A Case Report of "Spinal Cord Apoplexy" Elicited by Metastatic Intramedullary Thyroid Carcinoma
Article information
Abstract
A 31-year-old man presented with acute onset of paraplegia. The patient's history was significant for thyroid carcinoma that had been treated 2 years earlier by thyroidectomy. A magnetic resonance imaging scan showed an enhancing intramedullary lesion at T7-8. Patient underwent surgical treatment and a tumor with hematoma was resected via posterior midline myelotomy. Postoperatively, the patient's motor weakness was improved to grade 3. The lesion showed typical histologic features consistent with papillary thyroid carcinoma. Early diagnosis and microsurgical resection can result in improvement in neurological deficits and quality of life of patients with an ISCM.
INTRODUCTION
Intramedullary spinal cord metastasis (ISCM) is a rare occurrence, and represents 8.5% of central nervous system metastases. ISCMs affect 0.1-0.4% of all carcinoma patients and comprise 1-3% of all intramedullary spinal cord neoplasms6-8). Generally, ISCMs arise from primary lung carcinoma, small cell carcinoma being the most common neoplasm, with the remainder originating from primary carcinomas of the breast, kidney, melanomas or lymphomas9). We report a novel case of an ISCM lesion which originates from a primary carcinoma involving the thyroid gland10).
CASE REPORT
A 31-year-old man presented with acute onset of paraplegia and hypesthesia below the umbilicus. The patient's history was significant for thyroid carcinoma that had been treated 2 years earlier with thyroidectomy.
On neurological examination, the patient presented with paraplegia which included a negative anal tone and showed positive signs of bilateral Babinski reflex. Sensory examination showed absence of pain, touch, vibration and temperature sense below the umbilicus. The remainder of the general physical examination was unremarkable. Laboratory evaluation, including full blood count, electrolytes, creatinine, liver function test, urine analysis and culture were unremarkable. However, thyroid function testing displayed a low TSH level because of previous thyroidectomy. The patient emergently underwent magnetic resonance imaging (MRI) of the spine, which showed a solitary 33 mm mass at the T7-8 level. The lesion appeared slightly hyperintense on T2 and iso signal intensity on T1-weighted images, enhancing homogeneously with intravenous contrast (Fig. 1). Initially, other intradural intramedullary tumors such as astrocytoma and ependymoma were considered. Although the patient's had a history of thyroid carcinoma that had been treated 2 years earlier with thyroidectomy, ISCM seemed an unlikely diagnosis, because the patient was young and there have not been any reported cases of ISCM associated with papillary thyroid carcinomas. With these study results, surgical exploration and excision of the mass was pursued. The patient underwent myelotomy via decompressive total laminectomy on T6, 7, 8 and tumor mass removal was accomplished. After myelotomy at the T7 level, a hematoma was identified. Below the T7 level, however, a dark-gray, yellowish mass that could be partially aspirated, indistinguishable from the surroundings, was identified. The lesion was dissected out and microscopically removed.
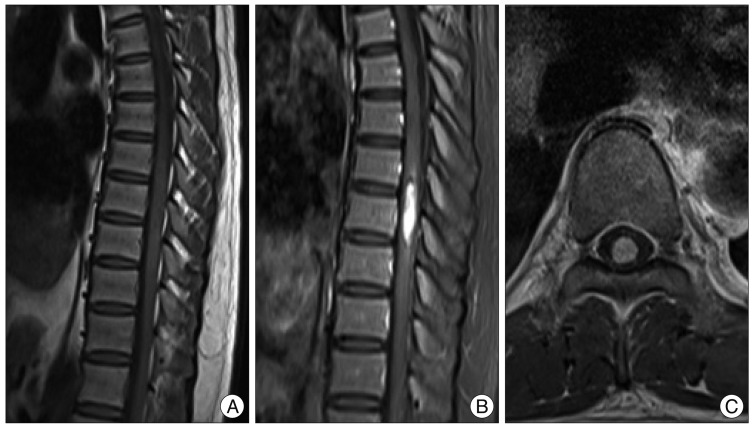
MRI scan of the thoracic spinal cord : sagittal (A) T1-weighted images, sagittal (B) and axial (C) gadolinium MRI of the thoracic spine showing a solitary mass in the intramedullary spinal cord at T7-8 level. The lesion showed a homogeneous enhancement following intravenous administration of gadolinium contrast.
Microscopically, the tumor showed a complex papillary pattern with invasion of the spinal cord. The papillae were lined by a layer of cuboidal to low columnar cells which had ground-glass nuclei, nuclear grooves and pseudoinclusions. Immunohistochemically, the tumor cells displayed diffuse positive staining for thyroglobulin and galectin-3. These findings are consistent with metastatic papillary carcinoma from the thyroid gland (Fig. 2). The patient progressively showed remarkable neurological recovery and after one week, motor power was improved to grade 3. He was referred to the general surgery department for recurrent thyroid carcinoma treatment.
