Mortality and Epidemiology in 256 Cases of Pediatric Traumatic Brain Injury: Korean Neuro-Trauma Data Bank System (KNTDBS) 2010–2014
Article information
Abstract
Objective
Among pediatric injury, brain injury is a leading cause of death and disability. To improve outcomes, many developed countries built neurotrauma databank (NTDB) system but there was not established nationwide coverage NTDB until 2009 and there have been few studies on pediatric traumatic head injury (THI) patients in Korea. Therefore, we analyzed epidemiology and outcome from the big data of pediatric THI.
Methods
We collected data on pediatric patients from 23 university hospitals including 9 regional trauma centers from 2010 to 2014 and analyzed their clinical factors (sex, age, initial Glasgow coma scale, cause and mechanism of head injury, presence of surgery).
Results
Among all the 2617 THI patients, total number of pediatric patients was 256. The average age of the subjects was 9.07 (standard deviation±6.3) years old. The male-to female ratio was 1.87 to 1 and male dominance increases with age. The most common cause for trauma were falls and traffic accidents. Age (p=0.007), surgery (p<0.001), mechanism of trauma (p=0.016), subdural hemorrhage (SDH) (p<0.001), diffuse axonal injury (DAI) (p<0.001) were statistically significant associated with severe brain injury.
Conclusion
Falls were the most common cause of trauma, and age, surgery, mechanism of trauma, SDH, DAI increased with injury severity. There is a critical need for effective fall and traffic accidents prevention strategies for children, and we should give attention to these predicting factors for more effective care.
INTRODUCTION
Although infectious and congenital diseases have decreased significantly as major causes of pediatric death owing to developments in modern medicine, traumas such as traffic accidents and falls have emerged as the major causes of death in children20). Among these, a traumatic head injury (THI) is a leading cause that can induce a long-term cognitive, behavioral, and personality disorders as well as death.
Unlike adults, children do not have fully developed central nervous system, and traumas and their prognoses in children differ in nature owing the differences in the head injury mechanisms and the structures of their skull2–6,11,17). In attempts to focus on this, there have been efforts to analyze pediatric THI; however, such efforts have been confined to patients admitted to single hospital, and there has been few nationwide epidemiologic survey. To this end, we conducted this study with the participation of multiple hospitals to analyze the clinical features of THI in hospitalized pediatric patients, determine effective treatments, and estimate prognoses.
MATERIALS AND METHODS
We conducted this study as a retrospective study using THI information collected by the Korean Neurotrauma Data Bank System (KNTDBS), which was established with participations of 23 university hospitals nationwide from 2010 to 2014. From a total of 2617 patients who hospitalized with THI, we analyzed data on 256 pediatric patients (under age 19) on gender, age, level of consciousness at admission with Glasgow coma scale (GCS), cause and type of trauma, whether or not surgery was performed, and the death rates.
We divided the child patients by age: infants (under age 1), preschoolers (age 1 to 5), schoolchildren (age 6 to 12), and adolescents (age 13 to 18). We classified the severity of each head injury based on GCS score as mild (13 to 15), moderate (9 to 12), and severe (3 to 8) groups. We only analyzed treatment outcomes in 184 cases for were conducted only in 184 cases for which the Glasgow outcome scale (GOS) scores were available, and we classified the outcomes as death (GOS I), poor outcome (GOS II–III), or good (GOS IV–V).
We classified specific injuries by type as skull fracture, epidural hemorrhage (EDH), subdural hemorrhage (SDH), subarachnoid hemorrhage (SAH) and intraventricular hemorrhage (IVH), pneumocephalus, diffuse axonal injury (DAI), brain contusion and parenchymal hemorrhage.
For statistical verification, we conducted the Chi-square test and Fisher exact test, using the statistical program SPSS version 20.0 (SPSS Inc., Chicago, IL, USA) for the analyses. We defined statistical significances as a p-value less than 0.05.
RESULTS
Demographic data
In total, 2617 patients were hospitalized with THI from 2010 to 2014, and 256 of these patients were children under age 19. By geographical distribution, there were 57 patients (22.3%) in Seoul, 13 (5.1%) in Gyeonggi-do and Incheon, 6 (2.3%) in Gangwon-do, 103 (40.2%) in Chungcheong-do and Daejeon, 5 (2.0%) in Jeonlla-do, 31 (12.1%) in Gyeongsang-do and Daegu, and 41 (16.0%) in Busan.
The mean age of the pediatric patients was 9.0±6.4 years. The largest proportion was the adolescents (38.7%), followed by the preschool children (Table 1).
The male-to-female ratio was 1.87: 1, and the male predominance increased as age increased (p<0.001) (Fig. 1).
