Delayed Improvement after Endoscopic Carpal Tunnel Release
Article information
Abstract
Objective
In most patients with carpal tunnel syndrome (CTS), pain and/or paresthesia disappeared or decreased in a month after endoscopic carpal tunnel release (ECTR). However, subpopulation of patients showed delayed improvement following ECTR. We analyzed the delayed improvement hands to investigate the characteristics of those patients and to determine the predictable factors of delayed improvement.
Methods
Single-portal ECTRs were performed in 1194 hands of 793 CTS patients from 2002 to 2011. Five-hundred seventy hands with minimal 1-year postoperative follow-up were included. We divided the 545 satisfied hands into early (group A) and delayed (group B) groups according to improvement period of 1 month. Demographic data, clinical severity and electrodiagnostic abnormality were compared between groups.
Results
Group A included 510 hands and group B included 35 hands. In group B, 11 hands improved in 2 months, 15 hands in 3 months and 9 hands in 6 months, respectively. In group A/B, according to clinical severity, 60/1 hands were graded to I, 345/24 hands to II, 105/10 hands to III. In group A/B, based on electrodiagnostic abnormality, 57/3 hands were classified to mild, 221/11 hands to moderate and 222/21 hands to severe group. Statistical analysis between groups did not reach significance but electrodiagnostic or clinical severity had a tendency to affect the delayed response.
Conclusion
It is difficult to predict the factors contributing to postoperatively-delayed response in subpopulation of CTS patients. However, we recommend that postoperative observation for at least 6 months is necessary in patients without symptomatic improvement.
INTRODUCTION
Carpal tunnel syndrome (CTS) represents the most common compressive peripheral neuropathy, predominantly presenting as a tingling sensation, pain and numbness in the distribution of the median nerve and it is estimated to affect about 1% of the population33,37). CTS is usually diagnosed on the basis of the patient's history and clinical findings, and confirmed by electrophysiological studies. Recently, ultrasonography and/or magnetic resonance imaging can also be used to evaluate the median nerve and surrounding structures to complement electrophysiological study in diagnosing CTS12,35).
When conservative treatment including medications, splinting or local injection of steroid into carpal tunnel fails, simple decompression of the median nerve by division of the transverse carpal ligament is indicated as an effective surgical treatment. As surgical technique, open carpal tunnel release (OCTR) has been the gold standard method. Since the introduction of endoscopic technique by Okutsu et al.32) in 1987 for treatment of CTS, endoscopic carpal tunnel release (ECTR) has been widely used as a minimally-invasive carpal tunnel surgery22). ECTR techniques are divided into two categories depending on the number of skin incision used to access carpal tunnel : single-portal vs. dual-portal techniques. ECTR has advantage over OCTR such as less postoperative pain and more rapid postoperative recovery but there is still major controversy between the two procedures regarding the outcome and the complication rates5,22,31,41).
Successful results after endoscopic carpal tunnel decompression have been reported with range from 92 to 98%10,22,40). In most CTS patients with successful postoperative outcome, preoperative tingling sensation and pain decreased significantly within 1-7 days after ECTR and completely resolved by one-postoperative month31,41). However, a small number of patients showed delayed improvement after 1 month following ECTR. Although various studies have reported preoperative prognostic indicators of the outcome of carpal tunnel release8,23,30,43,44), to the knowledge of the authors, there have been no studies that have analyzed the delayed improvement patients after endoscopic carpal tunnel surgery. We analyzed patient subpopulation with the delayed improvement after ECTR to investigate the characteristics of those patients and to determine the predictable factors of delayed improvement.
MATERIALS AND METHODS
Patient population
We retrospectively reviewed databases of CTS patients who underwent ECTR at our hospital from 2002 to 2011. The preoperative assessment included a detailed history, symptoms and physical examination and all patients undergoing ECTR had electrodiagnostic studies confirming compression of the median nerve at the level of the transverse carpal ligament. However, small number of patients with severe symptoms underwent ECTR even though electrodiagnostic studies did not reveal any abnormalities, compatable with CTS. Patients with postoperative period more than 12 months were analyzed and patients with prior carpal tunnel surgery or patients with diabetes or an underlying disease, related to CTS were excluded from the study.