DISCUSSION
ISCM is uncommon neoplastic lesions and account for 3-5% of cases of myelopathy in patients affected by carcinoma7). In the literature, lung carcinoma, especially small cell carcinoma, accounts for a majority of cases followed by breast carcinoma, melanoma, lymphoma, and renal cell carcinoma6,8,12,15). The mode of tumor spread to the spinal cord is not clear, but the autopsy findings suggest that intramedullary tumor may result from hematogenous spread via the arterial circulation. As many as 2% of patients in the end stage of disseminated cancer are found to have ISCM. MRI as diagnostic imaging technique has improved over time. It has become the gold standard for diagnosis and evaluation of rare tumors, hence the detection rate of ISCM is expected to increase. Presenting symptoms of ISCM usually consist of weakness, followed in frequency by sensory loss, pain and bowel and bladder disturbance. Weakness and pain present early, as compared to sensory loss, with sphincter disturbance having the latest onset12). Prognosis of ISCM is compounded by treatment modality and tumor type, with lung and breast metastases correlating with the shortest survival. Treatment of ISCM consists of immediate steroid bolus, radiation and chemotherapy with subtotal cytoreductive surgery and the treatment of choice is considered case by case17). High dose dexamethasone may allow for limited and transient neurological improvement, while radiotherapy often results in stasis of the deficit without improvement. However, in combination with chemotherapy, radiation correlates with an increased length of survival. Cytoreductive surgery is another treatment option for lesions early in the course of neurological deficits. It has not been found to increase the length of survival as compared to other treatment modalities.
Our report describes the case of a thoracic spinal cord lesion proven to be a metastasis from thyroid carcinoma10). In younger patients, both papillary and follicular carcinomas have a more than 97% cure rate if treated appropriately. Both papillary and follicular carcinomas are typically treated with complete removal of the thyroid lobe that harbors the carcinoma, in addition to the removal of most or all of the other side. Postoperatively, most, but not all, patients with thyroid carcinoma need radioactive iodine treatments after their surgery. Patients with medullary carcinoma usually do not need iodine therapy because medullary carcinoma almost never absorbs the radioactive iodine. Some small papillary carcinoma treated with a total thyroidectomy may not need iodine therapy as well. These carcinomas (medullary and some small papillary carcinoma) are often cured with simple (complete) surgical therapy alone3). Bleeding from thyroid carcinoma is uncommon. Anaplastic thyroid carcinoma (ATC) comprises only 1-3% of all thyroid neoplasm1,4). Bleeding from ATC is a rare, but potentially life-threatening complication requiring sophisticated intervention facilities which are not usually available at odd hours in emergency1). When present, distant metastasis occurs primarily in the lungs and to a lesser extent in the bones. The occurrence of metastatic lesions with hemorrhage arising from a primary thyroid carcinoma is extremely rare5). A few cases of lower gastrointestinal metastatic hemorrhage were reported, which were also associated with familial adenomatous polyposis14).
Spinal cord apoplexy is a hemorrhage occurring directly into the spinal cord. Spinal cord apoplexy may be due to traumatism, to changes in the coats of the blood-vessels, or to excessive blood-pressure. The clot may be as large as an almond, seldom larger, with the appearance dependent upon its age. When its occurrence is recent it will be red or dark in color, and they tend to change to brown or yellow with age. The clot may later become encapsuled by a fibrous deposit. There may be gliomatous tumors or acute myelitis involvement12). As this case, spinal cord apoplexy was induced by metastatic thyroid tumor bleeding. Spontaneous hemorrhage was presumably responsible for the acute progress of the myelopathy in our patient. Honma et al.10) reported a case of intramedullary metastasis of presumed poorly differentiated thyroid carcinoma associated with a hemorrhage caudal to the tumor, identical to the configuration demonstrated in our patient. It is almost impossible to make a positive diagnosis because the symptoms of hematomyelia are similar. Prompt diagnosis and urgent surgical treatment are needed when the patient has neurological symptoms. If the hemorrhage is small in quantity, absorption may speedily take place with complete recovery16). Prognosis depends upon the extent and location of the clot.
The prognosis of a patient who has an intramedullary cord lesion is grave, and treatment is mostly undertaken to relieve pain and to preserve or stabilize neurologic function. Medical and surgical interventions and radio-therapy have controversially been used as a therapeutic modality.
Advent of new surgical strategies including radiotherapy, would make an improvement for ISCM treatment modalities. Making an early diagnosis of ISCM could lead to a prompt decision of the necessity of major intervention. Providing patients with successful palliation and improving their quality of life demand multidisciplinary strategic treatment planning2,11,13).
CONCLUSION
ISCM is rare but after the advent of the MRI they are being encountered with increasing frequency. This is the fifth documented case of an intramedullary spinal cord metastatic lesion arising from a primary thyroid carcinoma and inter alia. It is second documented case of ISCM induced spinal apoplexy after 190510). Early diagnosis and microsurgical resection can result in improvement in neurological deficits and in the quality of life of patients with ISCMs.
