Le, Nguyen, Do, Nguyen, and Vo: Guidance of Nerve Stimulator and Ultrasound for Transforaminal Epidural Steroid Injection in Lumbosacral Radicular Pain : A Single Institution Experience in Vietnam
Abstract
Objective
This study aimed to evaluate the clinical feasibility of the combination of ultrasound and nerve stimulator guidance in transforaminal epidural steroid injections (TESIs) to manage lumbosacral chronic radicular pain.
Methods
Using the combination of nerve stimulator and ultrasound guidance, TESIs were performed in 125 segments of 78 patients who presented with chronic lumbar radicular pain. Demographic characteristics and surgical outcomes were recorded on admission, pre-procedural and post-procedural for 1-week, 1-month, 3-month, and 6-month follow-ups. The result was measured using the Numeric rating scale (NRS) and Oswestry disability index (ODI).
Results
Patients who received TESIs showed significant improvements on two evaluation tools (NRS, ODI), compared to that before procedure (p<0.001). No significant complications were observed for 6 months’ follow-up.
Conclusion
The result suggests that a combination of ultrasound and nerve stimulator guidance in transforaminal epidural injections is safe, reliable and effective for short-term management of lumbar disc herniation. It is a promising technique and has shown good results in providing intermediate pain relief.
Key Words: Chronic pain · Injections · Ultrasound.
INTRODUCTION
Nowadays, the acknowledgment of chronic pain has gone further in etiology, predisposing factors, consequences and management. The argument about “Is Chronic Pain a Disease” is a debated topic that often divides opinion [ 1, 18]. The Global Burden of Disease 2019, has continuously dictated that chronic low back pain (CLBP) remained the leading cause of years lived with disability [ 6]. CLBP exerts an enormous personal and economic burden [ 3]. The patient suffering a CLBP is recommended to classify into one of four groups : 1) nonspecific low back pain; 2) back pain associated with a radiculopathy or spinal stenosis; 3) back pain referred from a non-spinal source; or 4) back pain associated with another specific spinal cause [ 13]. Management of lumbar disc herniation requires a multidisciplinary approach, including conservative management and surgery [ 12, 14]. The transforaminal epidural steroid injections (TESIs) for the treatment of lumbosacral radicular pain had been studied as target-specific, minimally invasive therapy and reported to be more effective than interlaminar and caudal routes [ 7, 8]. TESIs under the fluoroscopy (FL) guide have demonstrated their accuracy and effectiveness; but have significant disadvantages, such as the irradiation of the patients and the physicians, high cost and ambitious technique [ 14]. In recent years, ultrasound (US) has been proven successful in identifying the anatomical structure of the spine and in the methods of lumbar pararadicular infiltration. Injections performed under US guidance significantly reduced the procedure time and no radiation exposure [ 2, 21]. Nerve stimulator or electrical stimulation as a safeguard against neural injury has been studied extensively about peripheral nerve blocks, and to decrease the incidence of injury during peripheral nerve blocks. Before the use of nerve stimulator, it was assumed that eliciting paresthesia may predict proximity to a specific nerve. The interventionist initially attempts to seek the nerve by low-voltage stimulation at a frequency of 50 Hz, aiming for the most vital sensory stimulation at the lowest possible voltage. The cannula needs to be within 3 mm of the nerve to create an adequate lesion and a maximum stimulation level of around 0.6 V would indicate this. The interventionist always ensures that the cannula is not dangerously close to any motor nerve when trying to lesion a sensory nerve. The introduction of US allowed for objectively measuring needle proximity to a target nerve. This body of evidence indicates that a proportion of patients exhibit no motor response with both intraneural and epineural needle tip position when a magnitude of current that maintains specificity is applied to peripheral nerves [ 4, 15]. This helps interventionist determine the appropriate spinal segment of radial pain. We use a nerve stimulator guidance to improve the success of needle trajectory and to target correct position during US-guided TESI. Almost prior injection techniques under sonography required firm solutions by FL or computer tomography (CT) images. This study used both US and nerve stimulator guidance to perform TESIs. We proposed to evaluate the effectiveness of the double guide during TESIs to manage in lumbar disc herniation with chronic radicular pain.