Mechanism, type and severity of THI
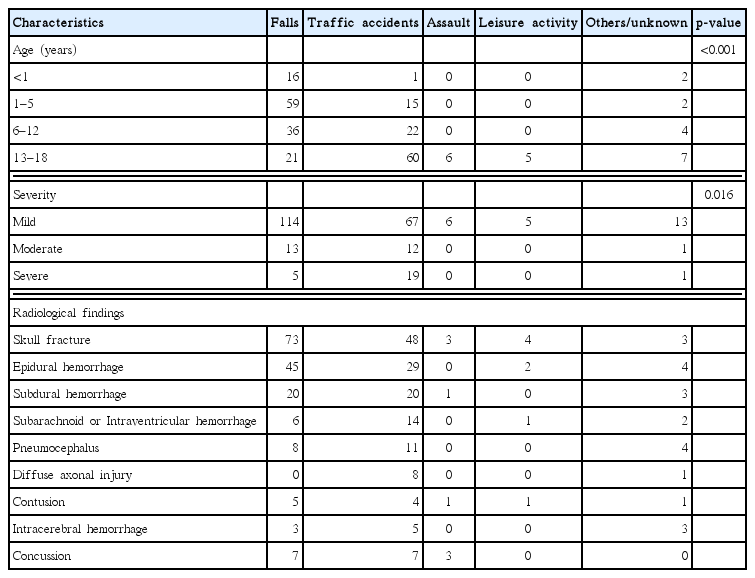
In terms of the mechanism of THI, falls were the most common cause followed by traffic accidents (Table 1).
By age, falls were the most common mechanism in the infants, preschoolers, and schoolchildren, but the adolescents showed a statistically significant higher rate of traffic accidents (p<0.001). By mechanism, skull fracture accounted for the largest proportion of injuries from both falls and traffic accidents, followed by EDH. By severity, mild THI was the most common (205 patients, 80.1%) followed by moderate (26 patients, 10.2%), and severe (25 patients, 9.8%). In the analysis of trauma mechanism by injury severity, falls were the most common cause of both mild and moderate head injury followed by the traffic accident. In patients with severe head injury traffic accidents were the most common cause (p<0.016) (Table 2).
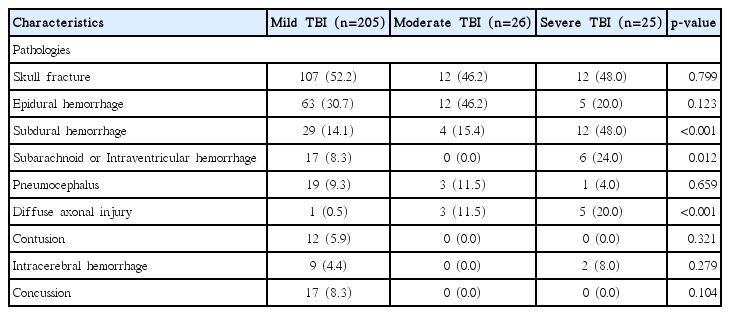
In terms of diagnoses by injury severity, skull fracture was the most common injury in patients with mild and moderate THI followed by EDH. In patients with severe head injury, skull fracture and SDH accounted for the highest proportions followed by SAH or IVH. In patients with severe head injury, SDH (p<0.001) and DAI (p<0.001) were more frequent, with statistical significance (Table 3).
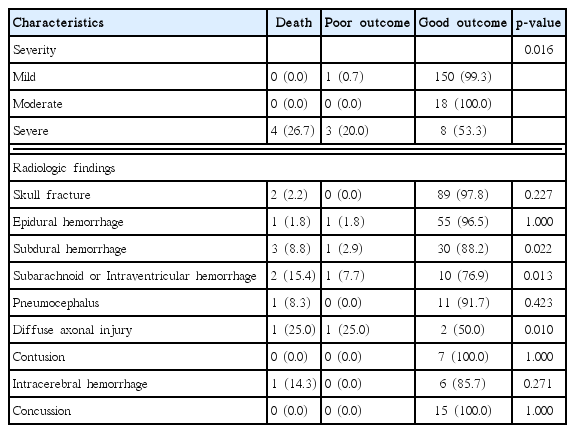
Treatment outcome
Treatment outcomes showed no statistical significance by injury mechanism (p=0.223) or age group (p=0.163). By injury severity, most patients with mild THI showed good outcomes, as did all patients with moderate THI. In the group with severe THI, eight patients (53.3%) showed good outcomes, three patients (20.0%) showed poor outcomes, and four (26.7%) had died. That is, the treatment outcomes were statistically significantly poor for severe head injuries (p<0.001). By specific injury diagnosis, in SDH patients, there were three deaths, one patient with a poor outcome, and 30 patients with good outcomes (p=0.022), whereas in the group with SAH or IVH, there were 2 deaths, one poor outcome, and 10 good outcomes (p=0.013). Among the DAI patients, one died, one had a poor outcome, and two had good outcomes (p=0.010). All results showed statistically significant differences (Table 4).
Outcome related to age, severity of traumatic brain injury and various pathologies induced by head trauma
A total of 34 patients had undergone surgery, and the patients also showed statistically significant lower GCS (p<0.001). There were three deaths (11.1%) among the 27 patients whose GOS scores were provided, one patient (3.7%) showed a poor outcome, and 23 patients (85.2%) showed good outcomes.
