Decompression of the Sciatic Nerve Entrapment Caused by Post-Inflammatory Scarring
Article information
Abstract
A rare case of chronic pain of entrapment neuropathy of the sciatic nerve successfully relieved by surgical decompression is presented. A 71-year-old male suffered a chronic right buttock pain of duration of 7 years which radiating to the right distal leg and foot. His pain developed gradually over one year after underwenting drainage for the gluteal abscess seven years ago. A cramping buttock and intermittently radiating pain to his right foot on sitting, walking, and voiding did not respond to conventional treatment. An MRI suggested a post-inflammatory adhesion encroaching the proximal course of the sciatic nerve beneath the piriformis as it emerges from the sciatic notch. Upon exploration of the sciatic nerve, a fibrotic tendinous scar beneath the piriformis was found and released proximally to the sciatic notch. His chronic intractable pain was completely relieved within days after the decompression. However, thigh weakness and hypesthesia of the foot did not improve. This case suggest a need for of more prompt investigation and decompression of the chronic sciatic entrapment neuropathy which does not improve clinically or electrically over several months.
INTRODUCTION
Sciatic nerve entrapment can occur from the pelvis to the distal thigh. The most common site is between the greater sciatic notch and ischial tuberosity12,14). The piriformis syndrome is caused by entrapment of the sciatic nerve at the level of the greater sciatic notch by the pyriformis muscle1,15). The clinical entity of piriformis syndrome is a matter of controversy13,15). Different theories exist to support the premise that the piriformis itself either compress or irritate the sciatic nerve12). Regardless of its prevalence, the diagnosis of piriformis syndrome should only be made after excluding all other potential causes of sciatica5,12,14,15). Even with this sophisticated preselection for surgery, surgery in patients with pyriformis syndrome is often unrewarding11,14).
The authors report a rare case of chronic sciatic nerve entrapment caused by post-inflammatory scarring, in which chronic, disabling pain of buttock and leg successfully relieved by surgical decompression.
CASE REPORT
A 71-year-old male patient presented with chronic, disabling buttock pain and right leg radiating pain for 7 years. He described a toothache-like pain in right buttock that occasionally radiated distally in right leg and foot, and diffuse hypesthesia and paresthesia along distal leg and foot. Sitting, particularly on a firm, hard chair, or on the common mode, and walking aggravated his symptoms. Straining during urination or defecation evoked shock-like pain in the right distal leg and foot. He also had an intermittent cramping, squeezing dysesthetic pain in his distal leg and foot. He had no back pain.
On physical examination, two dimple-like, old operation scars were observed in the right buttock (Fig. 1A). A moderate atrophy of right gluteal and harmstring muscles was observed and the circumferential diameter of right thigh decreased compared to the left side. Deep compression in his right lower buttock promptly elicited a cramping pain in the right buttock which radiated in the distal leg and, more excruciating pain, in dorsum and sole of the foot. He walked with an aid of cane. Neurologic examination revealed NMT grade IV+ weakness in the knee flexion. However, there was no motor weakness in the ankle and foot. Sensory examination showed moderate hypesthesia in his lateral calf, dorsum and sole of right foot. Ankle jerk was diminished in right side. No allodynia was observed. Rectal and urinary continence was preserved.
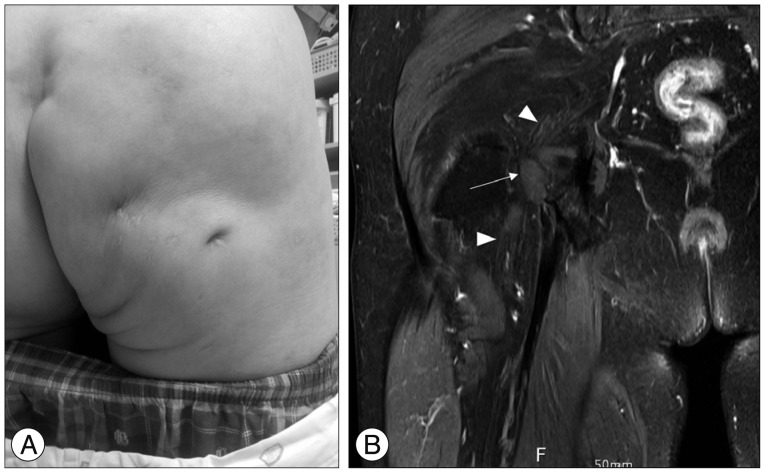
A physical photograph and magnetic resonance imaging showing the gluteal abscess in the right hip seven years ago. A : A photograph show-ing dimple-like postoperative scars in the patient's buttock. B : A gadolinium-enhanced T1 coronal image shows an irregularly enhancing band-like lesion (arrow) encroaching the sciatic nerve (arrowheads).