MATERIALS AND METHODS
Ethics considerations
The study was approved by the Ethics Committee of The University Medical Center with decision number IRBVN01003/IRB00010293/FWA00023448 No.115/GCN-HDDD. The study was prepared on the ethical principles of the Declaration of Helsinki. The informed consent form will contain extensive information about this trial including the purpose of the trial, the study design, potential risks and benefits associated with the trial and the participants’ rights and responsibilities.
Study design, setting and participant
This is a prospective observational study. All the patients for this study were performed at the pain management unit from May 2020 to May 2022 and satisfying the inclusion and exclusion criteria of the study.
The inclusion criteria were : 1) age ≥18 years old; 2) clinical lumbar radicular pain lasting more than 3 months. The clinical manifestation and lumbar disc herniation on the magnetic resonance imaging characteristic were relevant; 3) conservative treatment, which includes : anti-inflammatory medication, gabapentinoids (Gabapentin or Pregabaline), tricylic antidepressants (Amitryptiline) and physical therapy, no satisfactory improvement of symptoms after a 3-month strategy; and 4) pain level evaluation by the Numeric rating scale (NRS) ≥5.
The exclusion criteria for this audit were : 1) local infection, sepsis and bacteremia; 2) pregnancy; 3) coagulation disorder; 4) prior epidural injection in the past 3 months, such as nerve root injection and caudal injection; 5) spinal tumors or tuberculosis, spinal deformity, history of spinal surgery; 6) symptoms of severe nerve damage including motor paralysis, muscle atrophy, peripheral neuropathy, arterial vascular disease, malignancy and cauda equina syndrome; and 7) allergic to the drugs used in this study.
Study procedure
The procedure was performed at the operating theatre at.
It is quickly confusing to describe the painful area between physicians and patients, especially the contrast of the supine position in examination with the prone position in performance. Thus, the patients checked in advance which of the four regions made for the pain by the physicians before the procedure : 1) the skin front of the thigh and calf was encoded in region 1; 2) the outside of the thigh and calf was called region 2; 3) the skin back of the thigh and the calf was called region 3; and 4) the skin inside of the thigh was called region 4.
Symptoms of the L4 nerve causes pain in region 1 (without the presence of pain in the calf). The symptoms of the L5 radicular pain were described as pain at the region 2 of the thigh, calf and radiation to the first toe. Following this decree, S1 radicular pain was pictured as pain in the region 3 of the thigh, calf and radiation to the fifth toe. Before the performance, each patient was examined and encoded their pain area.
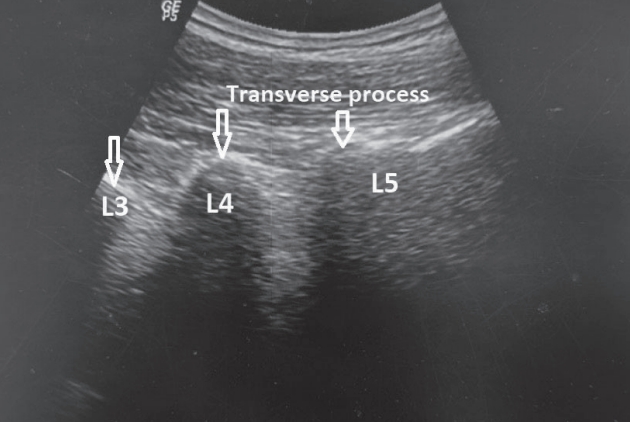
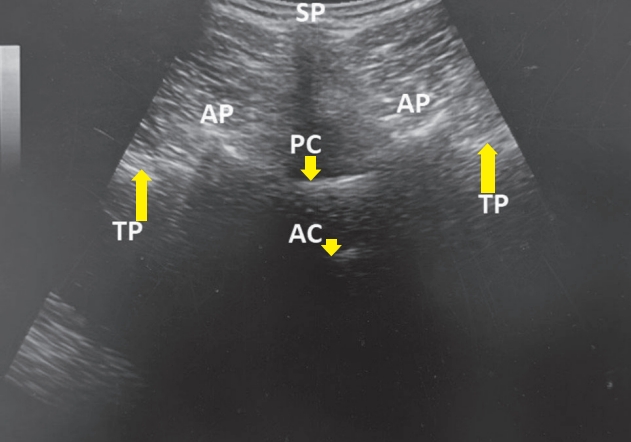
During the procedure, the needle was set alongside the nerve under US guidance. A standardized US-guided lumbar approach was utilized for pararadicular spinal injections by LOGIQ P5 (device signature P5 : 178256 SU4; GE Ultrasound Korea, Ltd, Seongnam, Korea). A 2-5 MHz convex probe and a prone position where required. In the beginning, the spinal level was first defined in a sagittal US image starting from the sacrum toward the cephalad spinous processes in median plane ( Fig. 1) and paramedian plane ( Fig. 2). At the target level, the probe was rotated 90° for a median transverse image as the “crown” sign ( Fig. 3). The transducer was then translated laterally at the respective spinal segment to see the spinous process and adjacent structures (vertebral arch lamina, zygapophyseal articulations, inferior and superior facets, transverse process and vertebral isthmus). The angle between the inferior edge of the basal portion of the transverse process and vertebral lamina, is considered the space where the spinal nerve is located. At 3-4 cm from the midline, we performed local anesthesia with lidocaine 1% and gently insert the 20-gauge tip cannula (RF cannula needle, length 100 mm or 150 mm with a 10 mm active tip; Cosman Medical, Inc., Burlington, VT, USA) in the direction passed skin at 45° angle using the “inplane” technique, until the tip targeted to the lateral side of the lamina ( Fig. 4). The position of the needle tip was examined by using the Stimulation Program of the Radiofrequency generator machine (Cosman G4; Cosman Medical, Inc.). The test is then performed while the patient is awake, using sensory stimulation at 50 Hz was initiated at 0.1 volts and slowly titrated up by increments of 0.1 volts until the patient could identify the stimulation (tingling, buzzing, vibration, or concordant pain). If the patient failed to perceive sensory stimulation at less than 0.5 volts, the lowest sensory stimulation testing was accepted after at least three attempts of adjusting electrode placement. Motor stimulation was then performed at 2 Hz to ensure proper positioning and avoid lesioning of the spinal motor nerve. When the needle tip was in the right place, the response caused by the stimulus is expected to intensify and radiation from the lumbar to the leg is like the patient’s pain area. The current stimulated response was called threshold current density. Then, the mixture of the 2 mL dexamethasone (4 mg/mL; Vinh Phuc Pharmaceutical Joint Stock Company, Vinh Phuc, Vietnam) and 2 mL bupivacaine 0.5% (Laboratoire Aguettant, Lyon, France) was injected into the pararadicular once for transforaminal epidural injections. Check vital signs during the procedure. Patients were evaluated after 2 hours of the procedure and discharged with advice to avoid too much bending, lifting heavy weights, or walking distances and asked to reexamine at 1 week, 1 month, 3 months, and 6 months. The NRS and Oswestry disability index (ODI) were recorded at all times. Neurological check-ups of the lower limb included motor examination in form tone, muscle strength, reflexes and sensory examination. During the period of recruitment (from May 2020 to May 2022), there were 85 eligible patients. Due to the COVID-19 pandemic and serious affection to Vietnam from May 2021, post procedural assessment has to stop because of isolation, four patients lost follow-up and three patients were operated on for discectomy after 1-3 months. Therefore, only 78 patients followed up on our 6-month study.
Measurement of outcome
Patients’ characteristics were gender, age and baseline data upon admission. The data were collected including the NRS and ODI for painful assessment before the procedure and after 1-week, 1-month, 3-month, and 6-month reexamination.
A 2-point or more decrease or 50% reduction on the NRS was deemed to represent clinically meaningful improvements in pain intensity. The ODI calculated 10 items including pain, individual function and personal comprehensive function. The minimum score for each item is 0 (good state), whereas the highest score is 5 (poor state). The ODI referred to the percentage of the sum of scores from all 10 items out of 50.
