Comparison of the Indications and Treatment Results of Burr-Hole Drainage at the Maximal Thickness Area versus Twist-Drill Craniostomy at the Pre-Coronal Point for the Evacuation of Symptomatic Chronic Subdural Hematomas
Article information
Abstract
Objective
To analyze the clinical data and surgical results from symptomatic chronic subdural hematoma (CSDH) patients who underwent burr-hole drainage (BHD) at the maximal thickness area and twist-drill craniostomy (TDC) at the precoronal point.
Methods
We analyzed data from 65 symptomatic CSDH patients who underwent TDC at the pre-coronal point or BHD at the maximal thickness area. For TDC, we defined the pre-coronal point to be 1 cm anterior to the coronal suture at the level of the superior temporal line. TDC was performed in patients with CSDH that extended beyond the coronal suture, as confirmed by preoperative CT scans. Medical records, radiological findings, and clinical performance were reviewed and analyzed.
Results
Of the 65 CSDH patients, 13/17 (76.4%) with BHD and 42/48 (87.5%) with TDC showed improved clinical performance and radiological findings after surgery. Catheter failure was seen in 1/48 (2.4%) cases of TDC. Five patients (29.4%) in the BHD group and four patients (8.33%) in the TDC group underwent reoperations due to remaining hematomas, and they improved with a second operation, BHD or TDC.
Conclusion
Both BHD at the maximal thickness area and TDC at the pre-coronal point are safe and effective drainage methods for symptomatic CSDHs with reasonable indications.
INTRODUCTION
Chronic subdural hematoma (CSDH) is a disease of old age, and surgery in these patients carries a higher risk. Recent advances in imaging techniques, in addition to the widespread use of antiplatelet and anticoagulant drugs, have also resulted in an increase in CSDH diagnoses7).
Treatment of CSDH has been controversial. Although non-operative management of CSDH is certainly an option12), the prevailing opinion is that patients with symptomatic CSDH should be treated with surgical evacuation. Surgical procedures for CSDH have been favored by the less invasive twist-drill craniostomy (TDC) and burr-hole drainage (BHD) techniques.
Many studies have reported that TDC in many ways was better for the management of CSDH3). However, it is also well known that TDC carries a risk of hemorrhagic complications, as it is a blind technique. The pre-coronal point is based on anatomy, external carotid artery angiography, and brain imaging. TDC at the pre-coronal point with closed-system drainage for symptomatic CSDH was shown to be a normally safe entry point in a previous report from our institute4,8). The aim of this study was to compare more clinical data and surgical results for patients who underwent BHD at the maximal thickness area and TDC at the pre-coronal point with closed-system drainage as a continuation of our previous report.
MATERIALS AND METHODS
Definitions and indications for BHD at the maximal thickness area and TDC at the pre-coronal point
This retrospective study was performed on consecutive symptomatic patients with CSDH who were treated surgically at a single institution between January 2009 and December 2010. The 65 patients underwent surgical evacuation for CSDH, defined as a collection of fluid within the potential subdural space, radiographically consistent with liquefying blood and appearing hypo-dense on brain computed tomography (CT) scans. Complete medical records of 65 patients were available for evaluation of the clinical course, postoperative CT scans, and complications. The 65 patients were divided into two groups : BHD at the maximal thickness area (17 patients : 8 men, 9 women) and TDC at the pre-coronal point (48 patients : 28 men, 20 women).
We defined the pre-coronal point, as confirmed by preoperative CT scans, to be 1 cm anterior to the coronal suture at the level of the superior temporal line4). On brain CT scans, the level of the superior temporal line was defined as the top of the densest part of the temporalis muscle around the coronal suture. The coronal suture and the superior temporal line could be identified clearly on brain CT scans. We defined the maximal thickness area as the point of maximum thickness of the hematoma. All patients were evaluated using preoperative CT scans (Fig. 1). The clinical grade was determined during the preoperation period and 3 months after surgery according to the Markwalder grading scale (MGS)9).
