Migration and Coiling of Peritoneal Catheter into the Subgaleal Space: A Very Rare Complication of Subgaleoperitoneal Shunt
Article information
Abstract
Upward migration of the peritoneal catheter of a subgaleo-peritoneal (SP) shunt and coiling into the subgaleal space is an extremely rare complication of a SP shunt. A 32-year-old male patient visited our hospital presenting with a large skull defect due to a prior craniectomy performed elsewhere. The patient underwent a cranioplasty with methylmetacrylate, but subsequently developed progressive pseudomeningocele and subgaleal cerebrospinal fluid (CSF) collection. The patient underwent CSF diversion via a SP shunt. After SP shunting, the pseudomeningocele disappeared completely. Six months later, the patient presented with progressive scalp swelling. Skull X-ray showed migration and coiling of the distal catheter of the SP shunt. The patient was treated by removing the entire shunt catheter and the dura was covered with a subgaleal flap. We would like to report our experience with a very rare complication of subgaleo-peritoneal shunting.
INTRODUCTION
Subgaleo-peritoneal (SP) shunt is an alternative treatment for cranial pseudomeningocele5). The distal catheter of a SP shunt is placed using the same surgical procedures as in a ventriculoperitoneal (VP) shunt. Various complications related to VP shunts have been reported. Shunt failure due to infection or obstruction is a common complication. A very rare complication of SP shunts is the migration and coiling of the peritoneal catheter under the scalp9). We report a case of a 32-year-old man who developed complete migration and coiling of the distal catheter into the subgaleal space.
CASE REPORT
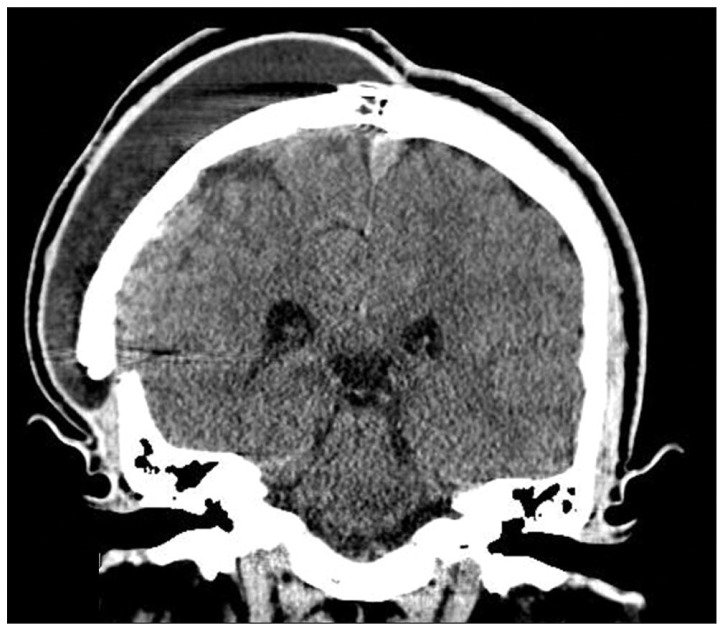
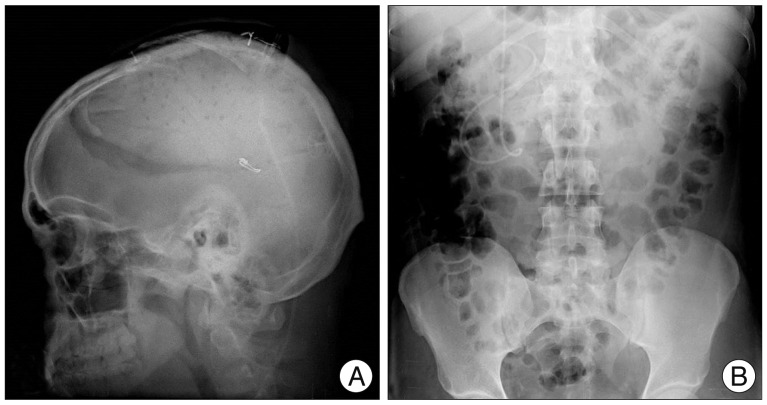
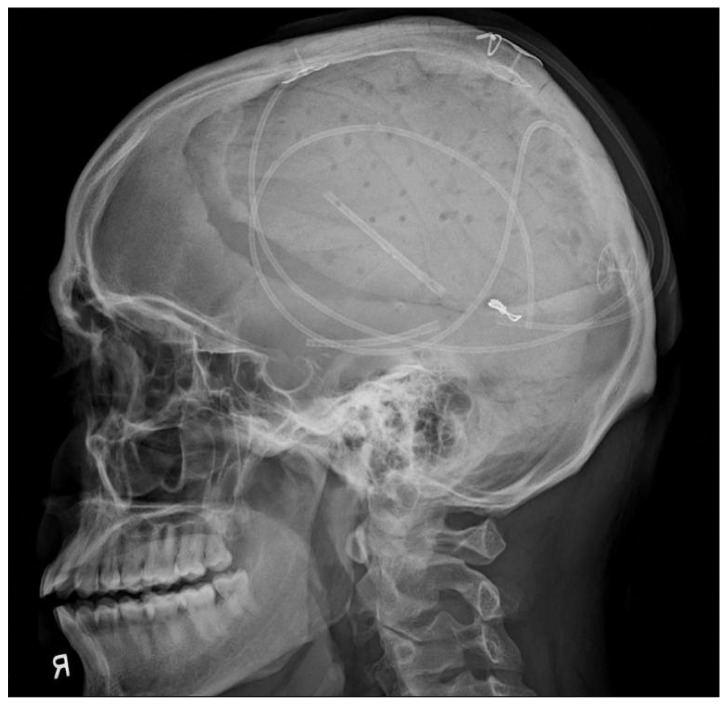
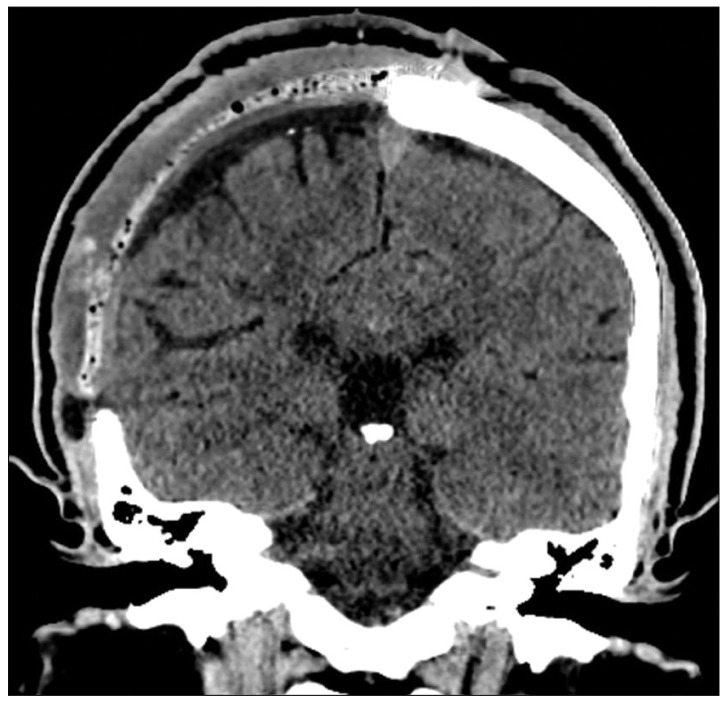
A 32-year-old male patient underwent a craniectomy and duraplasty with artificial dura due to an infected compound depressed skull fracture at another hospital. Eighteen months later, the patient underwent cranioplasty using methylmetacrylate for the skull defect which crossed the sagittal suture line. After the cranioplasty, the scalp progressively grew due to leakage of the cerebrospinal fluid (CSF) into the subgaleal space (Fig. 1). Conservative treatments such as direct aspiration of the CSF followed by compression with elastic bandage and continuous lumbar drainage were not effective. The patient underwent SP shunting for persistent cranial pseudomeningocele. Two short catheters were placed into the subgaleal space and connected to a distal catheter using a Y-shaped rigid connector without