Unilateral C1 Lateral Mass and C2 Pedicle Screw Fixation for Atlantoaxial Instability in Rheumatoid Arthritis Patients: Comparison with the Bilateral Method
Article information
Abstract
Objective
Bilateral C1 lateral mass and C2 pedicle screw fixation (C1LM-C2P) is an ideal technique for correcting atlantoaxial instability (AAI). However, the inevitable situation of vertebral artery injury or unfavorable bone structure may necessitate the use of unilateral C1LM-C2P. This study compares the fusion rates of the C1 lateral mass and C2 pedicle screw in the unilateral and bilateral methods.
Methods
Over five years, C1LM-C2P was performed in 25 patients with AAI in our institute. Preoperative studies including cervical X-ray, three-dimensional computed tomography (CT), CT angiogram, and magnetic resonance imaging were performed. To evaluate bony fusion, measurements of the atlanto-dental interval (ADI) and CT scans were performed in the preoperative period, immediate postoperative period, and postoperatively at 1, 3, 6, and 12 months.
Results
Unilateral C1LM-C2P was performed in 11 patients (44%). The need to perform unilateral C1LM-C2P was due to anomalous course of the vertebral artery in eight patients (73%) and severe degenerative arthritis in three patients (27%). The mean ADI in the bilateral group was 2.09 mm in the immediate postoperative period and 1.75 mm in 12-months postoperatively. The mean ADI in the unilateral group was 1.82 mm in the immediate postoperative period and 1.91 mm in 12-months postoperatively. Comparison of ADI measurements showed no significant differences in either group (p=0.893), and the fusion rate was 100% in both groups.
Conclusion
Although bilateral C1LM-C2P is effective for AAI from a biomechanical perspective, unilateral screw fixation is a useful alternative in patients with anatomical variations.
INTRODUCTION
Atlantoaxial instability (AAI) may be caused by trauma, arthritis, tumor, infection, or congenital malformation316). Atlantoaxial stabilization resulted from bony fusion is needed to correct deformities and prevent neurological impairment. The surgical method of C1-2 transarticular screw fixation was introduced by Margerl and has been the main technique for wire fusion of C1 and C2 vertebrae358). However, fusion rates may be altered by the depth of the vertebral artery (VA) groove of the lateral mass and the width of the C2 pedicle1). Additionally, screw fixation might be challenging due to the high risk of injury to the VA, which can lead to massive bleeding and cerebral infarction1620). Therefore, Goel and Laheri introduced C1 lateral mass and C2 pedicle screw fixation (C1LM-C2P), which was popularized by Harms and Melcher, to reduce the risk of injury to the VA56101116). Furthermore, in the inevitable situation of injury to the VA or in the case of unfavorable bone structures, C1LM-C2P cannot be performed using the bilateral method. Therefore, the aim of this study is to compare the fusion rates of the unilateral and bilateral methods using the C1LM-C2P technique.
MATERIALS AND METHODS
Between March 2009 and December 2013, 25 consecutive patients in our institution underwent C1LM-C2P to address AAI due to rheumatoid arthritis. Among those patients, basilar invagination was found in two.
Preoperative radiologic imaging studies were performed to obtain accurate information on the anatomy of the atlas and axis. Cervical X-rays, including hyperextension and hyperflexion views, were obtained to confirm the instability of the C1-2 complex. The atlanto-dental interval (ADI) was examined to determine the instability status at the preoperative; immediate postoperative; and 1, 3, 6, and 12-month postoperative periods. Moreover, computed tomography (CT) scans with 1-mm slices were performed to examine the potential insertion pathway of the C1 lateral mass screw and C2 pedicle screw, and CT angiography in the area of C1-2 was used to visualize the pathway of the VA for examining potential anomalies and reducing the possible complication of VA injury. Magnetic resonance (MR) images were studied to evaluate cervicomedullary compression.
Posterior C1LM-C2P screw fixation, the surgical technique of Harms and Melcher6), was performed in all patients in this study group. After discharge, patients reported to an outpatient clinic at postoperative months 1, 3, 6, and 12 to measure ADIs as the index of bony fusion. The evaluation of bony fusion was performed 12 months after the operation. Bony fusion was defined as a bony bridge which was seen at the C1-2 inter-spinous space on lateral radiograph images, no difference of ADI between the immediate postoperative period and the 12 month time point, and no instrument failure during the follow-up period21).