Clinical grade
The clinical findings in the patient group were classified into 3 grades according to the consistency and severity of symptoms as follows17).
Grade I : intermittent symptoms with paresthesia at night
Grade II : persistent symptoms throughout the day with hypesthesia in the finger of the median nerve distribution
Grade III : constant symptoms with weakness or thenar muscle atrophy
Electrodiagnostic grade
The electrophysiological study was performed using a Cadwell Sierra Wave® (Cadwell Laboratories, Kennewick, WA, USA). The study consisted of motor and sensory median nerve conduction tests using standard techniques according to the practice parameters for the electrodiagnosis of CTS of the American Association of Electrodiagnostic Medicine, the American Academy of Neurology, and the American Academy of Physical Medicine and Rehabilitation3). The electrophysiological abnormalities were classified into three grades according to Stevens' classification as follows39).
Mild : prolonged median sensory distal latency
Moderate : prolonged median sensory and motor distal latency
Severe : abnormal needle electromyography other than the above two abnormalities, or no response in sensory and motor distal latency
Surgical technique
The modified Menon's single-portal method25) was applied to all of the 793 patients as a means of ECTR by the same neurosurgeon. ECTR was carried out under monitored anesthetic care by intravenous injection of propofol without endotracheal intubation. After exsanguination of the arm and inflation of a tourniquet up to 250 mm Hg, a 1.0-cm transverse incision is made along the proximal wrist crease in the ulnar side of the palmaris longus tendon. Subcutaneous dissection exposes the antebrachial fascia under surgical loupe. A transverse incision is made on the antebracheal fascia, exposing underlying ulnar bursa. Subligamentous dissection toward the fourth finger is carried out to reflect the synovial tissue from the undersurface of the transverse carpal ligament (TCL) and to create a space for the endoscopic device with a synovial elevator. A washboard sensation could be felt in the undersurface of the TCL with the elevator and its tip could be felt on the palm while it passes the distal part of the TCL. A slotted cannula is introduced into the carpal tunnel and a rigid 30°-angled 2.7-mm endoscope is inserted through the cannula. Manifestation of reduced transillumination could be observed in the palm while the endoscope is under the TCL. White transversely running fibers of TCL and a fat pad distal to the distal edge of the TCL can be seen on the endoscopic view. After ensuring that there are no intervening structures in the operative field, the TCL is incised proximally to distally with a forward-facing knife. After the TCL is completely cut out, both an escape of palmar fat into the carpal tunnel and retraction of cut edges of the TCL out of the endoscopic view could be observed as well as increased transillumination through the palm. A right-angled probe is used to palpate the divided TCL. The tourniquet is released. Wound closure is accomplished in layers following hemostasis and a bulky compressive dressing is applied.
Statistical analysis
Clinical severity and electrodiagnostic abnormality were compared between groups using chi-square test and demographic data including age and duration of symptoms was compared using Pearson's correlation analysis. Differences between groups were regarded as significant if p<0.05. All analyses were performed using SPSS, version 19.0, commercially available software package (SPSS Inc., Chicago, IL, USA).
RESULTS
Single-portal ECTRs were performed in 1194 hands of 793 patients with electrodiagnostically-proven idiopathic CTS from 2002 to 2011. Among 1194 hands, 570 hands of 388 patients with minimal 1-year postoperative follow-up were included in the study. Mean age of the patients was 53 years (range, 24-82 years) and mean follow-up period was 23.6 months (range, 12-160 months). Patients' clinical outcomes were assessed with postoperative improvement of tingling sensation, pain and numbness at 1, 3, 6, and 12 months postoperatively. Among 570 operated hands, 545 hands (95.6%) were satisfied and 25 hands (4.4%) were dissatisfied. We divided the 545 satisfied hands into early (group A) and delayed (group B) improvement group according to improvement period of 1 month.
