Difference of Sagittal Spinopelvic Alignments between Degenerative Spondylolisthesis and Isthmic Spondylolisthesis
Article information
Abstract
Objective
The purpose of this study was to analyze the differences of spinopelvic parameters between degenerative spondylolisthesis (DSPL) and isthmic spondylolisthesis (ISPL) patients.
Methods
Thirty-four patients with DSPL and 19 patients with ISPL were included in this study. Spinopelvic parameters were evaluated on whole spine X-rays in a standing position. The following spinopelvic parameters were measured : pelvic incidence (PI), sacral slope, pelvic tilt (PT), lumbar lordosis (LL), and sagittal vertical axis from C7 plumb line (SVA). The population of patients was compared with a control population of 30 normal and asymptomatic adults.
Results
There were statistically significant differences in LL (p=0.004) and SVA (p=0.005) between the DSPL and ISPL group. The LL of DSPL (42±13°) was significantly lower than that of the control group (48±11°; p=0.029), but that of ISPL (55±6°) was significantly greater than a control group (p=0.004). The SVA of DSPL (55±49 mm) was greater than that of a control group (<40 mm), but that of ISPL (21±22 mm) was within 40 mm as that of a control group. The PT of DSPL (24±7°) and ISPL (21±7°) was significantly greater than that of a control group (11±6°; p=0.000).
Conclusion
Both symptomatic DSPL and ISPL patients had a greater PI than that of the asymptomatic control group. In conclusion, DSPL populations are likely to have global sagittal imbalance (high SVA) compared with ISPL populations because of the difference of lumbar lordosis between two groups.
INTRODUCTION
In the past, the treatment for spinal disease was focused on regional problem, as a neural decompression and obtaining a bony fusion. As spinal surgery techniques have developed, a concept about whole spinal alignment has been emphasized as important for managing spinal disease. Spinopelvic (lumbosacral pelvic junction) alignment is very important in understanding the overall alignment of the spine. And, it is a considerable factor, especially when performing lumbar fusion surgery. Sagittal alignment of the spine has been investigated in many studies, primarily in the normal population8,20). In the normal population, the correlation between pelvic incidences, sacral slope and lumbar lordosis have been well documented3,11,19). Also, several studies have reported sagittal alignment in populations of patients with low back pain7-9), degenerative spondylolisthesis (DSPL)1,12,20), and isthmic spondylolisthesis (ISPL)6,14). Recent studies suggested a predominant role of spinopelvic parameters to explain lumbosacral spondylolisthesis pathology.
DSPL and ISPL are commonly seen by clinicians and require fusion surgery to be considered for sagittal spinopelvic alignment. Thus, understanding the characteristics of the spinopelvic parameters of DSPL and ISPL are very important for spine surgeons. The interesting thing is that the characteristics of the spinopelvic parameters of DSPL and ISPL are different although the overall same spondylolisthesis. Most studies have reported the spinopelvic parameters of the DSPL and ISPL population as compared with the normal population, separately. There were few studies about the difference in spinopelvic parameters between DSPL and ISPL. The purpose of this study was to demonstrate the differences in spinopelvic parameters between the DSPL and ISPL population. And each group compared with a control group without low back pain, respectively.
MATERIALS AND METHODS
Patients' population
We assessed 53 spondylolisthesis patients who were treated with lumbar interbody fusion in our hospital from January 2008 to September 2010; 34 patients with DSPL and 19 patients with ISPL. The DSPL group consisted of 6 men and 28 women, and the ISPL group consisted of 3 men and 16 women. The mean age was 65.7 years (range, 45-80 years) and 54.0 (range, 36-71 years) in the DSPL and ISPL group, respectively. According to the Meyerding's classification13), 25 DSPLs were grade I (5-25%) and 9 were grade II (25-50%); and 15 ISPLs were grade I and 4 were grade II. The involved levels for the DSPLs were L3-4 in 4 patients (11.8%), L4-5 in 22 patients (64.7%), and L3-4 and L4-5 in 8 (23.5%). Those for ISPLs were L4-5 in 9 (47.3%), and L5-S1 in 10 (52.6%) (Table 1).