Data analysis
Mean, standard deviation, median, interquartile and frequency and percentage were used to describe the data. Chi-squared tests, Fisher’s exact tests and Paired-Sample T-tests were used to evaluate the association between patient characteristics and pain degree. All statistical tests were two-sided with a significance level of 0.05. Continuous data before operation with non-normal distribution were analyzed using the Mann-Whitney U-test. Data were analyzed using the SPSS ver. 25.0 (IBM Corp., Armonk, NY, USA) software.
RESULTS
Patients’ characteristics
There were 78 eligible patients. The mean age was 55.7±15.5 years old and the majority were male patients (40 males and 38 females). Before the procedure, the pain was assessed with a mean NRS was 7.33±1.04. According to ODI, there was 69.2% of patients with cripples. The pain area of all the patients was enrolled with 67 at L5-nerves (region 2), 36 at S1-nerves (region 3), and 22 at L4-nerves (region 1). Pain duration ranged from 6 months to the longest 54 months and the mean time was 17.9±6.5 months. The mean threshold of the stimulation current was 0.9±0.4 mA. Fifty-six patients (71.8%) detected the response threshold at 0.5-1 mA and 22 patients (28.2%) had a higher response threshold over 1 mA. The characteristics data of patients are presented in Table 1.
Effectiveness of transforaminal epidural injection with longitudinal data
The assessment by NRS 1 week after the procedure was significantly lower than before the injection at admission (T-test, p<0.001). Seventy-five patients (96.2%) achieved a 2-point or more decrease or 50% reduction on the NRS after 1 week post-procedural. This number was 74 (94.9%), 71 (91.0%), and 61 (78.2%) at 1, 3, and 6 months reexaminations, respectively. The NRS at 1-month, 3-month, and 6-month reexaminations showed a reduction versus the pre-intervention NRS ( Fig. 5). In terms of ODI, the score decreased at 1-week, 1-month, 3-month, and 6-month reexamination. The suffered cripple patients improved function early in the first week posterior performance (69.2% to 0%, T-test, p<0.001). The outcome measured by ODI are presented in Table 2.
Safety
The injection procedures were tolerable for all the patients. No patient experienced any complication such as an aggravation of the pain, numbness, headache, dizziness, or an allergic reaction. There was not any treatment-related complications after 6 months follow-up.
DISCUSSION
In Vietnam, this study was the first to investigate the effect of US and nerve stimulation guidance TESIs in the management of chronic lumbar radicular pain. Our findings showed a reduction of NRS from 7.33 before the procedure to 3.01 after one month and to 3.78 after a 6-month follow-up. We also found similar results compared to other studies. Wan et al. [ 20] studied on 46 patients with chronic lumbar radicular pain, the US-guided TESIs therapy was shown to cause significant pain reduction, measured using the Visual analogue scale. The sonographically guided pararadicular injections are feasible and effective in treating lumbar unilateral radicular pain. Guang-Hui et al. [ 10] investigated the efficacy of US-guided transforaminal nerve blocks in 60 patients with lumbar radicular pain. They found significant improvement in pain and function from baseline data to data obtained throughout the 3 months of the follow-up period. Meanwhile, our study approached transforaminal injection and still achieved a good outcome for short-term pain relief of the patients. We also noted the trend toward better outcomes based on ODI. In terms of ODI that indicated the level of disability, there were no cripple patients post-intervention after 1-month and 6-month follow-ups. Most patients had a better quality of life and even got back to work. The reduction of post-intervention analgesic consumption and ODI were reported in Omar’s research which studied the effect on 32 patients with radicular pain [ 15]. ODI decreased significantly after intervention up to 3 months compared to the pre-intervention value. Herniated discs can cause direct compression of the nerve root or posterior root ganglia and indirect compression of the blood vessels surrounding the nerve. Once the surrounding tissues and nerve roots are inflamed, a cascade of inflammatory mediators is produced, all of which activate afferent nerves, make the nerves very sensitive, and cause pain. TESI aims to deliver the drug directly to the damaged spinal nerve root. The most common is a mixture of local anesthetics and corticosteroids. Corticosteroids can inhibit the production and release of proinflammatory substances. Local anesthetics can inhibit the generation of action potentials, nerve impulses in response to harmful stimuli, and the transmission of painful stimuli to the brain [ 14, 17]. This is the first study to evaluate the effectiveness of double guidance TESIs in managing chronic lumbar radicular pain in Vietnam. Relief of symptoms and functional test have been the gold standard for evaluating the success of US-guided injection, with no serious complications in any of the patients. Lumbar epidural injections have commonly been used in the posterior median and paramedian approaches in local anesthesia. US-guided lumbar spinal injections have many benefits : elimination of radiation exposure; visualization of soft tissues, nerves and real-time needle advancement. Because of the immediate visibility of the target position, the needle could be advanced to the target structure in just a few seconds and under safe, real-time controlled conditions.
