828,   6. Fullerton HJ, Wu YW, Sidney S, Johnston SC : Risk of recurrent childhood arterial ischemic stroke in a population-based cohort : the importance of cerebrovascular imaging. Pediatrics 2007, 119 : 495-501,   7. Ganesan V, Prengler M, McShane MA, Wade AM, Kirkham FJ : Investigation of risk factors in children with arterial ischemic stroke. Ann Neurol 2003, 53 : 167-173,   8. Kissela BM, Khoury JC, Alwell K, Moomaw CJ, Woo D, Adeoye O, et al : Age at stroke : temporal trends in stroke incidence in a large, biracial population. Neurology 2012, 79 : 1781-1787,    9. Lee EH, Yum MS, Ko TS : Risk factors and clinical outcomes of childhood ischemic stroke in a single Korean tertiary care center. J Child Neurol 2012, 27 : 485-491,   10. Lynch JK, Hirtz DG, DeVeber G, Nelson KB : Report of the National Institute of Neurological Disorders and Stroke workshop on perinatal and childhood stroke. Pediatrics 2002, 109 : 116-123,   11. Mackay MT, Wiznitzer M, Benedict SL, Lee KJ, Deveber GA, Ganesan V : International Pediatric Stroke Study GroupArterial ischemic stroke risk factors : the International Pediatric Stroke Study. Ann Neurol 2011, 69 : 130-140,   12. Meyer-Heim AD, Boltshauser E : Spontaneous intracranial haemorrhage in children : aetiology, presentation and outcome. Brain Dev 2003, 25 : 416-421,   13. Moharir M, Deveber G : Pediatric arterial ischemic stroke. Continuum (Minneap Minn) 2014, 20( 2 Cerebrovascular Disease):370-386,    14. Nelson KB, Lynch JK : Stroke in newborn infants. Lancet Neurol 2004, 3 : 150-158,   15. Per H, Unal E, Poyrazoglu HG, Ozdemir MA, Donmez H, Gumus H, et al : Childhood stroke : results of 130 children from a reference center in Central Anatolia, Turkey. Pediatr Neurol 2014, 50 : 595-600,   16. Rafay MF, Pontigon AM, Chiang J, Adams M, Jarvis DA, Silver F, et