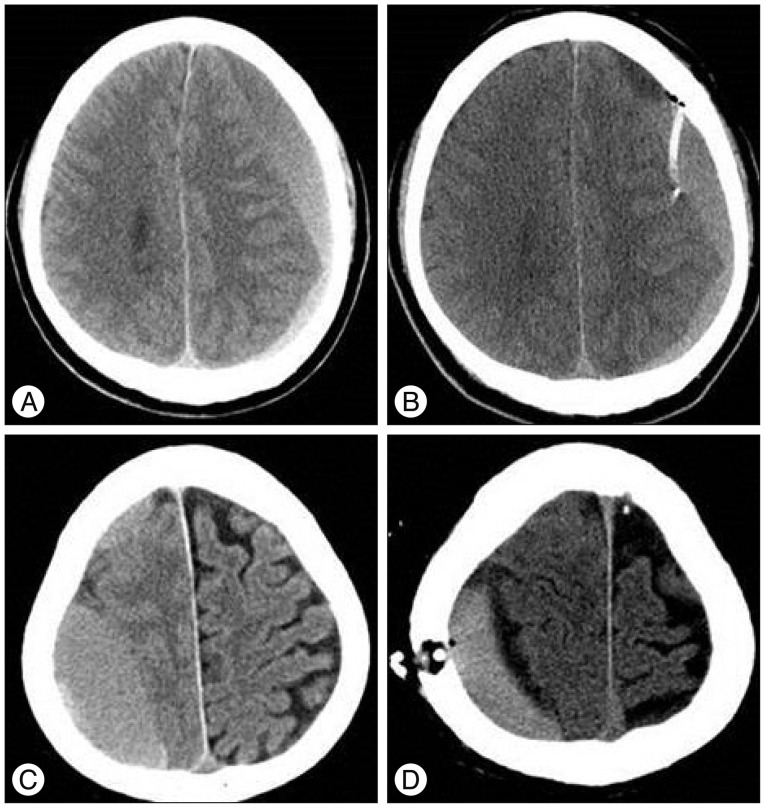
A and B : These images show a comparison of a preoperative brain CT scan and a postoperative brain CT scan after twist-drill craniostomy in a 58-year-old male patient. B : The image shows that the ventriculostomy ca-theter was introduced into the subdural space at the pre-coronal point, defined as 1 cm anterior to the coronal suture at the superior temporal line. C and D : These images show a comparison of a preoperative brain CT scan and a postoperative brain CT scan after burr-hole drainage in a 71-year-old male patient. D : The image shows the burr-hole at the maximal thickness area.
Operative procedures
Burr-hole drainage at the maximal thickness area
After the diagnosis of CSDH by clinical examination and radiological evaluation, all patients in this group underwent evacuation of the subdural hematoma using BHD at the maximal thickness area with local anesthesia and intravenous sedation in the operating room. A local hair shave and infiltration of local anesthesia were performed, and a 15-mm burr-hole was made using a Midas-Rex drill after a 3- to 4-cm skin incision was made over the area of maximal hematoma thickness. The dura and outer membrane were incised in a cruciate fashion, and the CSDH was drained.
Twist-drill craniostomy at the pre-coronal point
The pre-coronal point was identified in each patient in the operating room before draping; it was measured in the usual manner with reference to the external landmarks of the coronal suture and the superior temporal line. After scalp preparation with alcohol and povidone-iodine solution, 2% lidocaine was infiltrated. A stab incision was made using a no. 15 scalpel at the drill entry point. First, a hand drill, equipped with a 4-cm Steinman pin was placed perpendicular to the surface of the skull, and a mark was made on the outer skull to keep the twist drill from slipping. Then, using a 6-cm twist drill, the skull and dura were penetrated at a 45° angle to the surface of the bone to prevent the catheter entering the cortex. The typical direction of the drill was posterior-inferior, towards the auricle. A standard no. 5 ventriculostomy catheter was introduced into the subdural cavity -5 cm. The contents of the catheter flowed freely due to the downward orientation of the catheter. Neither aspiration with negative pressure nor flushing with normal saline was performed. The closed-system drainage was assembled by attaching the catheter to a ventricular drainage bag, and the catheter was left in the hematoma cavity for a few days to drain it slowly.
