Comparison of Sagittal Spinopelvic Alignment between Lumbar Degenerative Spondylolisthesis and Degenerative Spinal Stenosis
Article information
Abstract
Objective
The purpose of this study was to evaluate the differences in sagittal spinopelvic alignment between lumbar degenerative spondylolisthesis (DSPL) and degenerative spinal stenosis (DSS).
Methods
Seventy patients with DSPL and 72 patients with DSS who were treated with lumbar interbody fusion surgery were included in this study. The following spinopelvic parameters were measured on whole spine lateral radiographs in a standing position : pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS), lumbar lordosis angle (LL), L4-S1 segmental lumbar angle (SLL), thoracic kyphosis (TK), and sagittal vertical axis from the C7 plumb line (SVA). Two groups were subdivided by SVA value, respectively. Normal SVA subgroup and positive SVA subgroup were divided as SVA value (<50 mm and ≥50 mm). Spinopelvic parameters/PI ratios were assessed and compared between the groups.
Results
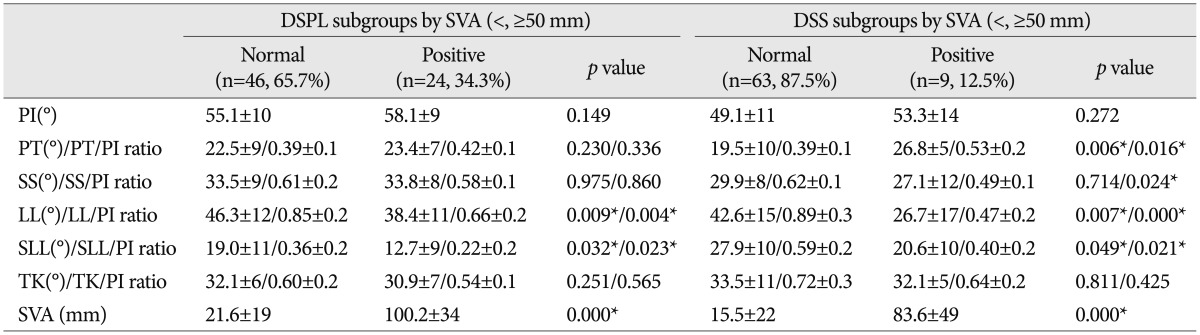
The PI of DSPL was significantly greater than that of DSS (p=0.000). The SVA of DSPL was significantly greater than that of DSS (p=0.001). In sub-group analysis between the positive (34.3%) and normal SVA (65.7%), there were significant differences in LL/PI and SLL/PI (p<0.05) in the DSPL group. In sub-group analysis between the positive (12.5%) and normal SVA (87.5%), there were significant differences in PT/PI, SS/PI, LL/PI and SLL/PI ratios (p<0.05) in the DSS group.
Conclusion
Patients with lumbar degenerative spondylolisthesis have the propensity for sagittal imbalance and higher pelvic incidence compared with those with degenerative spinal stenosis. Sagittal imbalance in patients with DSPL is significantly correlated with the loss of lumbar lordosis, especially loss of segmental lumbar lordosis.
INTRODUCTION
Lumbar degenerative spondylolisthesis (DSPL) and degenerative spinal stenosis (DSS) are representative degenerative spinal diseases. Both were originally described as separate pathological entities based on the anatomy involved, though both cause narrowing of the spinal canal, compression of the nerve roots, and can lead to neurogenic claudication17,22). However, there are some different regional radiographic findings between DSPL and DSS. DSPL shows anterior slipping of one segment of the spine compared to the next lower segment. DSS shows intervertebral disc degeneration, disc space narrowing, facet and ligamentum flavum hypertrophy without slippage. To date, numerous studies of the two disease entities regarding pathophysiology, clinical signs, and postoperative outcomes have been reported. Recently, whole spinal sagittal alignment is becoming increasingly important for assessing pathological mechanisms and treating degenerative spinal disease. Recent studies have suggested a prominent role of spinopelvic parameters to explain lumbosacral spondylolisthesis pathology6,14,17,19).
Sagittal alignment of the spine has been investigated in many studies, primarily in the normal population10,21). Also, several studies have reported sagittal alignment in populations of patients with low back pain9,10,11), degenerative spondylolisthesis2,21), and isthmic spondylolisthesis8,16). In addition, a few studies on spinopelvic alignment for DSPL and DSS have been reported2). However, there have been few studies that focused on the difference in sagittal alignments between the two disease entities. The purpose of this study was to evaluate differences in sagittal spinopelvic alignment between DSPL and DSS patients.
