Pituitary Stalk Hemangioblastoma in a von Hippel-Lindau Patient : Clinical Course Follow-Up Over a 20-Year Period
Article information
Abstract
Supratentorial hemangioblastomas (HBs) are rare, and pituitary stalk HBs are extremely uncommon; therefore, pituitary stalk evaluation is often overlooked. Herein, we report the development of pituitary stalk HB over a 20-year period and the importance of regular long-term follow up for patients with HBs.
INTRODUCTION
Hemangioblastomas (HBs) are benign vascular tumors of the central nervous system (CNS) that occur either sporadically (67-80% of cases) or as part of von Hippel-Lindau disease (VHL, 20-33% of cases)3,5,6). HBs originate most frequently in specific regions of the CNS (retina, cerebellum, brainstem, and spinal cord) and seldom occur in the supratentorial compartment of the CNS3). In a recent series, 11% of the HBs in VHL disease were developed in supratentorium, which is more than previously thought5). The natural course of supratentorial HBs has not yet been clarified due to a lack of reports based on a long follow-up period. Recently, a few reports have described the natural history of supratentorial HBs; however, the median length of imaging follow-up was less than 10 years5,7). We herein present a long-term progression of pituitary stalk HB over a 20-year follow-up period in a patient with VHL disease.
CASE REPORT
A 15-year-old boy was admitted to our hospital in 1990 with an one year history of intermittent headache and vomiting. A solitary hypervascular mass was demonstrated at the right cerebellum and was removed completely. Histologic finding was consistent with HB. There was no recurrence during a few years of follow-up. However, 7 years following the initial surgery, brain magnetic resonance image (MRI) showed a cystic mass with a mural nodule in the right cerebellar hemisphere and several small masses at the right cerebellopontine angle and left cerebellar vermis representing recurrence. Resection of the lesion was achieved, using suboccipital craniectectomy, and gamma-knife therapy was performed. Seventeen years following the initial surgery (2007), he developed progressive headache, dizziness and diplopia. At that moment, brain MRI revealed a homogeneous enhancing suprasellar mass (Fig. 1) and enlarged edematous optic chiasm (Fig. 2). Additionally, he was clinically diagnosed with VHL disease with numerous enhancing nodules and syringomyelia along the cervical and thoracic spine, multiple cysts in the both kidneys and the pancreas, and renal cell carcinoma in the lower pole of the right kidney. His endocrinological profile was normal. He subsequently received gamma-knife radiosurgery for pituitary and other residual lesions in the brain. Twenty-two years following the initial surgery (2012), he complained recurred dizziness and progressive diplopia. Brain MRI revealed an increased size of the pituitary mass (from 4.3×5 mm to 7×11.5 mm) and cerebellar masses, despite treatment. After the cerebellar lesion has been removed surgically, he was discharged and scheduled for further follow-up imaging and gamma-knife therapy because the patient's symptoms were subsided and the surgeon opted for observation.
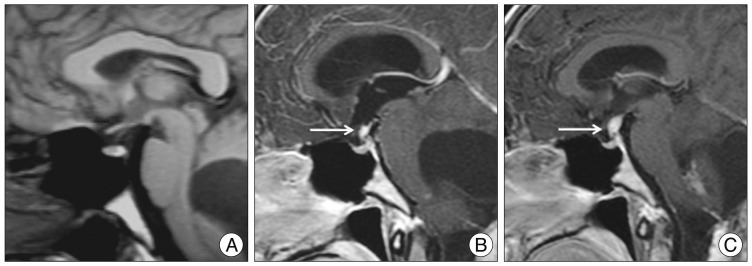
Serial magnetic resonance imaging (MRI) of a pituitary stalk hemangioblastoma. A : Sagittal T1-weighted MRI performed 8 years following original resection reveals a normal pituitary stalk. B : Contrast-enhanced sagittal T1-weighted MRI performed 17 years following the initial surgery shows a 5-mm pituitary stalk hemangioblastoma (arrow). C : Twenty-two years following the initial surgery, MRI demonstrates an increased size of the pituitary stalk mass (arrow).