However, US-guided lumbar spinal injections are complicated techniques. Some factors might affect the US image quality of the spine and decrease needle visualization, such as obesity, osteophytes and degeneration in the elderly. Gofeld et al. [ 9] used a modified in-plane technique aiming at the vertebral body as a sonographic landmark and were the first to demonstrate the feasibility of the lumbar TESIs. The accuracy of the intraformational injection under US guidance was 91.3%. TESIs under US guidance had proved feasible, safe and wellaccepted by patients and intervention physicians due to the lack of radiation and real-time guidance [ 2, 17, 22]. The most important part of this procedure is to pinpoint the needle tip at the target nerve root. Previous studies needed FL or CT scan to confirm the needle tip. It means that the procedure still required a complex room and devices. In our study, electric stimulation has been seen to be sensitive to localize nerve. The higher the current intensity (mA), the greater probability of depolarization of an adjacent nerve. When the needle is placed closer to the nerve roots, less electrical current is needed to stimulate. Thus, there is a relationship between evoked nerve current intensity and the distance of the nerve-needle tip [ 4, 19]. We aim to achieve the appropriate needle position next to the nerve without touching it. In a study by Vassiliou et al. [ 19], at a threshold ≤0.2 mA, the needle tip seems to be intra-neural. For transforaminal epidural injections, the threshold current intensity between 0.5 and 2.0 mA is known associated with a sufficiently small distance from the nerve to the needle so that steroid and local anesthetic injections would work [ 5, 19]. In our study, there were 117 nerves had been stimulated with the same lumbar radicular pain at the threshold from 0.5 to 1.0 mA. Eight S1 nerves were stimulated at the threshold over 1.0 mA and less than 2.0 mA. All these patients had a 50% reduction in the NRS reduced NRS at the 1-week, 1-month, 3-month, and 6-month assessments. And no major complications were reported during and after TESIs. This result suggests that the current intensity between 0.5 and 2 mA could be used as a firm solution to TESIs. The effectiveness of this method is based on not only the precise localized needle tip by double guidance but also the re-judgment of the level of the injured nerve by comparing the patient’s pain area and stimulation. In previous studies, there are the similar result on effectiveness and safety of high amplitude over 2.0 mA in the guidance for the TESIs. In our study, there was no nerve required the current intensity more than 2.0 mA. Thus, we did not suggest stimulating the current intensity of more than 2.0 mA as the studies conducted by Kim et al. [ 11] and Emami et al. [ 4]. We used a nerve stimulator guidance to improve needle trajectory success and target position correction in US-guided TESI. Our study suggested that a nerve stimulator guidance can help us as an additional guide for successful US-guided TESI. Some authors also used US and electrical stimulation as a guide to TESI, a safe, accurate, and successful strategy for relieving patients with lumbar radicular pain [ 4, 11, 16]. In this study, since patients were monitored in 6 months so only short-term outcome was assessed. Especially, NRS and ODI increased at the 6-month examination versus the result at the 1-week and 1-month. This point can be explained by the short duration of steroid and anesthesia action. Therefore, our study did not find long-term outcomes for pain relief.
There are some limitations in this study. First, there was no definitive control group; neither the patient nor the doctor was blinded. This design was not chosen because the patient suffered from severe pain and using a placebo was considered unethical. Second, the study was from a single center. Third, data were affected by patients who lost contact during follow-up. The long-term effects of this procedure require a more significant number of studies in the future.