Estimation method
The clinical grade was determined in the pre-operation period and 3 months after surgery according to the MGS9) (Table 1). We performed CT scans in the preoperative period. Postoperative CT scans were conducted routinely at 3 hours, 3 days, and 3 months after surgery. Postoperative air accumulation was defined as dense air around the subdural catheter. The CSDH density of preoperative CT scans was classified as hypo-dense, iso-dense, high-density, or mixed-density. The CSDH was classified as mixed-density if it contained some acute blood, iso-dense if it reached the brain parenchyma, or hyper-dense or hypo-dense if it reached the brain. Catheter failure was defined as an inappropriate position. Recurrence of CSDH was defined as confirmed postoperative hematoma expansion on postoperative CT scans and aggravation of neurological dysfunction. We used Student's t-test to compare means and the χ2-test to analyze the frequency.
RESULTS
Patient demographic data
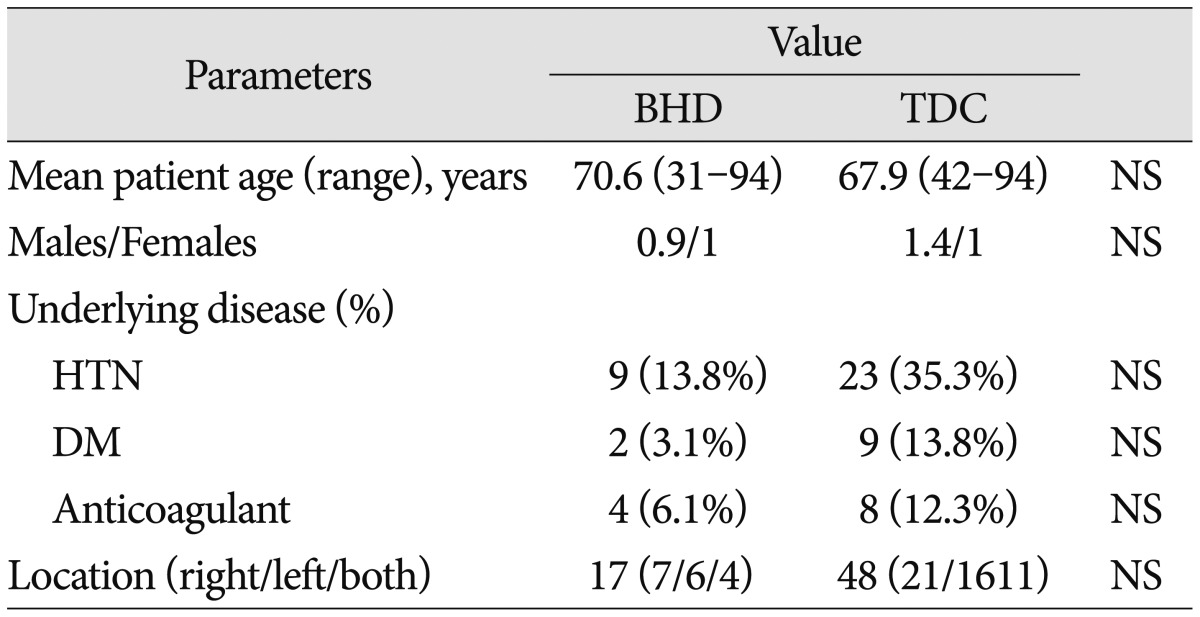
Demographic and clinical data for the 65 patients with symptomatic CSDH are shown in Table 2. Overall, the mean patient age was 68.6 (range, 31-94) years, and the male : female ratio was 1.2 : 1. For BHD at the maximal thickness area, the mean age was 70.6 (range, 31-94) years, and the male : female ratio was 0.9 : 1. For TDC at the pre-coronal point, the mean age was 67.9 (range, 42-94) years; the male : female ratio was 1.4 : 1. Underlying diseases and their locations are shown in Table 2. The data showed no significant difference between the groups.