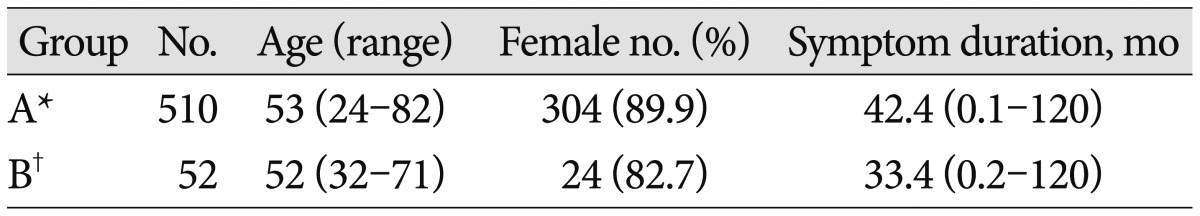
Group A included 510 hands in 338 patients with 304 males and 34 females. The mean age of group A was 53 years (range, 24-82 years). Group B included 35 hands in 29 patients with 5 males and 24 females. The mean age of group B was 52 years (range, 32-71 years). Mean symptom duration was 42.4 months in group A and 33.4 months in group B. Table 1 shows the baseline characteristics of the study groups. In group B, 11 hands improved in postoperative 2-months, 15 hands in postoperative 3-months and 9 hands in postoperative 6-months, respectively.
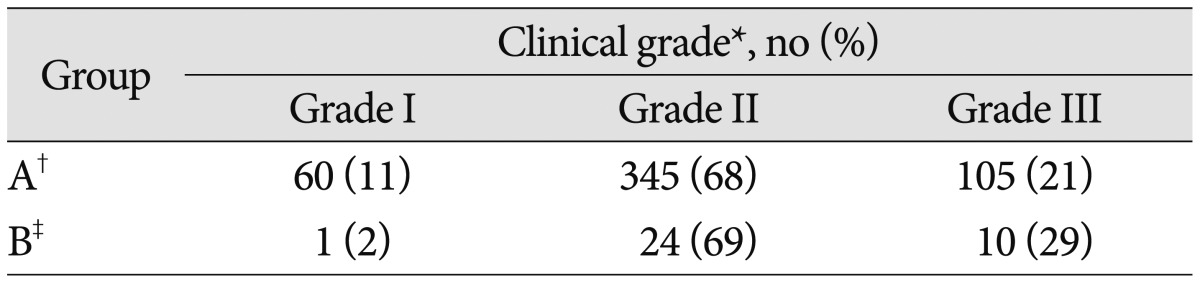
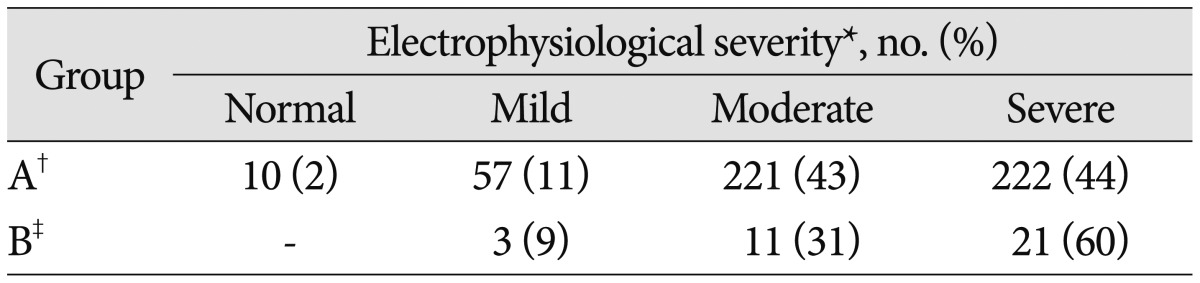
In group A/B, according to clinical severity, 60/1 hands were graded to I, 345/24 hands to II, 105/10 hands to III (Table 2). In group A/B, based on electrodiagnostic abnormality, 57/3 hands were divided to mild group, 221/11 hands to moderate group and 222/21 hands to severe group with normal findings in 10 hands of group A (Table 3). Statistical analysis of these results between groups did not reach significance (clinical severity : p=0.191, electrodiagnostic abnormality : p=0.294) but severity of electrodiagnostic abnormalities or clinical severity had a tendency to affect on delayed response. In addition, age and duration of symptoms did not affect the postECTR improvement period (age : p=0.478, duration of symptoms : p=0.1).