any valve systems (Fig. 2). The cranial shunt catheter was anchored at the level of the connector. Following the SP shunt, the pseudomeningocele were relieved. Six months later, the patient again presented with scalp swelling and headaches. Simple X-ray of the skull revealed a migrated and coiled shunt catheter under the scalp (Fig. 3). The peritoneal catheter was seen by an abdominal radiography. The patient was treated by removing the entire shunt catheter and the dura was covered with a subgaleal flap to prevent CSF leak. After the operation, the subgaleal CSF collection disappeared (Fig. 4) and the patient is currently doing well without further complications.
DISCUSSION
SP shunt is a simple and effective alternative treatment for cranial pseudomeningoceles5). The procedure of creating a SP shunt is similar to that of a VP shunt. In a SP shunt, the proximal catheter is inserted into the subgaleal space instead of the ventricle, and the remaining procedures of subcutaneous tunneling and distal catheter insertion is the same as in VP shunts. The most common complications of VP shunts are infection, obstruction, and mechanical failure due to fracture, disconnection, malposition, and kinking of catheter. However, unusual complications associated with VP shunts have been reported including CSF collection and cyst formation, bowel perforation, migration of the tube into pleural cavity, liver, heart, scrotum, anus, abdominal wall, vagina, uterus, and subcutaneous coiling of the peritoneal catheter2-4,6,8,10-12). Upward migration of the peritoneal catheter into the craniotomy flap or ventricle is extremely rare1,9). Various mechanisms for upward migration of peritoneal catheter have been described9). Repeated abdominal wall contractions can be the cause for driving the catheter out and into the fibrous tract around it. This event can be subsequent to high intra-abdominal pressure around the catheter leading to migration of the catheter toward the subcutaneous tissue. Vigorous movement of the head and neck can help upward migration of catheter. Also, wide subgaleal space associated with CSF collection can facilitate catheter movement in an upward direction9). Pang and Wilberger7) described that straight tubing without a valve could facilitate migration of the shunt catheter. In this case, wide subgaleal space, valveless shunt and, patient's habit (the patient rubbed the scalp frequently) might play a role in the process of shunt catheter migration.
CONCLUSION
SP shunt is a safe and simple alternative treatment for cranial pseudomeningocele. Although an extremely uncommon complication, proximal shunt catheter migration and coiling should be considered.