Preoperative radiological imaging
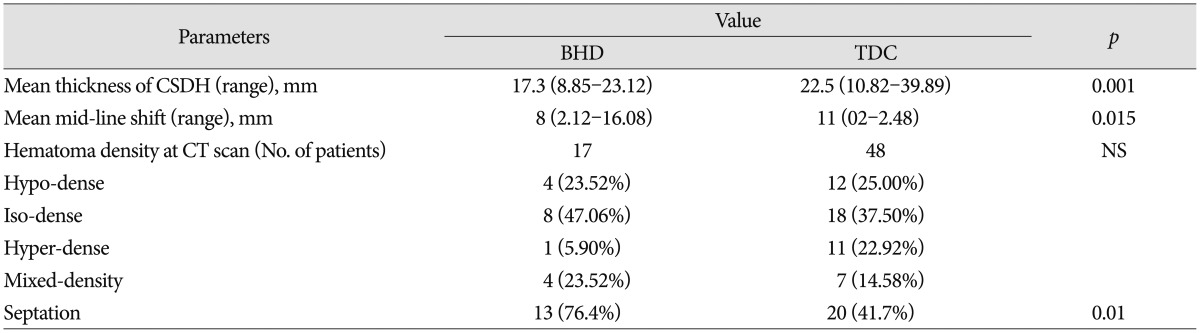
The mean thickness of the CSDH for BHD at the maximal thickness area was 17.3 (range, 8.85-23.12) mm, and the mean thickness for TDC at the pre-coronal point was 22.5 (range, 10.82-39.89) mm (p=0.001). The mean midline shift in CSDH for BHD at the maximal thickness area was 8 (range, 2.12-16.08) mm, and the mean midline shift for TDC at the pre-coronal point was 11 (range, 0-22.48) mm (p=0.015). The hematoma density and septation in the CT scan (hypo-dense, iso-dense, hyper-dense, or mixed-density) are shown in Table 3.
Postoperative parameters
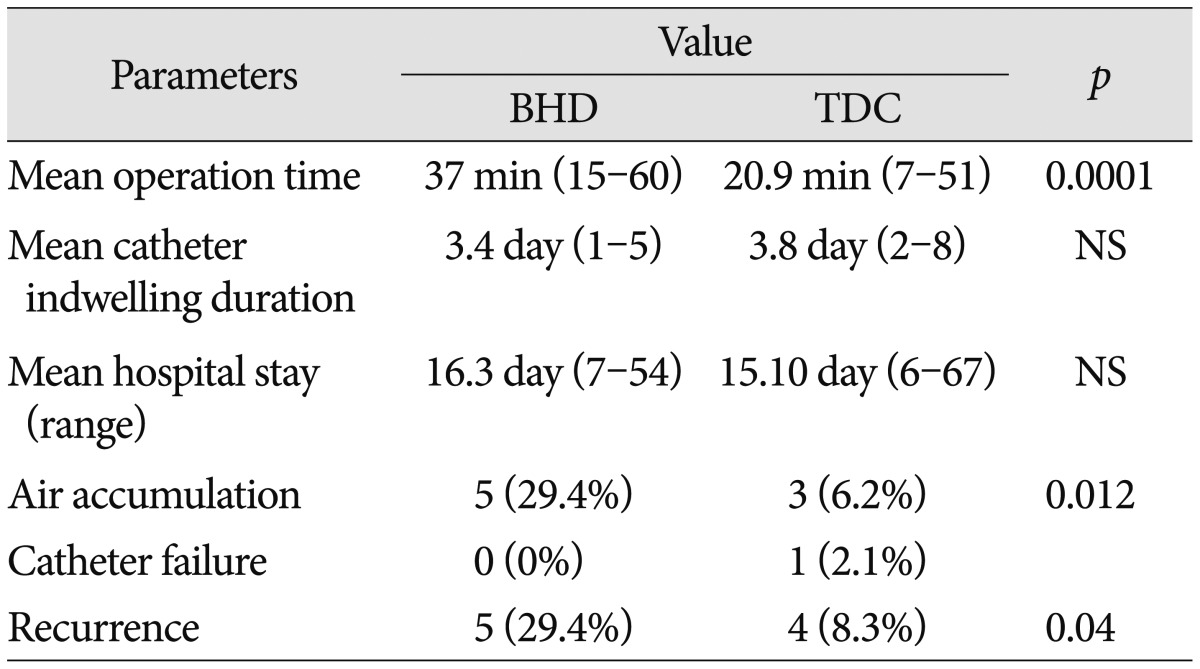
The operation times were significantly shorter in the TDC at the pre-coronal point group (range, 7-51 min; mean 20.9 min) than in the BHD at the maximal thickness area group (range, 15-60 min; mean 37 min) for both unilateral and bilateral cases (p=0.0001). The mean duration of the indwelling subdural catheter for BHD at the maximal thickness area was 3.4 (range, 1-5) days and for TDC at the pre-coronal point 3.8 (range, 2-8) days (p=0.205). The mean hospital stays in the two groups were similar : 16.3 (range, 7-54) days for BHD at the maximal thickness area and 15.10 (range, 6-67) days for TDC at the pre-coronal point.