DISCUSSION
Cerebellar HBs are the most common manifestation of VHL disease and are often multiple in nature3,4). Although cerebellar HBs are histopathologically benign, they show a degree of malignant clinical behavior in long-term follow up. Additionally, it is well documented that, despite complete removal of cerebellar HBs, further de novo or disseminated lesions may occasionally develop in VHL patients after intervals ranging from 6 months to 17 years (average, 7 years) after the initial diagnosis2).
With respect to the natural history of VHL disease, Wanebo et al.7) reported that HBs associated with VHL disease have two separate phases of growth : a rapid growth phase, which tended to be followed by a quiescent phase that can last for more than 2.5 years. They represented that 74% had tumors with one growth phase, whereas 26% had tumors with at least two growth phases7). In our case, the cerebellar HBs remained quiescent for about 7 years. However, recurrent cerebellar HBs developed, and subsequently, a pituitary stalk HB also occurred.
Peyre et al.5) focused on supratentorial HBs in VHL disease that were found mostly in the temporal and sellar regions where supratentorial lesions occur. Additionally, Lonser et al.3) demonstrated that 11% of all 250 VHL patients had supratentorial HBs, and 29% of the supratentorial HBs were located in the pituitary stalk. They revealed that the pituitary stalk is the most common site for development of supratentorial HBs in patients with VHL disease. The mechanism of pituitary dissemination of cerebellar HBs is unclear. No case of de novo development of disseminated HBs without previous surgery has been reported, strongly suggesting the spread and spillage of tumor cells through the cerebrospinal fluid (CSF) space. Most of the recurrent masses are located in the infratentorial area, and the paucity of supratentorial lesions may reflect CSF flow and the effect of gravity, supporting the hypothesis of tumor spread through the CSF pathway2). Thus, it is important to minimize tumor cell spillage to the supratentorial area during procedures, and surgeons and radiologists should consider the possibility of supratentorial dissemination, including the pituitary stalk of cerebellar HBs.
Hemangioblastomas occur predominantly in adults aged 30-40 years. However, our case demonstrated cerebellar HBs in a 15-year-old male, younger than the reported predominant age. He underwent a very long-term follow-up over 20 years, and a pituitary stalk HB developed 17 years after the initial HB diagnosis. An increased size of a pituitary stalk HB was found during a 22-year follow-up period, despite radiotherapy. He had diplopia related to an edematous optic chiasm, and might represent blockage of vein backflow. Despite visual symptoms, he was treated with only radiosurgery. Optimal surgical timing and treatment of choice were poorly defined. Lonser et al.3) sought asymptomatic pituitary stalk HBs that do not require treatment. Surgery can be reserved until associated signs or symptoms occur. However, Peyre et al.5) supported the idea that the main indication for surgery is asymptomatic growth of either the tumor or the cyst. Additionally, previous studies of HBs have demonstrated highly variable growth patterns; however, all increased in size over time5,7). Furthermore, some previous reports indicated that complete resection of pituitary stalk HBs often produces panhypopituitarism; thus, some controversy exists regarding the surgical strategy in pituitary stalk HB patients.
HB is generally a radio-resistant tumor, and high-dose radiation therapy for numerous lesions scattered throughout the CNS is difficult1,2). Medications, such as interferon-alpha, thalidomide, or vascular endothelial growth factor receptor antagonists to inhibit angiogenesis, did not result in remarkable tumor treatment2). Thus, HBs associated with VHL disease usually continue to occur over the course of the life of the patient, which necessitates life-long surveillance2). Additionally, multiple growth pattern of HBs was established7). Patients may need to be monitored more frequently during intervals of tumor enlargement. Serial MRI, visual field testing and clinical and laboratory endocrinological follow-up of pituitary stalk tumors are important to detect potential enlargement. Furthermore, the optimal timing and strategy of surgery have not been determined; these depend on the ability to cure these tumors while preserving pituitary function. Based on previous and our reports, close, long-term follow up is necessary to monitor the recurrence or dissemination of cerebellar HBs. Moreover, supratentorial evaluation is mandatory, particularly for pituitary stalk tumors irrespective of the presence of symptoms.
Acknowledgements
A special thank you goes to those who contirubuted to this paper : Especially Prof. Kim for his valuable comments and sharing his knowledge.