MATERIALS AND METHODS
Patient population
Seventy DSPL and 72 DSS patients who were treated with lumbar interbody fusion surgery at our institution from January 2009 to September 2011 were enrolled. The DSPL group consisted of 18 men and 52 women, and the DSS group consisted of 29 men and 43 women. The mean age was 62.3 years (range, 44-77 years) and 64.9 years (range, 42-87 years) in the DSPL and DSS groups, respectively.
The involved levels in the DSPL group were L3-4 in 9 patients (12.9%), L4-5 in 51 patients (72.9%), and L3-4-5 in 10 patients (14.3%).The slippage grade was evaluated according to Meyerding's classification15) and was determined to be 57.1% (40/70) grade I and 42.9% (30/70) grade II. Those levels involved in DSS were L3-4 in 6 patients (8.3%), L4-5 in 30 patients (41.7%), L5-S1 in 16 patients (22.2%), L3-4-5 in 12 patients (16.7%), and L4-5-S1 in 8 patients (11.1%) (Table 1).
All patients had symptoms unresponsive to conservative treatment for at least 6 months. Patients were excluded from the study if they had one or more of the following criteria, according to clinical and/or radiological data : history of any spinal surgery, including a lumbar discectomy, pathologic spinal disease (trauma or tumor), scoliosis, or femoral pathology.
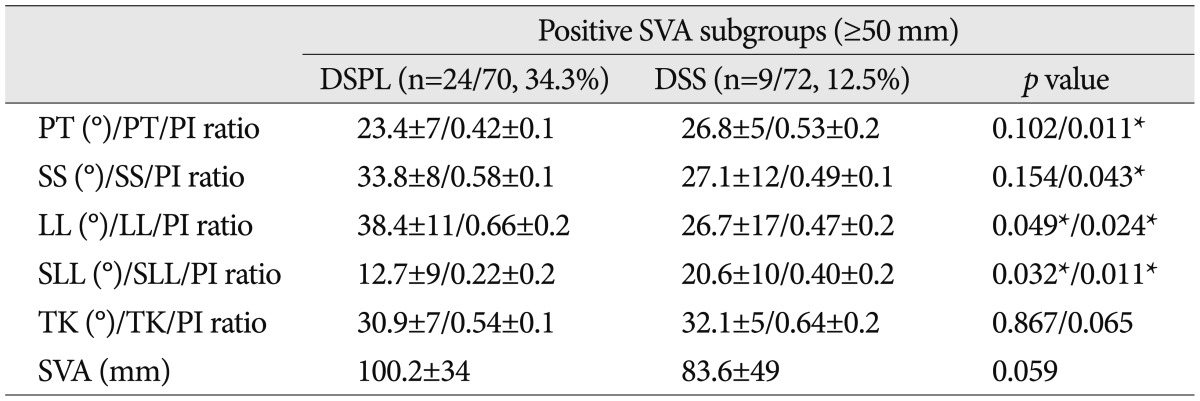
Spinopelvic parameters
Spinopelvic parameters were measured on a whole-spine lateral radiograph (14×36 inches) with the hips and knees extended in a standing position after at least 5 minutes of walking. The following radiographic parameters were measured : pelvic incidence (PI), sacral slope (SS), pelvic tilt (PT), lumbar lordosis (LL), L4-S1 segmental lumbar angle (SLL), thoracic kyphosis (TK), and sagittal vertical axis (SVA) from the C7 plumb line. PI is defined as the angle between the perpendicular to the upper sacral endplate at its midpoint and the line connecting this point to the femoral head axis. This is a morphologic parameter, considered as a constant, independent of the spatial orientation of the pelvis. The SS is defined as the angle between the horizontal and the upper sacral endplate. This is a positional parameter, varying according to the position of the pelvis. The PT is defined by the angle between the vertical and the line through the midpoint of the sacral plate to the femoral head axis; this is also a positional parameter. LL is defined as the angle between the upper L1 endplate and the upper sacral endplate. L4-S1 SLL is defined as the angle between the upper L4 endplate and the upper sacral endplate. L4-S1 segment is a hypermobile, commonly pathologic segment, and comprises most of the lumbar lordosis in the lumbar spine. TK is defined as the angle between the upper T4 endplate and the lower T12 endplate. SVA from the C7 plumb line is defined as the horizontal offset from the postero-superior corner of S1 to the C7 plumb line (Fig. 1).