We found air accumulation for BHD at the maximal thickness area in 5 (29.4%) cases and for TDC at the pre-coronal point in 3 (6.2%) cases on postoperative brain CT scans (p=0.012). Catheter failure for BHD at the maximal thickness area was 0 (0%) and occurred in one TDC at the pre-coronal point case (1/48, 2.1%). Recurrence was 5/17 (29.4%) for BHD at the maximal thickness area and 4/48 (8.3%) for TDC at the pre-coronal point (p=0.04)(Table 4).
Our data indicate that the initial maximal thickness and midline shifting were more severe with TDC. However, the TDC group showed a shorter operation time and fewer surgical complications than the BHD group at the maximal thickness area.
Clinical outcome
Analysis of our data revealed that patient clinical performance was downgraded from preoperative to postoperative grades for BHD at the maximal thickness area : 12 (70.5%) patients of grade 1 and 2 (11.7%) of grade 2 were downgraded to 13 (76.4%) of grade 0 and 1 (5.8%) of grade 1. Among the TDC group, 37 (77.0%) were grade 1, and 8 (16.6%) were grade 2 preoperatively. After TDC, the grades decreased to grade 1 in 42 (87.5%), grade 0 in 3 (6.2%), and increased to grade 3 in 3 (6.2%) patients. Of the 65 patients, 59 showed symptomatic and neurological improvements; six did not : 3 (17.6%) of grade 3 in the BHD at the maximal thickness area group and 3 (6.2%) of grade 3 in the TDC at the pre-coronal point group (Table 5).
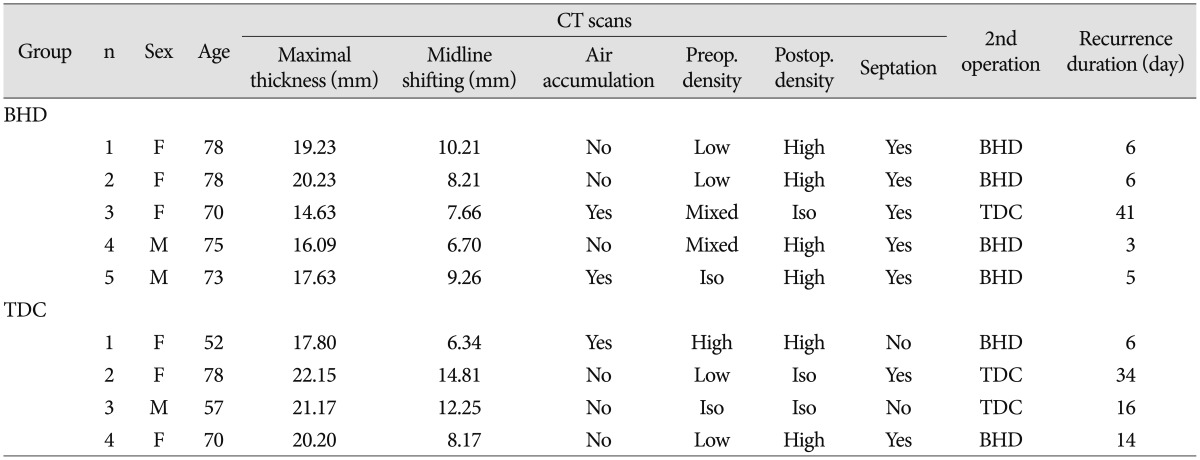
Recurrence cases
Clinical and radiological data showed five patients with recurrence in the BHD at the maximal thickness area group. The mean age of the patients was 74.8 years (range, 70-78), the mean maximal thickness was 17.56 mm (range, 14.63-20.23), and the mean midline shift was 8.40 mm (range, 6.7-10.21) (Table 6).