Operative technique
After wide exposure of the C1-2 posterior structures, the starting point in the C1 lateral mass was formed with a high speed drill at the connection point of the posterior arch and the lateral mass. After tapping the drilled pathway, screws with a diameter between 3.5 mm and 4.0 mm were inserted into the lateral mass. Before marking the entry point of the C2 screw, the medial border of the C2 pedicle was identified to prevent screw malposition in the spinal canal. After identification of the transitional corner, which is the more cephalad portion of the lamina and C2 isthmus, an entry point was made 4 mm lateral and 4 mm caudal to the transitional corner using a drill. The direction was 20° to 30° medial and cephalad, with palpation of the medial border of the C2 pars interarticularis. After drilling and tapering, a polyaxial screw with the proper length and diameter was inserted. An interlaminar spacer and wiring between C1 and C2 were tightly fastened, and the rod was applied to the screw head.
Statistical analysis
Preoperative and postoperative ADIs were measured on lateral plain radiographs using a Picture archiving and communication system (PACS) and then compared side-by-side to evaluate the time of bony fusion and differences between unilateral and bilateral screw fixation. Statistical analyses were performed with SPSS version 18.0 (SPSS, Chicago, IL, USA). Non-parametric analysis was performed in the both unilateral and bilateral screw fixation groups. If the p-value was greater than 0.05, bony fusion was assumed. The Mann-Whitney U test was used to compare the bony fusion rate between the unilateral and bilateral screw fixation methods.
RESULTS
Unilateral C1 lateral mass and C2 pedicle screw fixation was performed in 11 patients (44%) in this study (Fig. 1A). The mean age of the unilateral screw fixation group was 53.1 years (range 30-74) with female predominance (90.9%). An anomalous course of the VA was the main reason for unilateral screw fixation, which was required in eight patients. The other three patients harbored a narrowed pathway of screw insertion. Meanwhile, in the bilateral screw fixation group, the mean age was 55.9 years (range 40-72) with a female predominance (85.7%) (Table 1, Fig. 1B). Of the total patients, one showed VA stenosis compressed by the pedicle screw on digital subtraction angiography, but no other complications, such as neurologic impairment, massive bleeding, or infection, were found on further evaluation.

Postoperative images of the anteroposterior X-ray images of the C1 lateral mass and C2 pedicle screw fixation. A : Unilateral. B : Bilateral.
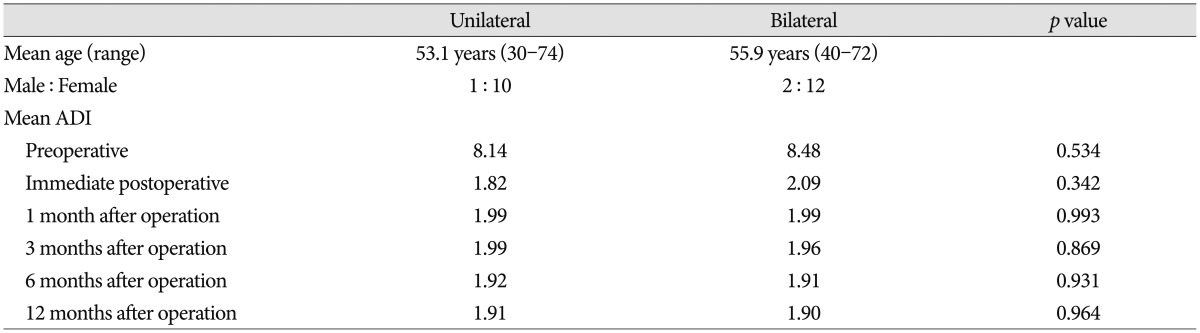
Demographic characteristics and atlanto-dental interval of patients with atlantoaxial instability surgically treated with C1 lateral mass and C2 pedicle screw fixation either unilateral or bilateral method
In the 11 patients in the unilateral screw fixation group, the preoperative mean ADI was 8.14 mm, and the mean immediate postoperative ADI was reduced to 1.82 mm. Moreover, measurements of mean ADI at 1, 3, 6, and 12 months postoperatively were 1.99 mm, 1.99 mm, 1.92 mm, and 1.91 mm, respectively. On the other hand, in the 14 patients in the bilateral screw fixation group, the mean preoperative ADI was 8.48 mm, and that at postoperative 1, 3, 6, and 12 months was 1.99 mm, 1.96 mm, 1.91 mm, and 1.90 mm, respectively (Table 1).
The postoperative ADI values at the immediate versus 1 month postoperative time points were not statistically different (unilateral group, p=0.241 and bilateral group, p=0.520). Similar results were found in the immediate versus 6 month time points unilateral group, p=0.859 and bilateral group, (p=0.052). Moreover, when comparing the whole follow-up period of 12 months for both techniques, no meaningful postoperative changes in ADIs were found, and atlantoaxial fusion was seen in all patients included in the study (100%). According to the Mann-Whitney test, there was no statistically significant difference between the unilateral and bilateral screw fixation groups (p=0.893) (Table 2).