All patients had symptoms unresponsive to conservative treatment for at least 6 months. Patients were excluded from the study if they had one or more of the following criteria, according to clinical and/or radiological data : history of any spinal surgery, including a lumbar discectomy; pathologic spinal disease (trauma or tumor); scoliosis; femoral pathology. Normal asymptomatic adults who were in a recently published study were set as the control population14). The control populations had no history of severe back pain or spine trauma, and consisted of 17 males and 13 females with an average age of 34.3 years (range, 28-42 years).
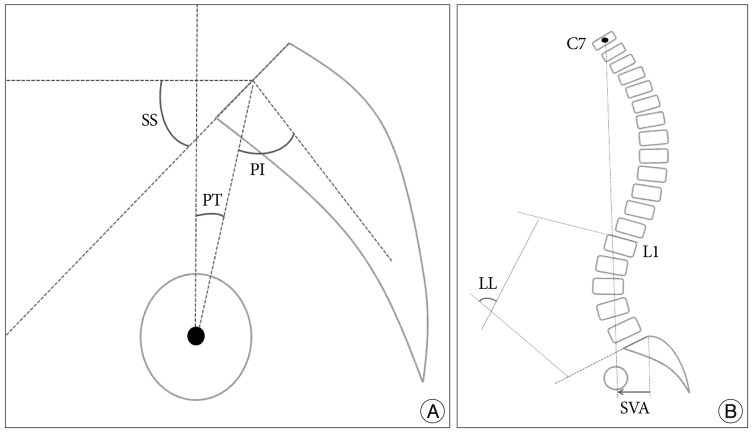
Spinopelvic parameters
Spinopelvic parameters were measured on a whole spine lateral radiograph (14×36 inch) with the hips and knees extended in a standing position after at least 5 minutes of walking. The following radiographic parameters were measured : pelvic incidence (PI), sacral slope (SS), pelvic tilt (PT), lumbar lordosis (LL), and sagittal vertical axis from C7 plumb line (SVA). PI is defined as the angle between the perpendicular to the upper sacral endplate at its midpoint and the line connecting this point to the femoral head axis. This is a morphologic parameter, considered as a constant, independent of the spatial orientation of the pelvis. The SS is defined as the angle between the horizontal and the upper sacral endplate. This is a positional parameter, varying according to the pelvis position. The PT is defined by the angle between the vertical and the line through the midpoint of the sacral plate to the femoral head axis; this is also a positional parameter. LL is defined as the angle between the upper L1 endplate and the upper sacral endplate. The SVA is defined as the horizontal offset from the postero-superior corner of S1 to the C7 plumb line (Fig. 1).
Statistical analysis
Statistical analysis was performed using SPSS software (version 12.0; 2003; SPSS, Inc., Chicago, IL, USA). The Mann-Whitney U test was employed for analysis differences in non-categorical variables between the two groups. The overall differences of sagittal spinopelvic parameters between the DSPL and ISPL groups were statistically analyzed. And, subgroups were divided in each of the groups according to the PI value (normal PI; 40<PI<60, high PI; PI≥60), and SVA value (normal SVA; SVA<40 mm, high SVA; SVA≥40 mm). The differences of spinopelvic parameters between the subgroups were statistically analyzed, respectively. Statistical p-values less than 0.05 were considered statistically significant.
RESULTS
Two spinopelvic parameters had significant statistical differences between the DSPL and ISPL group; LL (p=0.004) and SVA (p=0.005). The LL of DSPL group (42±13°) was significantly lower than that of the ISPL group (55±6°). The SVA of the DSPL group (57±49 mm) was significantly greater than that of the ISPL group (21±22 mm) (Fig. 2).