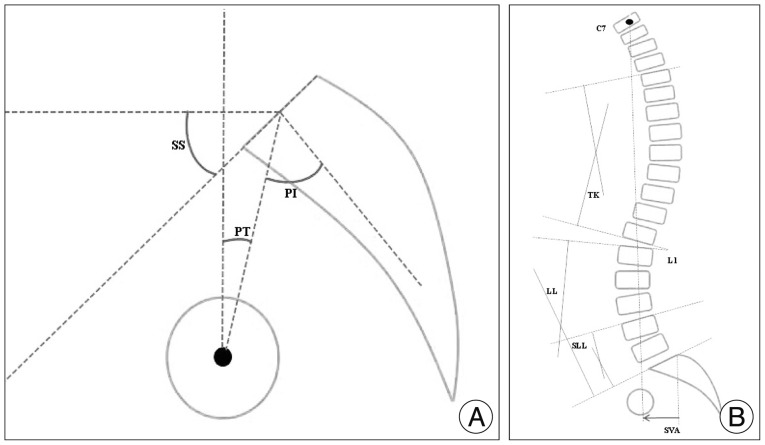
Illustration showing the spinopelvic parameters included in this study. A : This illustration displays the pelvic incidence (PI), the sacral slope (SS) and the pelvic tilt (PT). B : This illustration displays the thoracic kyphosis (TK), lumbar lordosis (LL), the segmental lumbar lordosis (SLL) and the sagittal vertical axis from the C7 plumb line (SVA).
All spinopelvic parameters measured by two individual physicians, respectively. The interobsever and intraobsever reliability of theses all radiographic parameters was assessed by inter- and intraclass correlation coefficient and those were above 0.8 for all parameters. Therefore, the method of digitally measuring these parameters was confirmed to be acceptable, and the measured data were highly reliable.
Statistical analysis
Statistical analysis was performed using SPSS software (version 18.0; SPSS Inc., Chicago, IL, USA). The Mann-Whitney U test was employed to analyze differences in non-categorical variables between the two groups. Overall differences of sagittal spinopelvic parameters between the DSPL and DSS groups were statistically analyzed. The groups were subdivided according to the SVA value (normal SVA <50 mm, positive SVA ≥50 mm). The differences of spinopelvic parameters between the subgroups were statistically analyzed. PI is a constant morphological parameter in an individual person. To minimize individual variations, spinopelvic parameters/PI ratios were assessed, and compared between the two groups. Statistical p-values less than 0.05 were considered statistically significant.
RESULTS
There were significant differences in PI, SS, SLL and SVA between the DSPL and DSS groups. The PI of DSPL (56.1±10°) was significantly greater than that of DSS (49.6±12°) (p=0.000). The SS (33.6±9°) and SVA (48.5±45 mm) of DSPL were also significantly greater than those (SS, 29.6±8°; SVA, 24.0±35 mm) of DSS (p=0.006; p=0.001). The SLL of DSPL (21.8±9°) was significantly lower than that of DSS (27.0±10°) (p=0.000). In analysis of parameter/PI ratios, the SLL/PI ratio of DSPL (0.40±0.2) was significantly lower than that of DSS (0.56±0.2) (p=0.000) (Table 2). In correlation analysis for assessing correlation between spinopelvic parameters and SVA, the LL (r=-0.396; p=0.001) and SLL (r=-0.317; p=0.007) of DSPL and LL (r=-0.367; p=0.002) had a weak negative correlation with SVA. The SLL (r=0.216; p=0.068) of DSS had no correlation with SVA.
The positive SVA (SVA ≥50 mm) and normal SVA subgroups (SVA <50 mm) of DSPL consisted of 24 patients (34.3%) and 46 patients (65.7%) out of 70 patients, respectively. The positive SVA and normal SVA subgroups of DSS consisted of 9 patients (12.5%) and 63 patients (87.5%) out of 72 patients, respectively.