CONCLUSION
The result suggests that a combination of US and nerve stimulator guidance in TESIs is safe, reliable, accurate and effective for short-term and mid-term management of chronic lumbar radicular pain. It is a promising technique and has shown good results in providing short-term relief of pain.
Fig. 1.
Ultrasound view in median sagittal plane. 
Fig. 2.
Ultrasound view in paramedian sagittal plane. 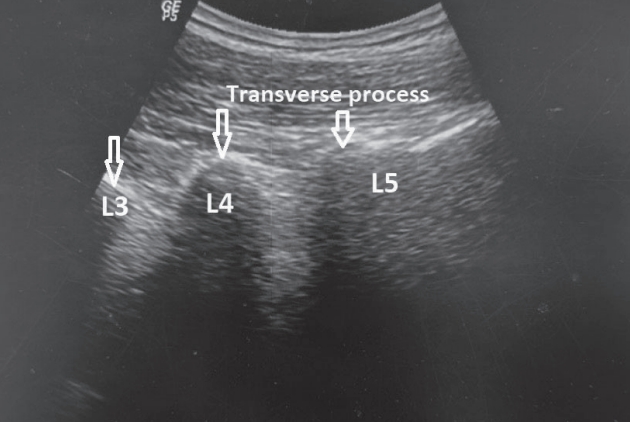
Fig. 3.
“Crown sign” on axial plane. Arrows indicate ultrasound view in axial plane. SP : spinous process, AP : articular process, TP : transverse process, PC : posterior complex, AC : anterior complex. 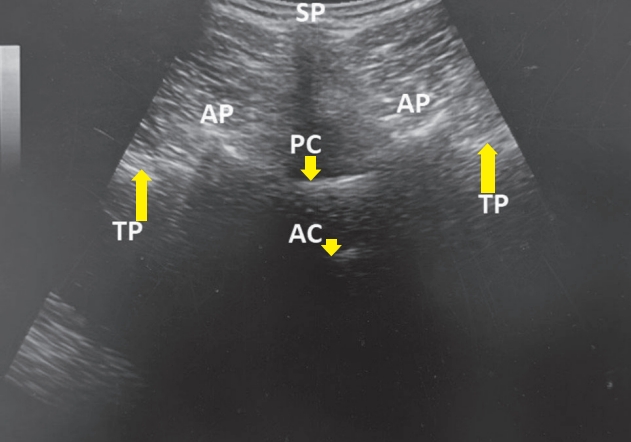
Fig. 4.
“In-plane” technique. SP : spinous process. 
Fig. 5.
Outcome measured by Numeric rating scale (NRS). 
Table 1.
The patients’ demographic and clinical characteristics
|
Characteristic |
Value (n=78) |
|
Age (years) |
55.7±15.5 (36-74) |
|
Sex, M/F |
40/38 |
|
NRS |
7.33±1.04 |
|
ODI |
|
|
21-40% |
0 |
|
41-60% |
30.8 |
|
61-80% |
69.2 |
|
81-100% |
0 |
|
Level nerve root pain |
125 |
|
L4 |
22 |
|
L5 |
67 |
|
S1 |
36 |
|
Pain duration (months) |
17.9±6.5 (6-54) |
|
The threshold current intensity (mA) |
0.9±0.4 (0.5-2) |
Table 2.