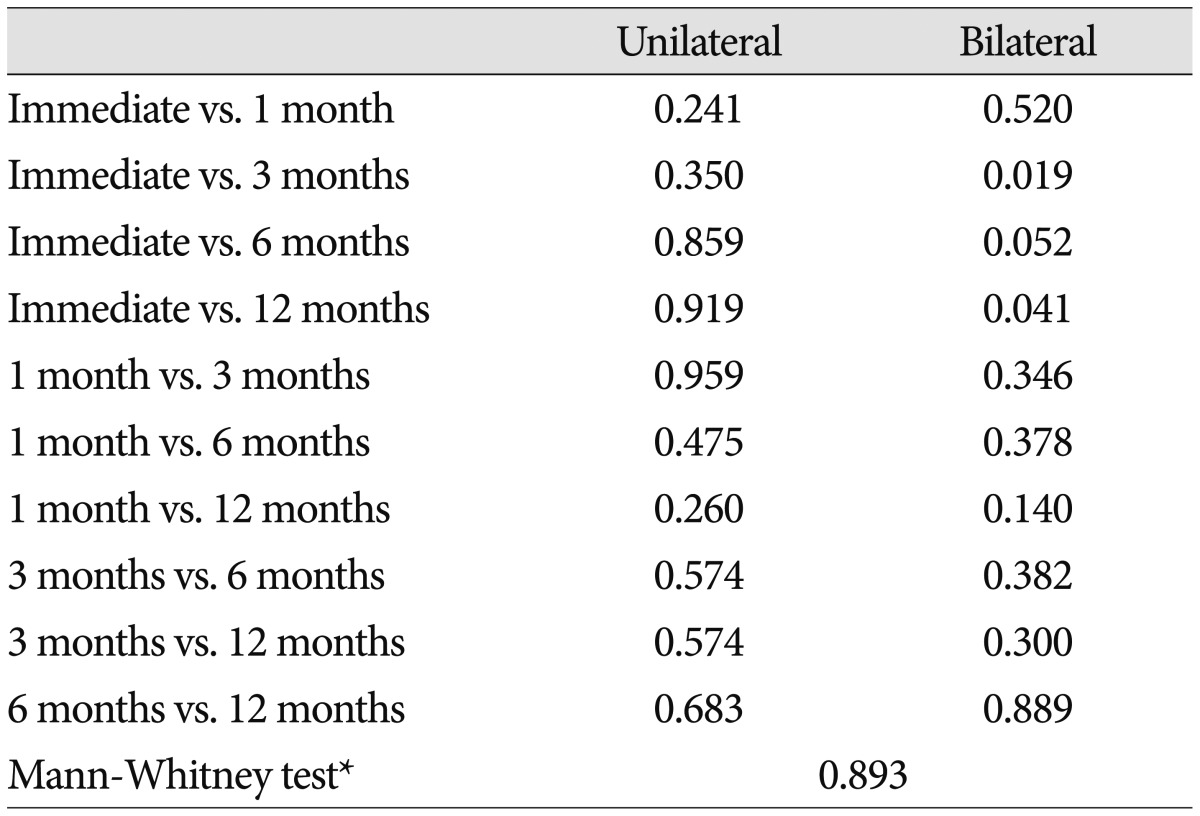
Statistical analysis between unilateral and bilateral groups on the basis of atlanto-dental interval measurement of bone fusion
When evaluating bony fusion at 12 months, instrument-related failure was not noted in any case. Bony bridge between the interlaminar space of C1-2 was demonstrated on CT scans in all patients. Differences in ADI between the immediate postoperative and 12 month time points were not statistically significant. Therefore, all enrolled patients achieved bony fusion without severe complications.
DISCUSSION
AAI may be caused by trauma, arthritis, or congenital malformations316). Chronic nuchal pain with or without neurological deficits may be encountered, and improperly treated upper cervical cord injury may trigger severe neurologic impairment.
The surgical method of C1-2 complex fixation has been introduced by many surgeons, and bilateral transarticular screw fixation using the wiring technique of Gallie or Brooks-Jenkins has achieved the highest stability and stiffness2712). However, bilateral transarticular screw fixation (TAF) is not always possible because of VA anomalies or fracture of the C1-2 complex1314). Therefore, stability achieved through bilateral TAF has been compared with that of unilateral TAF in a previous study. Hue et al.7) mentioned that there were no differences in fusion rate as measured by postoperative ADI change between unilateral and bilateral TAF.