Seven years before admission, he underwent a drainage operation for right gluteal abscess and his postoperative course was uneventful. However, an intermittent cramping pain in his right buttock on sitting and walking developed gradually during the following 6 months after the operation, and intermittent paresthesia and dysesthetic radiating pain in his distal leg and foot appeared at 12 months. Since then, his buttock and right leg radiating pain gradually worsened with time. The right buttock and distal leg and foot pain did not respond to various types of non-steroidal anti-inflammatory drugs, muscle relaxant, and weak opioids (including ultracet and tramadol). The combination of oral oxycodone (20-40 mg/day) and antiepileptics (gabapentin and pregabalin) was somewhat helpful but not sufficient. Transdermal fentanyl caused a severe dizziness and nausea and he could not tolerated an antidepressant (amitryptyline 10-30 mg h.s.) for dry mouth and urinary retention. His visual analogue scale varied varied between 43-78. Physical therapy and repeated lumbar epidural blocks achieved only transient relief for 2-3 hours.
An MRI revealed an irregular granulation encroaching the sciatic neurovascular bundle around the pyriformis muscle (Fig. 1B). Under the diagnosis of sciatic nerve entrapment, exploration was performed.
The patient was positioned prone with the affected side elevated slightly and the knee minimally flexed. The classic incision for proximal lesion of the sciatic nerve from the posterior inferior iliac spine to midline of the posterior thigh, curving lateral to the gluteal muscles was made. After deviding the skin and subcutaneous tissue, the inferior margin of the gluteus maximus and the long head of biceps femoris were sought. Just lateral and deep to the long head of the biceps femoris, the sciatic nerve was found within a fat pad. Subcutaneous dissection was carried proximally beneath the gluteus muscle without deviding the gluteus maximus. After elevation of the subcutaneous flap over the proximal gluteal muscle along the course of the sciatic nerve, a fibrotic scar which was the consequence of the former drainage procedure done 7 years ago was found (Fig. 2A). With a transverse dissection between the gluteus maximus, the proximal sciatic nerve was found and followed. An irregularly fibrotic, tendinous band just beneath the piriformis muscle overlying the sciatic nerve was released while carefully avoiding an injury to severely compressed sciatic nerve (Fig. 2). The sciatic nerve was decompressed proximally to its exit from the sciatic notch and free passage of the finger was confirmed along the course of it. The obturator internus, gemelii, and quadratus femoris were visible. The posterior cutaneous nerve of the thigh was left intact. Postoperative course was uneventful. The intermittent shock-like pain in the leg and the cramping buttock pain on sitting, walking, and especially during voiding disappeared completely within one week postoperatively. The medication against neuropathic pain was withdrawn two weeks postoperatively. He remained pain free for the following one year postoperatively until his last follow-up at outpatient clinic. However, his long-standing thigh weakness and diffuse hypesthesia along distal leg and foot did not improve.