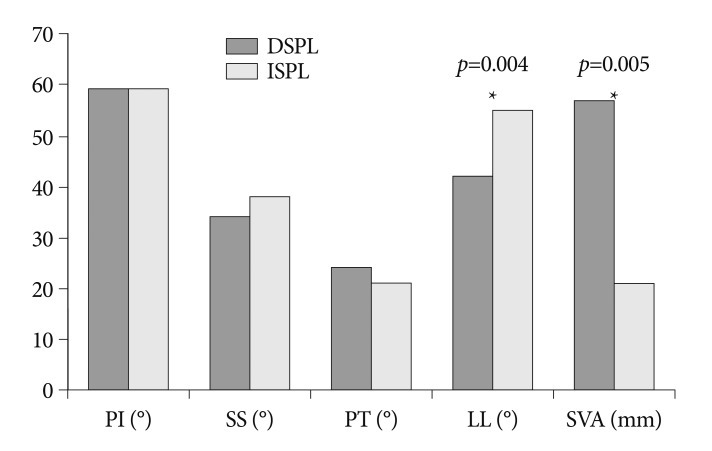
The comparison of spinopelvic parameters between DSPL and ISPL. Lumbar lordosis (LL) and sagittal vertical axis from C7 plumb line (SVA) had statistically significant differences between the DSPL and ISPL group. *This is significantly (p<0.05) different between groups by the Mann-Whitney U test. DSPL : degenerative spondylolisthesis, ISPL : isthmic spondylolisthesis, PI : pelvic incidence, SS : sacral slope, PT : pelvic tilt.
For the analysis with a control group, the PI was significantly greater for patients with DSPL (59±9°) and ISPL (59±13°) compared with a control group, respectively (49±9°) (p=0.000). The SS was significantly lower for patients with DSPL (34±7°) than that of the control group (38±7°) (p=0.023). The PT of DSPL (24±7°) and ISPL (21±7°) was significantly greater than that of the control group (11±6°; p=0.000). The LL of DSPL (42±13°) was significantly lower than that of the control group (48±11°; p=0.029), but that of ISPL (55±6°) was significantly greater than the control group (p=0.004). The SVA of DSPL (55±49 mm) was greater than that of the control group (<40 mm), but that of ISPL (21±22 mm) was within 40 mm of that of the control group (Table 2).
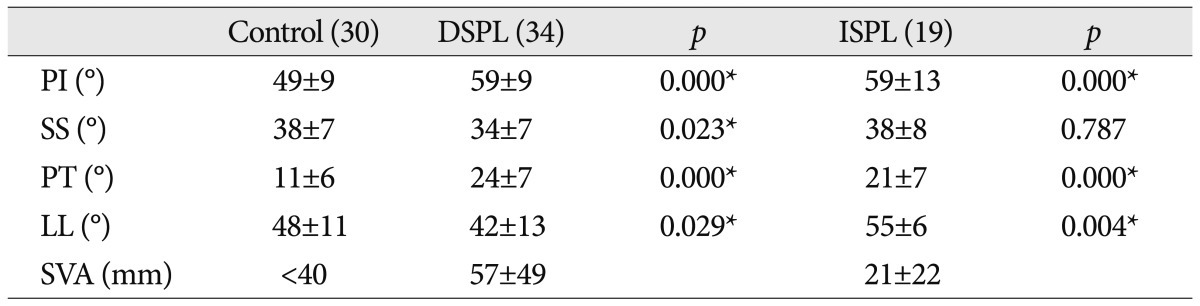