To overcome the major complication of vascular and neural injuries, C1LM-C2P was introduced by Goel and Laheri in 1994 and modified by Harms and Melcher in 200156). The superiority of C1LM-C2P fixation compared to TAF is a lower risk of VA injury due to the use of individual screw systems. The pathway of the screws in the TAF method, which crosses C2 through C1, is relatively complex and narrow compared with that of C1LM-C2P, which uses individual screw systems. However, some problems have been encountered in bilateral screw placement including severe anomalous VA pathways and restricted pathway for the 3.5 mm screw. The aim of the present study was to avoid such situations. In other words, if the risk of injuring the VA and spinal cord can be predicted preoperatively, abandoning screw placement in an ipsilateral side with anatomical variation may be a wise decision. In the 25 patients enrolled in the present study, no massive bleeding or neurologic damage was detected. Vertebral canal violation without other complications was noted in one case of VA stenosis caused by a C2 pedicle screw. The risk of VA injury cannot be completely eliminated even with C1LM-C2P. If preoperative CT angiography suggests a high risk of VA injury, the screw may be inserted on the unilateral side only. Therefore, our study was designed to identify differences in bony fusion between unilateral and bilateral fixation. When we compared the preoperative and postoperative ADI measures, there was no statistically significant difference between unilateral and bilateral fixation (p=0.893). This suggests that unilateral and bilateral C1LM-C2P produce the same bony fusion and reduction of AAI. In addition, the strength of fusion in the unilateral screw fixation groups was as strong as that in the bilateral screw fixation group.
We have come into conclusion with the unilateral C1LM-C2P showed as much strength as the bilateral C1LM-C2P. Likewise, the unilateral TAF showed as much strength as the bilateral TAF, which was mentioned by Hue et al.7) Comparison between the unilateral TAF and unilateral C1LM-C2P should be made in the future study of AAI. However, intraoperative reduction and smaller surgical site exposure are the advantages of C1LM-C2P which is more selective in choosing surgical technique in AAI9).
Several studies have been performed to reduce the complication rate when stabilizing the C1-2 complex. VA injury is the main complication of C1LM-C2P screw fixation. Anatomical variations of the VA and C1 lateral mass deformation due to systemic diseases like rheumatoid arthritis may increase the risk of VA injury. Also, as the surgical procedure is performed, the risk of injuring the VA increases with every 2% when the screw is inserted3141620). Therefore, comprehensive understanding of the atlantoaxial and VA anatomy by CT angiography can assist with successful surgical planning and reduce the complication rate related to the VA.
Other possible complications are also possible with these techniques. Internal carotid artery and hypoglossal nerve injury may occur because of the anatomical proximity to the anterior aspect of the lateral mass315). C2 dermatome anesthesia or pain may result in patients with C2 ganglion injury due to insufficient exposure of the C1 lateral mass and C1-2 joint34).
Improvement in surgical devices has been accompanying development of surgical techniques. Such improvements in navigation systems and monitoring devices may allow for improved accuracy when determining screw trajectory pathways1316). However, these navigation systems have limitations with regard to calibration of three-dimensional CT scans with fluoroscopy-based images, inaccuracies caused by manipulating surgical instruments in the operation field, and motion of the operating field or craniocervical junction even when fixed with a head clamp16171819). Therefore, navigation systems require increased accuracy when operating on the C1-2 complex. Intraoperative fluoroscopy with abundant surgical experience can reduce complications in C1-2 surgical techniques16). There is no definite surgical monitoring or assisting device to avoid VA injury. If there is a risk of VA damage, the choice to abandon predictable screw insertion will increase the safety and completeness of the surgical technique of C1LM-C2P screw fixation. Our study illustrated that unilateral screw fixation shows similar strength, bony fusion, and reduction rate as bilateral screw fixation.
Even though we were able to demonstrate that unilateral screw fixation is similar to bilateral fixation in terms of strength, bony fusion, and reduction rate, several limitations of our study must be considered. The existing limitations are a lack of retrospective study, small number of enrolled cases, and deficiency of the biomechanical study. Due to our small study cases, bony fusion has been made in the whole study group. Further prospective study using a multi-center design may help increasing the reliability of our unilateral surgical technique. Furthermore, future biomechanical studies using animal or human cadavers might provide numeric evidence supporting the present study conclusion.
CONCLUSION
C1 lateral mass and C2 pedicle screw fixation can performed in patients with AAI due to rheumatoid arthritis. Although bilateral fixation is the main treatment method for such cases, unilateral screw fixation can be performed if a neurovascular contraindication is predicted. In our study, by means of ADI changes, unilateral fixation showed similar strength to the bilateral fixation with bone fusion. Radiologic images, such as CT angiography with cervical three dimensional CT and MR images, should be performed to reduce the complications of C1LM-C2P prior to surgery.
Acknowledgements
This work was supported by the research fund of Hanyang University (HY-2012-G).
The English grammar was revised by eWorldEditing, Inc. supported by Hanyang University.