Clinical and radiological data showed four patients with recurrence in the TDC at the pre-coronal point group. The mean age was 64.2 years (range, 52-78). The mean maximal thickness was 4 mm (range, 17.8-22.15), and the mean midline shift was 10.39 mm (range, 6.34-14.81) (Table 6).
Both BHD at the maximal thickness area and TDC at the pre-coronal point were safe and effective drainage methods for symptomatic CSDHs. However, the rate of recurrence with TDC at the pre-coronal point was lower than that of BHD at the maximal thick-ness area.
DISCUSSION
In a recent article, from 16 randomized trials, the calculated overall estimates following management of CSDH patients per 100 individuals per year were 4% (95% CI, 2-7) mortality, 11% (95% CI, 5-19) morbidity, 82% (95% CI, 75-89) 'cure', and 11% (95% CI, 9-14) recurrence1). Conventional medical treatment, especially the use of mannitol alone, is not effective for CSDH management2). However, some recent studies have reported a few effective medical treatments.
Weigel et al.14) reported that ACE inhibitor treatment for the control of arterial hypertension lowered the risk of recurrence in patients undergoing operations for CSDH and possibly even the development of CSDH. This effect might be the result of an antiangiogenic effect of ACE inhibitors.
Several studies have shown that hyperfibrinolytic activities play a major role in the liquefaction and enlargement of CSDHs. Kageyama et al.5) hypothesized that CSDH can be treated with tranexamic acid without concomitant surgery. Tranexamic acid may simultaneously inhibit the fibrinolytic and inflammatory (kinin-kallikrein) systems, which might, consequently, resolve the CSDH. This treatment may prevent the early stages of CSDH that can occur after head trauma and recurrence of CSDH after surgery. However, surgical treatment is still considered to be more important in most cases.
The results of the current analysis show statistical evidence of similar efficacy and safety with short operation time obtained from the bedside drainage of CSDH compared with the most commonly practiced procedure (i.e., operating room burr-hole evacuation). The associated potential cost savings related to operating theater resources and the involvement of multiple health professionals differentiate TDC and BHD. Given that CSDHs are more frequent among the elderly, these treatments also diverge in terms of the perioperative risks related to general anesthesia, because BHDs are frequently performed under general sedation, whereas a local anesthetic is usually sufficient for TDC. Moreover, the amount of tissue cut and the size of skull hole favor TDC as the less invasive procedure1). TDC at the pre-coronal point is simple and easy surgical procedures compared with BHD at the maximal thickness area. For these reasons, TDC is a safe and effective procedure for CSDH in the elderly and may be considered as the first, and only, option in these patients10).
The use of TDC in the treatment of a chronic subdural hematoma was popularized by Tabaddor and Shulman13). However, because it is a blind technique, TDC does carry a risk of hemorrhagic complications. Postoperative intracranial hematomas include epidural, subdural, and intracerebral hematomas, due to brain penetration. Injury of the middle meningeal artery (MMA) during TDC may cause the development of epidural hematomas and also of subdural hematomas.
To some extent, considering our method, we have overcome the limitations of the blind technique. That is, the normal entry point for TDC was defined as 1 cm anterior to the coronal suture at the level of the superior temporal line for a safe procedure because all branches of the MMA run posterior to the coronal suture, and the vascular grooves are also located posterior to the coronal suture at the level of the superior temporal line4).
The recurrence was not found associated with the residual air volume in the hematoma cavity according to the previous studies6,11). However, the recurrence was associated with residual air accumulation between TDC and BHD in our study. So, further study is required for relationship between air accumulation and recurrence rate.
This study has some limitations. First, it was a retrospective analysis, not a randomized, controlled study. Second, there is no clear standard for drainage rate. Currently, we consider draining at 50 cc/h, but if there is a worsening headache or drainage of fresh red-colored hematoma, draining is stopped or the rate is reduced. Third, because all patients were Koreans and the sample size was small, the conclusions that can be drawn from these findings may be limited.
CONCLUSION
We analyzed the evacuation of symptomatic CSDHs in 65 patients, performed at a single institution, retrospectively. An analysis of our data revealed that BHD at the maximal thickness area and TDC at the pre-coronal point were safe and effective methods for CSDH treatment with reasonable indications.