al : Delay to diagnosis in acute pediatric arterial ischemic stroke. Stroke 2009, 40 : 58-64,   17. Salih MA, Abdel-Gader AG, Al-Jarallah AA, Kentab AY, Gadelrab MO, Alorainy IA, et al : Infectious and inflammatory disorders of the circulatory system as risk factors for stroke in Saudi children. Saudi Med J 2006, 27 Suppl 1 : S41-S52,  18. Salih MA, Al-Jarallah AS, Abdel-Gader AG, Al-Jarallah AA, Al-Saadi MM, Kentab AY, et al : Cardiac diseases as a risk factor for stroke in Saudi children. Saudi Med J 2006, 27 Suppl 1 : S61-S68,  19. Salih MA, Murshid WR, Zahraa JN, Abdel-Gader AG, Al-Jarallah AA, Kentab AY, et al : Congenital and genetic cerebrovascular anomalies as risk factors for stroke in Saudi children. Saudi Med J 2006, 27 Suppl : S53-S60,
20. Shi KL, Wang JJ, Li JW, Jiang LQ, Mix E, Fang F, et al : Arterial ischemic stroke : experience in Chinese children. Pediatr Neurol 2008, 38 : 186-190,   21. Testai FD, Gorelick PB : Inherited metabolic disorders and stroke part 1 : Fabry disease and mitochondrial myopathy, encephalopathy, lactic acidosis, and strokelike episodes. Arch Neurol 2010, 67 : 19-24,   22. Testai FD, Gorelick PB : Inherited metabolic disorders and stroke part 2 : homocystinuria, organic acidurias, and urea cycle disorders. Arch Neurol 2010, 67 : 148-153,   23. Tsze DS, Valente JH : Pediatric stroke : a review. Emerg Med Int 2011, 2011 : 734506,     24. Younkin DP : Diagnosis and treatment of ischemic pediatric stroke. Curr Neurol Neurosci Rep 2002, 2 : 18-24,  
Table┬Ā1
Clinical presentation of pediatric stroke

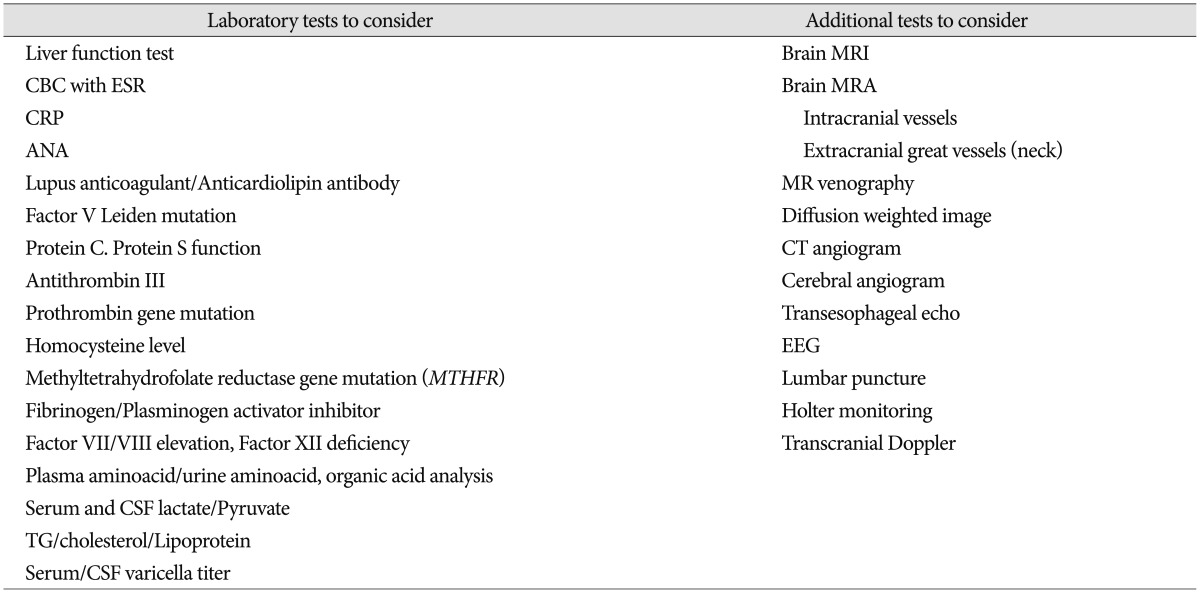
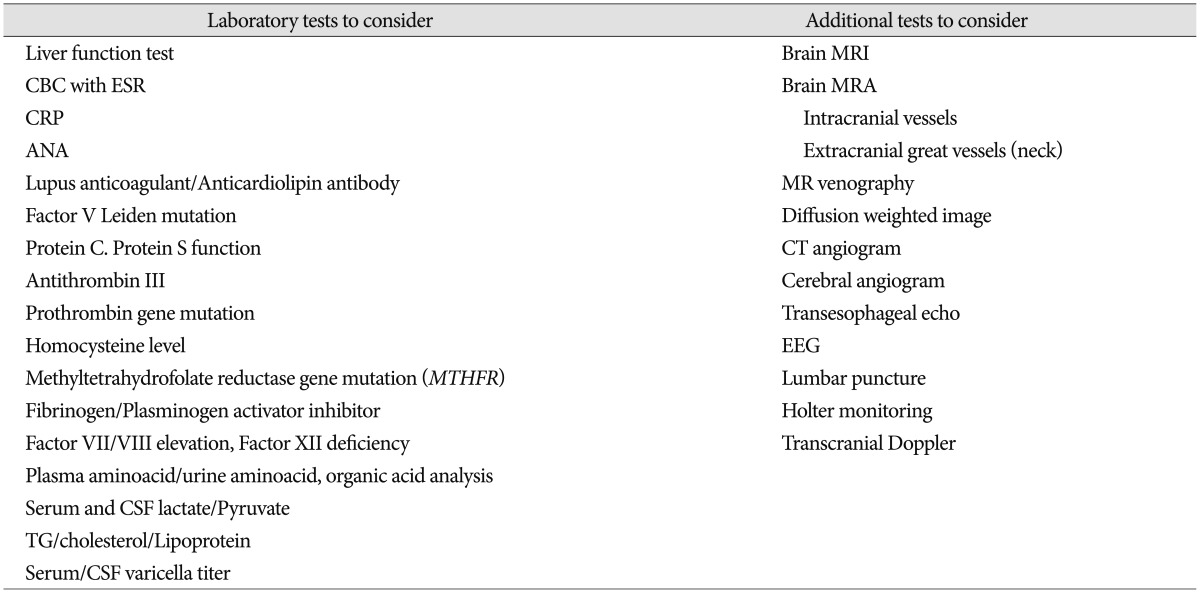
Table┬Ā2
Laboratory and diagnostic investigation for pediatric stroke
Table┬Ā3
Risk factors according to stroke type

Table┬Ā4
Most common risk factors according to age group*
|
|