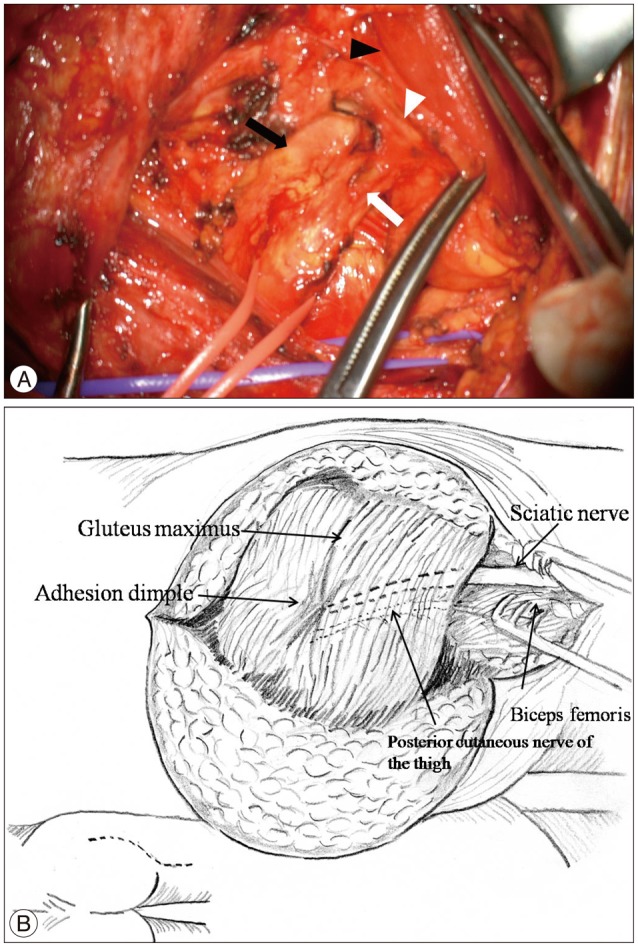
Intraoperative photographs showing sciatic nerve entrapment due to post-inflammatory adhesion scar. A : After dissecting the fibers of the gluteus maximus, severely compressed and flattened sciatic nerve (white arrow) was noted. The adhesion scar (white arrowhead) was elevated with Kelly clamp. The posterior cutaneous nerve of the thigh (black arrow) and piriformis muscle (black arrowhead) were found and neurolysis was done. B : A schematic drawing of the exposure.
DISCUSSION
Anatomy of the sciatic nerve
Formed by the L4-S3 roots, the sciatic nerve is the largest nerve in the body. The sciatic nerve exits the greater sciatic foramen as distinct tibial and peroneal divisions, enclosed in a common nerve sheath. In the pelvis, the sciatic nerve may descend anterior to, above, or through the piriformis muscle12,14,15). Variations of the sictic nerve/piriformis are well known12). In the distal thigh, the two divisions physically separate into tibial and common peroneal nerves. The sciatic nerve is the lifeline of the lower extremity. It provides knee flexion by innervation of the posterior thigh muscles and almost all sensory and motor functions below the knee12).
The piriformis muscle divides the greater sciatic region into supraspiriformis and infrapiriformis regions. The inferior gluteal neurovascular bundle, the sciatic nerve, and the posterior cutaneous nerve of the thigh pass in the lateral part of the infrapiriformis region. The piriformis muscle connects the sacrum and the greater trochanter, its main function is an external rotator of the hip with the leg extended and abductor of the hip when the thigh is flexed15).
Etiology of the sciatic nerve entrapment
Sciatic nerve irritation and compression can occur from pelvis to the distal thigh. The most common site is between the greater sciatic notch and the ischial tuberosity. Another site of sciatic nerve entrapment has been described due to the fibrous edge of the biceps femoris at the level of the ischial tuberosity in athletes10). Sciatic nerve compression can occur due to scar (following surgery, trauma, infection, injection), mass (e.g., bony impingement, cement, tumor, abscess, hematoma, entrometrioma), fibrous band, or vascular leash1,2,3,4,6,9,10). Dynamic factors such as leg crossing may also play a role in tethering the nerve. Direct injuries and stretch injuries to the sciatic nerve in the buttock could occur12,15).
Controversial concept of piriformis syndrome
Far more controversial is the clinical entity of piriformis syndrome12,13,14,15). Different theories exist to support the premise that piriformis muscle itself either compress or irritates the sciatic nerve. A widely held theory is that anatomical variations of the relationship of the sciatic nerve to the piriformis muscle predispose the sciatic nerve to entrapment by it5,7). Some believe that the sciatic nerve may be vulnerable to the entrapment lesions because it passes through or posterior to the piriformis muscle5,7). Others believe these normal variations are coincidental findings, and some postulated that piriformis spasm or degenerative or inflammatory changes in the piriformis cause compression against the bony pelvis and epineural irritation13).
Purist claim that an irritated nerve in the vinicity of the piriformis muscle is not proof of a cause-effect relationship13). In addition, they prefer to avoid the lavel syndrome and specify the cause, for example, sciatic nerve compression by synovial bursitis or posttraumatic scarring, rather than invoke a nondescriptive term (e.g., piriformis syndrome)7,13,14). As a results, some believe that the piriformis syndrome is underdiagnosed, many, overdiagnosed7,13). Regardless of its prevalence, the diagnosis of piriformis syndrome should only be made after excluding all other potential causes of sciatica12,14,15).