Outcome measured by Oswestry disability index
|
Time (n=78)
|
|
Baseline |
1-week |
1-month |
3-month |
6-month |
|
Level of disability |
|
|
|
|
|
|
Minimal (0-20) |
0 |
73.2 |
76.9 |
72.8 |
71.8 |
|
Moderate (21-40) |
0 |
17.9 |
19.2 |
23.1 |
19.2 |
|
Severe (41-60) |
30.8 |
8.9 |
3.9 |
5.1 |
9.0 |
|
Cripple (61-80) |
69.2 |
0 |
0 |
0 |
0 |
|
Bed-bound (81-100) |
0 |
0 |
0 |
0 |
0 |
|
p-value (T-test) |
|
<0.001 (19.35) |
<0.001 (22.93) |
<0.001 (20.70) |
<0.001 (19.06) |
References
1. Ballantyne JC, Sullivan MD : Is chronic pain a disease? J Pain 23 : 1651-1665, 2022   3. Chen S, Chen M, Wu X, Lin S, Tao C, Cao H, et al : Global, regional and national burden of low back pain 1990-2019: a systematic analysis of the Global Burden of Disease study 2019. J Orthop Translat 32 : 49-58, 2022   5. Gadsden JC : The role of peripheral nerve stimulation in the era of ultrasound-guided regional anaesthesia. Anaesthesia 76 Suppl : 65-73, 2021   6. GBD 2021 Low Back Pain Collaborators : Global, regional, and national burden of low back pain, 1990-2020, its attributable risk factors, and projections to 2050: a systematic analysis of the Global Burden of Disease Study 2021. Lancet Rheumatol 5 : e316-e329, 2023   7. Ghahreman A, Ferch R, Bogduk N : The efficacy of transforaminal injection of steroids for the treatment of lumbar radicular pain. Pain Med 11 : 1149-1168, 2010   8. Ghai B, Bansal D, Kay JP, Vadaje KS, Wig J : Transforaminal versus parasagittal interlaminar epidural steroid injection in low back pain with radicular pain: a randomized, double-blind, active-control trial. Pain Physician 17 : 277-290, 2014   9. Gofeld M, Bristow SJ, Chiu SC, McQueen CK, Bollag L : Ultrasound-guided lumbar transforaminal injections: feasibility and validation study. Spine (Phila Pa 1976) 37 : 808-812, 2012  10. Guang-Hui L, Guang-Yu Z, Yu-Zhang L, Yong-Tao Z, Shi-Min Z, Jiao J : Value of ultrasound-guided transforaminal nerve block in the treatment of lumbar disc herniation. J Int Med Res 48 : 300060520910910, 2022   11. Kim DH, Lim CH, Heo JY, Jang YJ, Choi YS : Feasibility of nerve stimulator as a supplemental aid for lumbar transforaminal epidural block. Clin Orthop Surg 6 : 324-328, 2014    12. Kreiner DS, Hwang SW, Easa JE, Resnick DK, Baisden JL, Bess S, et al : An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J 14 : 180-191, 2014   13. Last AR, Hulbert K : Chronic low back pain: evaluation and management. Am Fam Physician 79 : 1067-1074, 2009  14. Manchikanti L, Knezevic NN, Navani A, Christo PJ, Limerick G, Calodney AK, et al : Epidural interventions in the management of chronic spinal pain: American Society of Interventional Pain Physicians (ASIPP) comprehensive evidence-based guidelines. Pain Physician 24 : S27-S208, 2021  15. Omar S, Hegab SES, Reda MIS, El-Karadawy SA, Saad MM, El Sekily NM, et al : Ultrasound-guided fluoroscopic-verified trans-foraminal lumbar dorsal root ganglion pulsed radiofrequency modulation for radicular pain relief: clinical and cadaveric evaluation of the technique. Egypt J Radiol Nucl Med 52 : 41, 2021   16. Sato M, Simizu S, Kadota R, Takahasi H : Ultrasound and nerve stimulation-guided L5 nerve root block. Spine (Phila Pa 1976) 34 : 2669-2673, 2009   18. Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al : Chronic pain as a symptom or a disease: the IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain 160 : 19-27, 2019  19. Vassiliou T, Müller HH, Limberg S, De Andres J, Steinfeldt T, Wiesmann T : Risk evaluation for needle-nerve contact related to electrical nerve stimulation in a porcine model. Acta Anaesthesiol Scand 60 : 400-406, 2016   21. Wang D : Image guidance technologies for interventional pain procedures: ultrasound, fluoroscopy, and CT. Curr Pain Headache Rep 22 : 6, 2018    22. Yang G, Liu J, Ma L, Cai Z, Meng C, Qi S, et al : Ultrasound-guided versus fluoroscopy-controlled lumbar transforaminal epidural injections: a prospective randomized clinical trial. Clin J Pain 32 : 103-108, 2016 
|
|