In analysis of the positive and normal SVA subgroups of the DSPL group, there were significant differences in LL and SLL. The LL of the positive SVA subgroup (38.4±11°) was significantly lower than that of the normal SVA subgroup (46.3±12°) (p=0.009). The SLL of the positive SVA subgroup (12.7±9°) was significantly lower than that of the normal SVA subgroup (19.0±11°) (p=0.032). In analysis of parameters/PI ratios, there were also significant differences in LL/PI and SLL/PI ratios. The LL/PI ratio of the positive SVA subgroup (0.66±0.2) was significantly lower than that of the normal SVA subgroup (0.85±0.2) (p=0.004). The SLL/PI ratio of the positive SVA subgroup (0.22±0.2) was significantly lower than that of the normal SVA subgroup (0.36±0.2) (p=0.023).
In analysis of the positive and normal SVA subgroups of the DSS group, there were significant differences in PT (positive SVA subgroup, 26.8±5°; normal SVA subgroup, 19.5±10°), LL (26.7±17°; 42.6±15°) and SLL (20.6±10°; 27.9±10°) (p<0.05). In analysis of parameter/PI ratio, there were significant differences in PT/PI (positive SVA subgroup, 0.53±0.2; normal SVA subgroup, 0.39±0.1), SS/PI (0.49±0.1; 0.62±0.1), LL/PI (0.47±0.2; 0.89±0.3) and SLL/PI ratios (0.40±0.2; 0.59±0.2) (p<0.05) (Table 3).
In analysis between the positive SVA subgroups of DSPL and DSS, there were significant differences in PT/PI (DSPL, 0.40±0.1; DSS, 0.53±0.2), SS/PI (0.58±0.2; 0.49±0.1), LL/PI (0.66±0.2; 0.47±0.2) and SLL/PI ratio (0.22±0.2; 0.40±0.2) (p<0.05) (Table 4).
DISCUSSION
The sagittal balance of the spine is determined by the pelvic shape which is set by the PI. The PI was initially described by Duval-Beaupère et al.5) and has been recently studied by many investigators4,7). It is an invariable morphologic parameter in an individual person and an important anatomic parameter that reflects the anatomic configuration of the pelvis and greatly influences the sagittal configuration of the spine5,12,13). PI is strongly correlated with the SS and PT, and represents the algebraic sum of the SS and the PT : PI=SS+PT. Therefore, large-PI patients have also large PT and SS. Also, the morphology of the pelvis as quantified by PI is a strong determinant of the spatial position of the pelvis in a standing position : as the PI increases, so do SS, PT, or both. Values of spinopelvic parameters and correlations between them in the normal population have been well-established. Oh et al.16) reported the spinopelvic parameters of Korean normal population as followings, the PI was 49°; the SS was 38°; the PT was 11°, the LL was 48°16). Legaye et al.13) and Vaz et al.20) have demonstrated a correlation between PI and LL in the general population; a low PI is usually associated with a low lumbar lordosis, whereas a high PI is usually associated with a high lumbar lordosis. Also, the correlation between LL and SS has been reported in normal populations; LL increases linearly with SS. In the present study, for the precise analysis of variable parameters by individual constant PI variations, spinopelvic parameters/PI ratios were assessed, and compared between the two groups.
Degenerative spondylolisthesis vs. degenerative spinal stenosis
DSPL has traditionally been considered as a subcategory within the broader diagnosis of DSS because both patients may present with similar clinical symptoms and signs1). However, current studies suggest that they have different demographic characteristics and radiographic findings. Epidemiologically, Rosenberg18) reported that women were more likely to present with DSPL than men. In the present study, the proportion of women in the DSPL population was higher than that in the DSS population. In the current study, the DSPL population tended to have single-level, severe stenosis at L4-5, while the DSS population more frequently had moderate, multi-level involvement. The most common lesion of DSPL was at L4-5 (72.9%), while DSS tended to have multi-level involvement (Table 1).