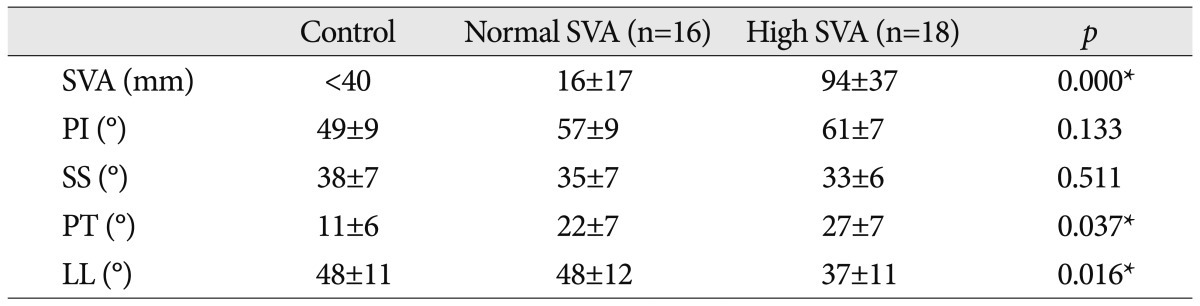
Comparison of spinopelvic parameters between the control and DSPL, between the control and ISPL groups
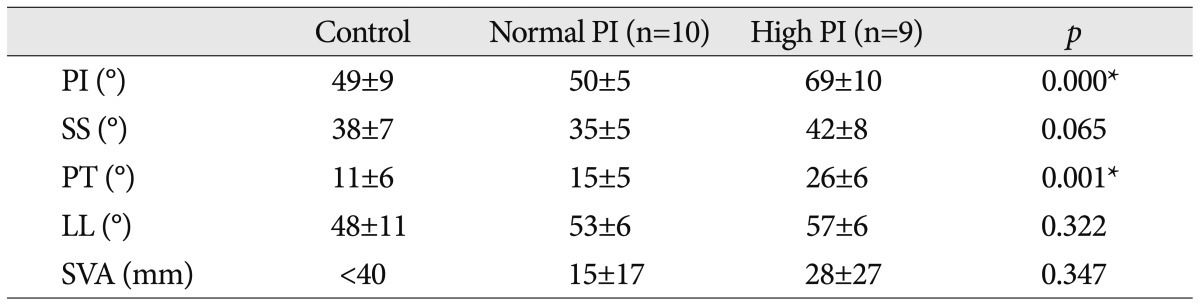
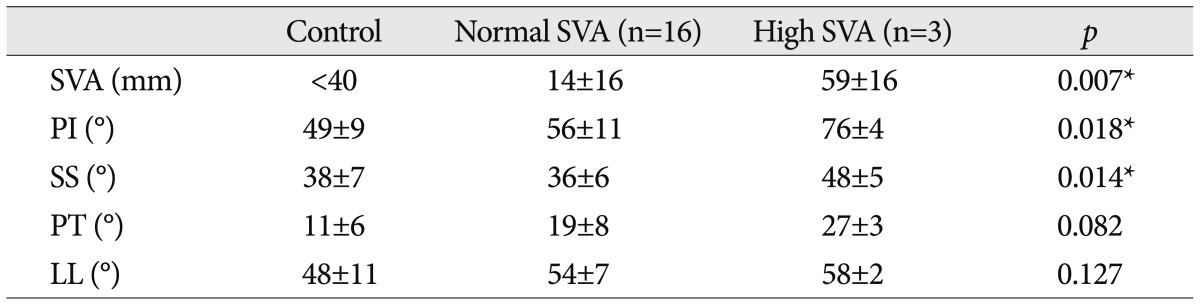
The DSPL group was divided 16 high PI (66±6°) and 18 normal PI (52±4°) populations according to the PI value (p=0.000). The SS (p=0.001) and PT (p=0.006) of the high PI group was significantly greater than that of the normal PI group (Table 3). The DSPL group was divided into 16 normal SVA and 18 high SVA populations according to the SVA value (p=0.000). The PT (p=0.037) of the high SVA group was significantly greater than that of normal the SVA group, and the LL (p=0.016) of the high SVA group was significantly lower than the normal SVA group (Table 4). The ISPL group was divided into 9 high PI and 10 normal PI populations according to the PI value (p=0.000). The PT (p=0.001) of the high PI group was significantly greater than that of the normal PI group (Table 5). The ISPL group was divided into 16 normal SVA and 3 high SVA populations according to the SVA value (p=0.007). The PI (p=0.018) and SS (p=0.014) of the high SVA group was significantly greater than that of the normal SVA group (Table 6).