DISCUSSION
Classic symptoms of CTS include tingling sensation, pain and numbness in the median nerve distribution of the hand comprising the thumb, index finger, middle finger and radial half of the ring finger. However, sensory symptoms do not always involve the entire median nerve distribution of the hand. In some patients, the ring finger is affected. Regardless of distribution, symptoms generally progress gradually over time.
The primary pathophysiologic mechanism of CTS development is known as an increase in interstitial pressure in the carpal tunnel, leading to median nerve compression. The normal interstitial pressure in the carpal tunnel is known to be 2.5 mm Hg with the wrist in neutral position and it increases to approximately 30 mm Hg with the wrist in either maximum flexion or maximal extension26). Symptoms of the median nerve compression including tingling sensation develop when carpal tunnel interstitial pressure increases above 30 mm Hg, leading to a reduction of epineural blood flow, development of epineural edema and block in axonal transport26). With prolonged compression of the median nerve at higher carpal tunnel interstitial pressure, manifestations of the median nerve compression generally progress over a period of months to years to develop more severe sensory symptoms and even thenar muscle weakness.
There are numerous causes of this increase in carpal tunnel pressure but most cases of CTS do not have identifiable cause42). However, idiopathic CTS is believed to be caused by combination of an anatomically small carpal tunnel and changes in the tenosynovium of the flexor tendons in the carpal tunnel such as edema, vascular sclerosis and fibrous hypertrophy26). Secondary causes of CTS include neuropathic factor with diabetes, metabolic and physiologic factor such as hypothyroidism, rheumatoid arthritis and pregnancy, and space-occupying lesion with tumor or cyst42). In addition, risk factors in the general population that contribute to CTS include repetitive movement of wrist extension and flexion, obesity, rapid dieting, short height, hysterectomy without oophorectomy and recent menopause11). We excluded the cases with secondary CTS from the study because the predisposing conditions of an identifiable cause that contribute to CTS may affect the surgical outcome, other than known preoperative prognostic indicators8,23,30,43,44).
Decompression of the carpal tunnel is recommended when symptomatic discomfort interferes with work or activity of daily living despite conservative treatment or advanced CTS with thenar muscle weakness even when sensory symptoms are not disabling. In these cases, decompression of the carpal tunnel can be used to improve clinical symptoms and physical findings of CTS, to prevent progression and loss of hand function and to eventually minimize loss of time from work.
Two different types of surgical procedures are in use for the treatment of CTS : open and endoscopic release of the transverse carpal ligament. OCTR is the traditional option and is easy to perform with good symptomatic improvement and a low complication rate. Since the introduction of a less invasive carpal tunnel surgery using surgical endoscope by Okutsu et al.32) in 1987, several modifications of endoscopic technique have been described in the literature1,7,9,25). Endoscopic procedures have been widely used as an alternative treatment to OCTR, and single-portal Agee technique1) and two-portal Chow9) technique are the two most commonly used procedures. We used modification of single-portal Menon technique25) using a forward-facing knife to divide the transverse carpal ligament. It is beyond the scope of this study to describe details of each technique so we do not discuss it in this article. Since the introduction of endoscopic carpal tunnel surgery in the late 1980s, thereis still controversy regarding the efficacy, safety and complication rate of open and endoscopic procedures. Jimenez et al.22) reported that ECTR surgery offer similar success and complication rate compared to open surgery in an extensive review of published articles on ECTR surgery covering six different types of techniques. In addition, he described patients undergoing ECTR experienced less postoperative pain and earlier return to work or activity of daily living but endoscopic technique need a learning curve and surgical experience for a successful outcome. Ashwoth5) also described in a critical review of 57 review articles regarding ECTR that ECTR surgery, compared to open surgery, seemed equally effective at improving symptoms and hand function in short and long outcome, and it may be more effective at reducing time to return to work. Endoscopic surgery was reported to have more transient nerve injuries such as neuropraxia, numbness and paresthesia but open surgery to have more wound problems including scar tenderness, hypertrophic scar and infection. He also reported endoscopic surgery is more resource-intensive and demands a higher surgical skill than open technique.