Oh et al.16) reported that PI of normal Korean population is 49°. In present study, mean PI of DSS group was 49° and that of DSPL was 56°. Seven degrees difference between both groups seems not significantly large, but there was different statistically between groups. Also, there was a significant difference in SS between the two groups (DSPL : 33°; DSS : 29°). PT was larger in both groups (DSPL 22° and DSS 20°), but it was not significantly different between the two groups (Table 2). Legaye et al.13) reported that a large PI indicated a large SS and large sagittal curves. Barrey et al.2,3) reported that patients with DSPL demonstrated significantly greater PI (60°) than the normal population (52°). Schuller et al.19) also reported a significant increase in PI (66° vs. 54°) and SS (42° vs. 33°) in the DSPL group than in the degenerative disc disease group. They suggested the anatomic orientation of the pelvis with a high PI and SS seems to represent a predisposing factor for DSPL. These current reports were concordant with the results of our study. Funao et al.6) reported that global sagittal balance was well-maintained in the DSPL and non-DSPL groups, and there was no significant difference in PT (23° vs. 22°) between the DSPL and non-DSPL patients. Schuller et al.19) reported a significant increase in PT (25° vs. 21°) in the DSPL group compared to that of the reference group. In the present study, global sagittal balance was also maintained in both groups, as the mean SVA of DSPL and DSS groups was also within normal range when SVA <50 mm, but that of DSPL (48 mm) was significantly greater than that of DSS (24 mm), statistically. The proportion of those with positive SVA in the DSPL group (34%) was higher compared with that of the DSS group (12%). In analysis of parameters, the variation of SVA was large in both groups. It seems that there were many patients with parameter similar with the counter group. I presented plotted graph of parameters including SVA. According to plotted graph, all values were within 2-standard deviation in both groups (Fig. 2) and there were statistically differences in SVA between two groups. There was no significant difference in PT (22° vs. 20°). In addition, there were significant differences in L4-S1 SLL between the two groups. The SLL of DSPL (21°) was significant less than that of DSS (27°) (Table 2). The L4-S1 segment is a hypermobile segment, the most common segmental instability, especially DSPL and/or stenosis lesion in DSPL and DSS pathology, and comprises most of the lumbar lordosis in the lumbar spine. And, in correlation analysis for assessing correlation between spinopelvic parameters and SVA, the LL (r=-0.396; p=0.001) and SLL (r=-0.317; p=0.007) of DSPL and LL (r=-0.367; p=0.002) of DSS had a weak negative correlation with SVA. The SLL (r=0.216; p=0.068) of DSS had no correlation with SVA.

Plot graph of spinopelvic parameters in DSPL and DSS patients. All values were within 2-standard deviation. PI : pelvic incidence, PT : pelvic tilt, SS : sacral slope, LL : lumbar lordosis, SLL : segmental lumbar lordosis, TK : thoracic kyphosis, SVA : sagittal vertical axis from C7 plumb line, DSPL : degenerative spondylolisthesis, DSS : degenerative spinal stenosis.
In the present study, unlike other studies, spinopelvic parameters/PI ratios were assessed (Table 2) because while PI is a fixed constant parameter in an individual person, other variable parameters are defined by PI and thus become larger or smaller based on the PI, and plotted graph of parameters/PI ratios were also presented (Fig. 3). In analysis of spinopelvic parameters/PI ratios between the two groups, there was a significant difference in the SLL/PI ratio (DSPL, 0.40; DSS, 0.56). In a simple comparison of parameters between the two groups, the LL of the DSPL group was larger than that of the DSS group, but the LL/PI ratio of the DSPL group was smaller than that of the DSS group in comparison of parameter/PI ratios (Table 2). It means that the LL of DSPL is also larger than that of DSS because the PI of the DSPL group is larger than that of the DSS group, but the LL of the DSPL group considering the PI value is actually smaller than that of the DSS group. Also, it seems that loss of LL in DSPL contributed to the significant loss of SLL compared with DSS. The loss of SLL in DSPL is larger and caused by anterior slippage as well as degenerative disc space narrowing, whereas the loss of SLL in DSS is caused by degenerative disc space narrowing. According to present study, the loss of lumbar lordosis contributed to significantly loss of segmental lumbar lordosis and larger SVA may be a driving force for DSPL.
