INTRODUCTION
Cleidocranial dysplasia (CCD) is a rare autosomal dominant disorder characterized by generalized dysplasia of the osseous and dental tissues. This condition is caused by mutation in the core-binding factor alpha 1 (CBFA1) gene, a transcription factor that activates differentiation of the osteoblasts3,910). An estimated prevalence rate for CCD is one per million4). CCD affects not only the clavicles and the skull but also the entire skeleton. The primary pathogenesis of CCD is defective midline ossification. This causes patent anterior fontanelle, metopic suture, wormian bones, cleft palate, and hypoplastic or absent clavicle4,9). In this report, these authors summarized a successful cranioplasty with the modified split calvarial graft technique utilized for a patient with CCD, who had been concerned about the undesirable esthetic appearance of his head.
CASE REPORT
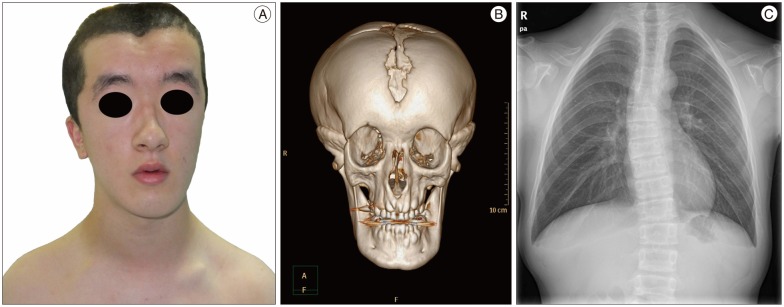
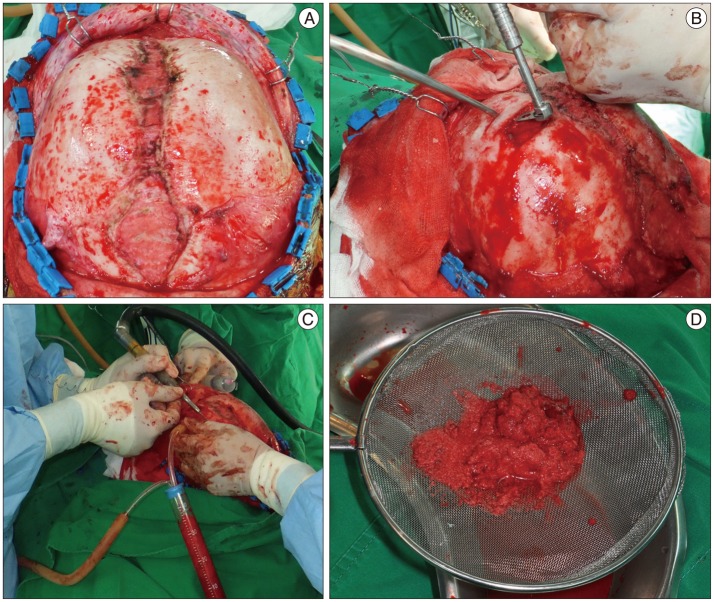
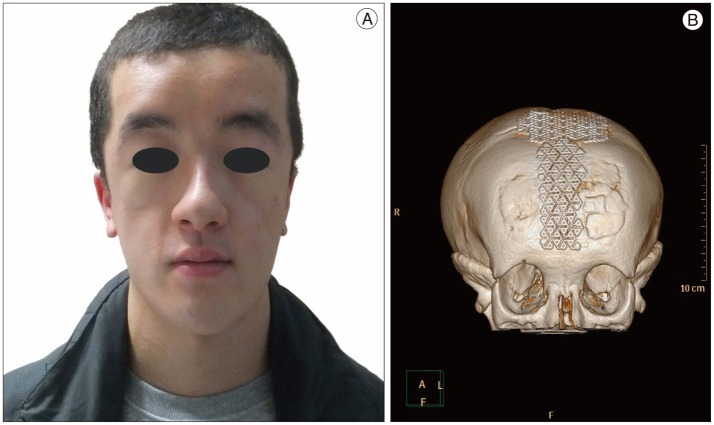
An 18-years old male visited our outpatient department with a complaint of cosmetic problems of his head. Apparently, he has a short stature and a large head with brachycephalic manifestation together with a midline forehead groove, including a depression of the anterior fontanelle and a depressed nasal bridge, some degree of hypertelorism with exophthalmos, and a small maxilla. This gave rise to a face with a small, flattened appearance with mandibular prognathism (Fig. 1A). His mother and older brother had a similar appearance just like him. His development and level of intelligence were normal. A 3-dimensional computed tomography (CT) revealed an opened anterior fontanelle, sagittal and metopic suture, and downward curvature of the zygomatic arch with maxillary hypoplasia (Fig. 1B). His thoracic cage was small and bell-shaped. Chest radiography showed a cone-shaped thorax and hypoplasia of the bilateral clavicles (Fig. 1C). Following clinical and radiographic examination, a cranioplasty was done. The surgical field was accessed with a bicoronal skin incision. The scalp and the periosteum were retracted anteriorly and the midline calvarial defect area on the metopic suture was exposed. After further fine dissection, the anterior fontanelle was also exposed with a posterior retraction of the midline scalp flap (Fig. 2A). After complete elevation of the pericranium around the skull defect areas, the modified split calvarial graft technique was applied. The outer table flaps were gained with a thin cutting tool (Midas Rex Legend EHS Stylus High-Speed Surgical Drill, Medtronics, Fridley, MN, USA) from the bilateral frontal bossing areas, where the bone was thick enough to be split into the outer and inner table flaps (Fig. 2B). This thin cutting tool could minimize bone losses while splitting the craniotomy flap. The bone flour was collected with a bone collector (a widely used generalized sputum collector which was connected to the intraoperative closed suction system) during bone sawing (Fig. 2C, D). After obtaining these multiple rectangular-shaped outer tables from the bilateral frontal bossing bones, these tables were put on to the skull defect areas. Then, the obtained bone flour (which had been collected by the aforementioned bone collector) and hydroxyapatite (HA) cement were molded together in the calvarial defect site. The areas filled-up with bone flaps and bone flour were covered with a tailored titanium mesh and low profile screws. The margins of the bone harvested area were smoothly drilled out with a high speed drill and filled up with HA cement and obtained bone flours for cosmesis (Fig. 3A, B). Finally, the results were satisfactory and the bone fusion was noticeable on the 6 month follow up brain CT scan (Fig. 4A, B).