DISCUSSION
Spinopelvic parameters
Recently, it has been recognized that the orientation of the lumbosacral pelvic junction plays a critical role in the overall alignment of the spine, and that sagittal spinopelvic balance is made from spinal and pelvic parameters. Many studies have reported spinopelvic parameters in normal and low back pain populations5,7,9,16,17,19). PI is an important anatomic parameter that describes the anatomic configuration of the pelvis and greatly influences the sagittal configuration of the spine4,10,11). It is relatively constant during childhood. Thereafter, PI increases significantly during adolescence until reaching its maximum value in adulthood10). It is not affected by posture or the pelvic position, and is considered to be invariable at the end of growth2). PI represents the algebraic sum of the SS and the PT : PI=SS+PT. Thus, if we consider the PI of any subject, when the sacral slope increases, the pelvic tilt decreases, and vice versa. It is commonly reported as a compensatory mechanism : when the trunk inclines anteriorly (e.g., age related change, sagittal imbalance, loss of lordosis, increase of kyphosis) a subject will try his/her best to maintain an economic posture and keep the spine balanced. Also, the morphology of the pelvis as quantified by PI is a strong determinant of the spatial position of the pelvis in a standing position : as the PI increases, so does the SS, PT or both. Values and correlations of spinopelvic parameters for the normal population have been well established. Legaye et al.11) and Vaz et al.19) have demonstrated a correlation between PI and LL in normal subjects; a low PI is usually associated with a low lumbar lordosis, whereas a high PI is usually associated with a high lumbar lordosis. Also, the correlation between LL and SS has been reported in normal populations; LL increases linearly with the SS18).
Degenerative spondylolisthesis versus isthmic spondylolisthesis
In the present study, patients with DSPL had a significant greater PI (59°) than the asymptomatic control populations (49°) (Table 2). It suggests that the shape of the pelvis, characterized by PI, is a predisposing factor for DSPL. In an asymptomatic normal population, it was demonstrated that patients with high PI had a high LL, and those with low PI had a low LL11,19). But, we observed that patients with DSPL demonstrated a low LL (42°), a low SS (34°), a high PT (24°) (pelvic retroversion), and a high SVA (57 mm) (anterior sagittal unbalance), compared with the control group. Also, analyzing between the high PI and the normal PI subgroup in the DSPL group, the SS and PT of the high PI subgroup was significantly greater than that of the normal PI subgroup, as a greater PI has a greater SS, PT. In spite of high PI, there was no significant difference in LL between high and normal PI subgroups. Additionally, the SVA (72 mm) of the high PI subgroup was greater than that (42 mm) of the normal PI subgroup, but, there was no significant difference (Table 3). For the analysis between the high SVA and normal SVA subgroup in the DSPL group, the PT (27°) of the high SVA subgroup was significantly greater than that (22°) of the normal SVA subgroup; the LL (37°) of the high SVA subgroup is significantly lower than that (48°) of the normal SVA subgroup (Table 4). It seems that the sagittal imbalance populations (high SVA subgroup) processed pelvic retroversion (increase of PT) as a compensatory mechanism, but did not overcome sagittal imbalance owing to the loss of lumbar lordosis (Fig. 3). These characteristics of spinopelvic parameters for DSPL can be described as the following phases. Initially, the patients with high PI would have had a high lordosis and high sacral slope. A high lordosis generates a large amount of force on posterior facet joints. As time goes on, these mechanical stresses on posterior facets cause and accelerate facet arthrosis. The posterior facets arthrosis associated with a significant inclination of the sacral slope predispose slipping. The slippage progresses to disc degeneration and collapse, and results in a loss of lordosis. This loss of lordosis induces a significant anterior displacement of the C7 plumbline and center of gravity. Thereafter, as a compensatory mechanism, patients with DSPL generate a decrease of SS associated with an increase of PT (pelvic retroversion)12) (Fig. 3). DSPL populations characterized by a high PI can have a greater potential to compensate global sagittal imbalance than populations with a low PI. Thus, the sagittal imbalance of DSPL is not severe and/or compensated1). But, as the loss of lumbar lordosis is even worse, sagittal imbalance can be more severe because of the limitation of compensation in pelvic retroversion.

Illustration showing the difference of sagittal spinopelvic alignment between DSPL (A) and ISPL (B). A : This illustration displays the sagittal spinopelvic alignment of DSPL. B : This illustration displays the sagittal spinopelvic alignment of ISPL. DSPL : degenerative spondylolisthesis, ISPL : isthmic spondylolisthesis, SVA : sagittal vertical axis from C7 plumb line.