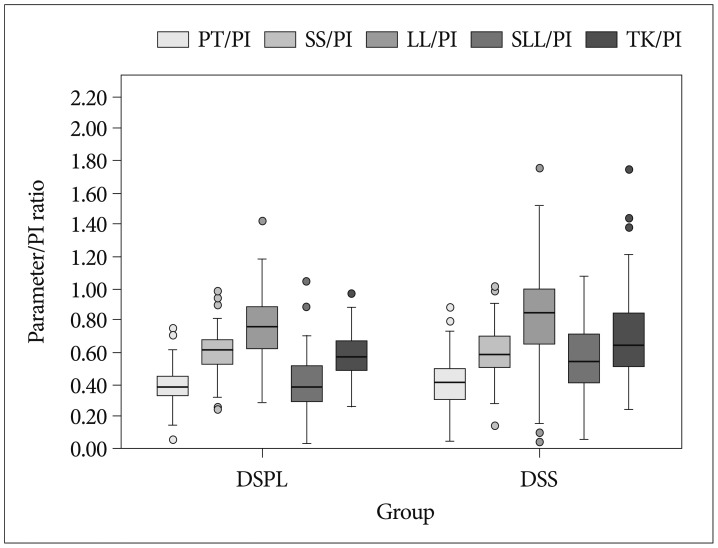
Plot graph of spinopelvic parameters/PI ratios in DSPL and DSS patients. All values were within 2-standard deviation. PI : pelvic incidence, PT : pelvic tilt, SS : sacral slope, LL : lumbar lordosis, SLL : segmental lumbar lordosis, TK : thoracic kyphosis, SVA : sagittal vertical axis from C7 plumb line, DSPL : degenerative spondylolisthesis, DSS : degenerative spinal stenosis.
In analysis between positive and normal SVA subgroups in DSPL group, the LL and SLL of the positive SVA subgroup were significantly lower than that of the normal SVA subgroup in the DSPL group. And, the LL/PI and SLL/PI ratio of positive SVA group were also significantly lower. It seems that the significant loss of lumbar lordosis and segmental lumbar lordosis induce sagittal imbalance of DSPL. But, in analysis between positive and normal SVA subgroups in DSS group, there were significant differences in PT, LL and SLL, and all parameters/PI ratios between DSS subgroups. It means that sagittal imbalance of DSS is diffusely correlated with PT, SS, LL, and SLL (Table 3). In analysis of parameters/PI ratios between the positive SVA subgroups of each group, all values of parameters/PI ratios were significantly different; the PT/PI ratio was larger in DSS than in DSPL, the SS/PI ratio was smaller in DSS than in DSPL, the LL/PI ratio was larger in DSPL than in DSS, and the SLL/PI ratio was smaller in DSPL than in DSS (Table 4). It seems that the sagittal imbalance of DSPL is caused by the loss of LL (LL/PI ratio, 0.66) and significant loss of SLL (SLL/PI ratio, 0.22), and mild pelvic retroversion (PT/PI ratio, 0.40) acted as a compensatory mechanism. However, sagittal imbalance of the DSS population is caused by overall loss of LL, and significant pelvic retroversion (PT/PI ratio, 0.53) operated as a compensation mechanism. The mean SVA of the positive SVA DSPL subgroup (100 mm) was larger than that of the positive DSS subgroup (83 mm) despite the relatively large LL and LL/PI ratios in the DSPL subgroup. It may be caused by a significant loss of lower lumbar (SLL) and anterior slippage in DSPL, and less generation of compensatory mechanisms (Fig. 4).

Illustration showing the difference of sagittal spinopelvic alignment between DSPL (A) and DSS (B). A : This illustration displays the sagittal spinopelvic alignment of DSPL. B : This illustration displays the sagittal spinopelvic alignment of DSS. DSPL : degenerative spondylolisthesis, DSS : degenerative spinal stenosis, LL : lumbar lordosis, SLL : segmental lumbar lordosis, PT : pelvic tilt, PI : pelvic incidence, SVA : sagittal vertical axis from C7 plumb line.
Limitations of the present study include the lack of an age- and sex-matched analysis, a small sample size, and the retrospective nature of the study. Nonetheless, the results of this study are meaningful because the differences in sagittal spinopelvic alignments between DSPL and DSS were investigated. These results will be helpful and must be considered in the surgical treatment of DSPL and DSS. However, we recognize that a prospective, larger and longitudinal study is necessary to clearly establish the spinopelvic alignments of DSPL and DSS.
CONCLUSION
Patients with lumbar degenerative spondylolisthesis have a greater PI, lower SLL/PI ratio and relatively high propensity for sagittal imbalance compared with degenerative spinal stenosis patients. Patients with DSS have a normal PI and relatively well-compensated sagittal balance from pelvic retroversion.
Patients with DSPL with positive SVA had significant loss of LL and SLL, however patients with DSS with positive SVA often have significant differences in PT, SS, LL, and SLL.
Acknowledgements
This study was presented in an oral session at the annual spring meeting of the Korean Neurosurgical Society, 2012.