Several studies have reported preoperative prognostic factors, affecting the outcome after surgical release of transverse carpal ligament and preoperative predictors included duration and severity of symptoms, grade of electrodiagnostic abnormalities, worker's compensation and work activity8,23,30,43,44). Good outcome has been associated with preoperative tingling other than anesthesia or weakness as well as good response to corticosteroid injection into carpal tunnel and poor result has been correlated with preoperative weakness or atrophy, associated diseases such as diabetis and thyroid disease, worker's compensation and heavy or repetitive work activity13,18,23,24,29,36,43,44). Clinical severity can have adverse effects on outcome in patient with CTS. The finding of delayed improvement in our series demonstrates late postoperative improvement group had more proportion of patient with severe clinical grade, but clinical severity did not differ significantly between early and late improvement groups. Even though we can expect poor outcome in patients with severe clinical grade of CTS, it is recommended that postoperative follow-up up to 6 months is necessary in idiopathic CTS patient without improvement. The duration of CTS has been shown to have no significant correlation with clinical outcome in patients undergoing carpal tunnel surgery19,43), whereas, other studies found worse outcome with longer duration2,13,24,27,29,30,44). Pauda et al.34) reported that the main positive prognostic factors of idiopathic CTS without treatment are short duration of symptoms and young age. Our study has indicated that the chronicity of CTS did not affect the time of improvement following ECTR. The role of NCS in predicting the outcome of carpal tunnel surgery is not clearly determined2,4,8,21,27,44). Schrijver et al.38) noted that NCS improved significantly at postoperative 12 months but only a modest correlation existed between relief of preoperative symptoms after surgery and the improvement of NCS. However, other studies showed that NCSs improve after surgery28). In severe CTS cases, nerve conduction studies results may not correlate with the clinical findings due to the varying nature of the impairment in different nerve fibers. In addition, nerve conduction studies will not accurately predict the recovery following release of the carpal tunnel, though neither do any of the other investigations predict this with any certainty6). Our study has shown that grade of electrophysiologic abnormalities does not correlate with the time course of improvement after carpal tunnel surgery, which means NCSs are not helpful to predict the improvement period.
Several studies demonstrate that improvements after carpal tunnel release decreased in older patients who were at risk of severe CTS, compared to a younger population14,15,16,20). Therefore, we can expect older patients to show a more delayed improvement than younger patients but we found no significant differences in the time of improvement following ECTR between early and delayed improvement group. In addition, worker's compensation can affect postoperative outcome and worker's compensation group showed diminished outcome, compared to patients without worker's compensation19). In our study, worker's compensation did not affect postoperative improvement period but we think it may delay postoperative improvement period. Therefore, worker's compensation status can be considered as a possible factor of delayed postoperative improvement in patients with worker's compensation.
CONCLUSION
Endoscopic decompression of carpal tunnel is effective as a primary or alternative surgical technique for the treatment of CTS, demonstrating symptomatic improvement within postoperative one-month in most patients. However, subpopulation of CTS patients can show delayed improvement postoperatively. Therefore, it is advised that postoperative observation for at least 6 months is necessary in the patients without symptomatic improvement to expect the delayed response.