There have been several studies about the characteristics of spinopelvic parameters for ISPL populations. Labelle et al.10) described that PI is significantly correlated with the degree of ISPL. Rajnics et al.15) noted that the SS, PT and PI in ISPL populations were significantly higher than those values in the normal populations. Moreover, Hanson et al.6) reported that as the degree of spondylolisthesis increased, the LL, PI and PT increased as well. In the present study, patients with ISPL also had a significantly greater PI (59°) than the asymptomatic control populations (49°), in the same way as DSPL. It also suggests that a high PI is a predisposing factor for ISPL. However, unlike the DSPL population, the ISPL population demonstrated a high LL (55°), a normal SS (38°), a high PT (21°), and the maintenance of a global sagittal balance within the normal range of SVA (21 mm), as compared to the control group. In an analysis between the high PI and the normal PI subgroup in the ISPL group, there were no significantly different parameters except for PT. The LL and SVA (57°, 28 mm) of the high PI subgroup was greater than those (53°, 15 mm) of the normal PI subgroup, but there were no significant differences (Table 5). A comparison between the high SVA and normal SVA subgroup in ISPL group revealed that the high SVA subgroup, as sagittal imbalance group, was only 3 populations, most (16 populations) of ISPL populations maintained the sagittal balance. The PI and SS (76°, 48°) of the high SVA subgroup was significantly greater than those (56°, 36°) of the normal SVA subgroup (Table 6). Generally, the ISPL group seems to maintain a sagittal balance, which can be caused by the maintenance of lumbar lordosis and is different from DSPL populations and mild pelvic retroversion (Fig. 3).
These comparative studies with the normal population were generally concordant with the present study. But, there were few studies for these differences of spinopelvic parameters between the DSPL and ISPL population. In our analysis between the DSPL and ISPL population, there were two statistically significant parameters; LL (p<0.05) and SVA (p<0.001) (Fig. 2). Based on the results of the analysis, the LL can be a considerable factor, because the SVA is a dependent variable. We can suggest that the characteristics of the spinopelvic parameters of ISPL that differ from DSPL are described as the following phases. Initially, the patients with high PI have a high lordosis and high sacral slope, which is same as DSPL. A high lordosis causes a high shear stress at the pars interarticularis, it develops spondylolysis and ISPL. To sum up, if mechanical stresses on the posterior column (pars interarticularis, facet joint) due to a high lordosis cause the defect of pars interarticularis (spondylolysis), ISPL can develop. After ISPL develops, lordosis is maintained or hyperlordosis is generated as a compensatory mechanism to maintain a global sagittal balance. Because mechanical stress is concentrated on the defect of pars interarticularis as a definite weak point, facet arthrosis and discopathy can relatively be less progressed than DSPL. In the analysis between ISPL and the control group, PT had a statistically significant difference. But, the PT of the ISPL population was less than those of the DSPL population (Fig. 2, Table 2). Also, mild pelvic retroversion is generated as a compensatory mechanism (Fig. 3).
There were several limitations in this study. First, it was difficult to evaluate a statistical significance due to a small number of cases and non-age, sex matched analysis. Second, this study did not include a high grade spondylolisthesis population. Third, the thoracic kyphosis of population was not evaluated in this study. Nonetheless, the results of this study are meaningful because the differences of sagittal spinopelvic alignments between DSPL and ISPL were investigated. But, we recognize that a prospective, larger and longitudinal study is necessary to clearly establish the spinopelvic alignments of DSPL and ISPL.
CONCLUSION
The pelvic incidence of both symptomatic DSPL and ISPL patients was greater than that of the asymptomatic control group. The DSPL population is characterized by a high sagittal vertical axis from the C7 plumb line, a loss of lumbar lordosis and high pelvic tilt (pelvic retroversion). On the contrary, the ISPL population has a high lumbar lordosis, normal sagittal vertical axis from C7 plumb line, and a mild increase of PT. In conclusion, DSPL populations are likely to be global sagittal imbalance compared with ISPL populations because of the difference of lumbar lordosis between two groups. These differences between DSPL and ISPL should be considered in surgical treatment.
Acknowledgements
This study was presented in an oral session at the annual spring meeting of the Korean Neurosurgical Society, 2011.