Clinical manifestation
Sciatic nerve compression typically produces local buttock pain with radiating symptoms into the distribution of the sciatic nerve. Patients may complain of painful dysesthesias or paresthesias, or painless hypoesthesias. Their symptoms may be worse with prolonged sitting, especially on hard surfaces (i.e., so-called wallet neuritis or hip pocket neuropathy)9,14,15). Patients may also note subtle weakness in the foot or toes, which may affect their gait. In more extreme cases, they may experience severe motor dysfunction in all muscles below the knee and hamstrings. Patients typically do not have back or hip symptoms12,14).
Sciatic nerve lesions may produce typical sensory disturbance or motor weakness in the sciatic nerve distribution2). In chronic cases, trophic changes may occur on the plantar aspect of the foot. Ankle and hamstring reflexes may be reduced in the affected limb, whereas the quadriceps reflex is preserved. Patients with sciatic nerve compression near the sciatic notch typically have localized pain between the posterior superior iliac spine and the greater trochanter. Frequently the diagnosis of piriformis syndrome is made without firm objective findings, and the diagnosis is largely a clinical one12,14).
Provocative test that stretch the piriformis include forced hip internal rotation with the thigh extended; Freiberg sign, resistence to abduction and external rotation; Pace sign, voluntary adduction, flexion, internal rotation of the hip; positive Lasègue sign. Hip external rotation may lessen pain12,14,15).
Diagnostic studies
High resolution MRI can delineate the sciatic nerve and its relationship to the piriformis muscle. Increased signal intensity or an enlarged sciatic nerve visualized on MRI in the region of the piriformis muscle is not specific for piriformis syndrome and may be suggestive of other pathologies, including inflammatory conditions, sarcoidosis, and lymphoma, to name a few differential diagnosis6). Asymmetry of the nerve compared with the contralateral side is helful, but not specific, because bilateral, fairly symmetric imaging abnormalities may be seen in patients with bilateral sciatic or lumbosacral neuropathies6,12). The interpretation of scans after piriformis injection should be done cautiously because the appearance of the piriformis and neighboring sciatic nerve may be altered following the procedure12,14).
Treatment of sciatic entrapment neuropathy
Nonoperative measures including nonsteroidal anti-inflammatory agents and medication to treat neuropathic pain, a course of physical therapy to stretch the piriformis and reduce spasm is helpful in many cases. Some have advocated injection with botulinum toxin A in relieving piriformis spasm. Trigger point injections may be helpful also12,14).
Surgery should be performed for patients with findings consistent with a diagnosis of sciatic neuropathy who do not improve clinically or electrically over -4 to 6 months12,14,15). However, it was suggested that surgery should be performed as a last option in patients diagnosed with piriformis syndrome who have failed nonoperative therapy and who have had all other diagnoses excluded. Even with this preselection, surgery in piriformis syndrome was often unrewarding11,12).
For localized pathology near the sciatic notch, a muscle-splitting approach thorough limited skin incision may be possible. For a more extensive dissection of the sciatic nerve, the approach with a modification of the Henry exposure of the sciatic nerve is needed8). The gluteus maximus can be detached from its insertion and reflected medially14). Neurolysis may include freeing fibrous bands or ligating enlarged veins. Some suggested intraoperative electrical studies are helpful in localizing the site of and determining the extent of neural injury, as well as prognosis on recovery12,14). In our case, we first localized the sciatic nerve just distal to the inferior margin of the gluteus maximus and followed its proximal course to sciatic notch. We found the dense adhesion scar resulting from previous drainage operation in the middle of the gluteus maximus, and a transverse muscle-splitting approach was done to find an entraped sciatic nerve without detatching the gluteus. An external neurolysis of the sciatic nerve was possible without much difficulty.
CONCLUSION
Sciatic nerve compression and entrapment can occur most commonly in the buttock level. Although compression of the sciatic nerve producing neurological symptoms and signs from mass lesion, scarring, and bony proliferation are well described, the report dealing surgical decompression of sciatic entrapment neuropathy is rare. Sciatic entrapment neuropathy caused by adhesion scar or inflammation around the sciatic notch should be decompressed surgically to avoid possible neurologic sequele as shown in this case.