DISCUSSION
CCD is a rare generalized skeletal dysplasia, which exhibits a defective endochondral and intramembranous bone formation. Typical features include hypoplastic/aplastic clavicles, a brachycephalic skull, patent sutures and fontanelles, midface hypoplasia, supernumerary teeth, a relatively short stature and other skeletal abnormalities3,49,10). These conditions are caused by mutations in the CBFA1 gene, a transcription factor that activates osteoblast differentiation3,910). An estimated prevalence rate for CCD is one per million. However, such low rate seems to be due to under-diagnosis of relatively modest medical problems1). It was reported that the intelligence of such a patient is normal in most cases4,9). Significantly in neurosurgery, CCD is an extremely rare cause of myelopathy in patient with atlantoaxial subluxation. Kobayashi et al.7) asserted in their recent report of a atlantoaxial subluxation-induced myelopathy patient with CCD that neurosurgeon should be aware that atlantoaxial subluxation may be the cause of cervical myelpathy in patient with CCD. Calvarial defects largely occur from trauma, tumor, cysts, postoperative and congenital deformities. Cranioplasty indicated for patients with calvarial defects of various causes is a common and familiar surgical procedure for neurosurgeons. It can be simple or somewhat complicated. Cranioplasty tends to be slightly more difficult in case of a calvarial defect secondary to congenital disorder, as opposed to other cases. Tokuc et al.15) suggested in their recent report of CCD in a mother and her daughter cases that a protective helmet can be provided in early childhood, and craniofacial remodeling can be undertaken at a later age, when the final size and shape of the skull become apparent. Split calvarial graft is one of several cranioplasty techniques used for the reconstruction of different types of congenital calvarial defects. Calvarial bone graft was first described as an osteocutaneous vascularized flap in 189013). In the 1970s, Strong and Moulthrop14) reported the use of free outer table calvarial bone grafts that would be split calvarial grafts13). In recent years, the split calvarial graft is often applied for the repair of traumatic or congenital deformities for esthetic purpose in cranioplasty. Despite the risk of calvarial graft including intracranial hemorrhage, violation of the inner table or dura mater during harvest, the complication rate related to split calvarial graft is very low2,5). The thickest and safest area for outer table graft harvesting is the parietal bone1). In this case, the calvarial graft harvesting sites were bilateral frontal bossing areas where the bones were thick enough to be split for not only to get the calvarial grafts, but also to flatten the forehead for cosmesis. Recently, there are several kinds of artificial materials for cranioplasty. Nevertheless, the autogenous calvarium is considered to the most suitable material for reconstruction of cranial defects than other widely used artificial materials2,312). Kang et al.6) study, one of the very few investigations of cranioplasty for CCD in literature, reported a successful cranioplasty using only BoneSource (calcium phosphate cement; Stryker Leibinger Corp., Kalamazoo, MI, USA) in a rare case of CCD. A case similar to ours would be the McGuire et al.8) study, which reported a series of 7 cases of cranioplasty for adult patients with CCD. They had to flatten the bilateral frontal bossing region with a large ovoid carbide burr and those liberated bone chips were harvested. Then, these harvested bone chips were packed directly onto the deficient area and fixated underneath the titanium mesh with fibrin glue. They reported that these results were satisfactory. But, O'Broin et al.11) reported that an attempt to combine titanium mesh with bone dusts in cranioplasty was not successful, because there appeared to be complete resorption of bone dusts in the long term with virtually no evidence of new bone formation or in-growth. In this case, we performed a cranioplasty with titanium mesh and HA cement, collected bone flours (harvested during sawing of frontal bossing regions) and multiple rectangular shaped outer tables that would be a modified split calvarial graft technique.
CONCLUSION
When correcting a full-thickness congenital calvarial defect, neurosurgeons should try to achieve satisfactory results in not only the cosmetic aspect but structural durability. As shown in this case, the calvarial defect in patients with CCD could be successfully corrected with a modified split calvarial graft technique for cranioplasty. This approach would bring very satisfactory results for both patients and physicians.