Four patients died from traffic accidents, a three-year-old female and three male adolescents; all had been admitted to the hospital with severe THI. Three patients were acute-SDH and underwent craniectomy at the time of admission to the emergency center.
DISCUSSION
Owing to modern medical advances, the infectious diseases that had previously been the major causes of death in children decreased significantly in number, and trauma is now a leading cause of death in children in Korea20). In the United States, from 2002 to 2006, there were an average of 697347 pediatric patients with THI annually, and of these, 60032 patients were hospitalized and 6169 died19). The nationwide statistics are not yet available, but in a study conducted with pediatric patients admitted to the university hospital emergency rooms in five regions, pediatric THI patients accounted for 32.7% of all pediatric trauma patients12).
It has been reported in the United States that the most prevalent age group for pediatric head injury is 0 to 4 years, but the highest rate of head injury among inpatient is in the age 10 to 14 range19). One study in Korea conducted patients who were admitted to the emergency room also found that the most prevalent age group for head injury in children was 0 to 4 years12), but a study among inpatients found the highest prevalence among 6 to 10 years18). In this study, we found the highest prevalence of head injury among the adolescents age 13 to 18. The two studies above showed different age of prevalence. It appeared that the differences arose because infants with head injuries cannot express their symptoms, so their guardians brought them to hospital to have the injuries examined because of concerns about the potential sequelae, but many of the falls that had resulted in head injury in the infants and toddlers were low energy falls2), and most had resulted in minor damage that did not require hospitalization10,16).
As reported in previous studies and our study, there were more male pediatric patients than the female2,9,12,21), and in particular, THI incidences was most prominent among schoolchildren; the implication is that boys have more physical activities than girls.
Falls and traffic accidents account for the majority of injuries in pediatric head trauma2,7–9,12–14,19–21). We found similar results in this study. As age increased, the incidence of falls decreased but that of traffic accidents increased greatly. Seventy-three patients among the adolescents group were injured in traffic accidents, twice as many as in the younger groups. As age increases, the opportunity to travel independently increases, leading to increased chances of traffic accidents and increased incidence of damage from higher energy impacts. These are considered the reason that the severity of brain damage tends to increase with age. Thus, safety education is necessary regarding both falls and traffic accidents. Most of this education takes place among school-age children; it should remind them that preventing these accidents is the most important matter, and it should take place regularly both at school and at home.
In this study, we found that skull fracture was the most common injury at 51.2%, which was consistent with the results from a previous domestic study among hospitalized patients that reported injury rates of 45.6–57.3%8,13,14). The authors of that study reported that most cases of intracranial hematomas were EDH8,14), whereas in this study, we found the incidence of intracranial hematomas to be 31.3% EDH and 17.6% SDH.
In this study, severe brain damage had occurred at high level in patients with DAI, SAH or IVH, and SDH, and the patients with severe brain damage showed poor outcomes. These results were similar to the results of other studies that reported that low GCS score accompanied by DAI was important for the prognoses. Luerssen et al.15) reported that the ages of the children themselves acted as a prognostic factor, but Berger et al.1) found that age and prognosis were not related. In this study, there were no differences in prognosis according to age. Mortality rates in pediatric THI patients have ranged from 0.06–7.3% in different reports8,12,14,19,21), and we found a similar rate, 1.171%.
Most pediatric patients with THI show no specific sequelae and good prognoses, but the cases accompanied by DAI, SAH, and SDH show poor prognoses, and thus, it is necessary to observe these patients more carefully.
This study has a number of limitations. First, because of wide variation in hospitals and individual variation of registration, there was a potential selection bias. Second, we could not perform regional analysis because there were differences in the degrees of participation among the hospitals, even after considering their sizes and numbers of beds. Third, there was difference of numbers of hospitals among regions and a few large hospitals did not participate in the KNTDBS. Fourth, there were no details on the trauma mechanisms such as the height of the fall or whether the child was a pedestrian or was in the car during traffic accidents. Fifth, because of the retrospective nature of the study, we did not have complete control over the variables; data were missing or incorrect data in many fields, so we excluded data on 72 patients from the statistical analysis of outcomes. We also did not analyze other factors such as prehospital care, neuro-monitoring, or use of the anticonvulsant mannitol.
To overcome these limitations, the next KNTDBS project should be planned to provide specific registration guides and validated data and it is required that more hospitals, especially regional trauma centers, should participate in KNTDBS.
CONCLUSION
This study is the first study using KNTDBS, Korea’s version of a neurotrauma data bank system, on pediatric patients who were hospitalized with THI. We expect that this study can help to prevent THI in children and to better determine their prognoses when injuries do occur, make registration guides, and attract new participants. Additional studies are needed to enable early detection of patients who in particular may require more aggressive treatment through the use of more clinical information.
Acknowledgements
Authors are thankful to members of the KNTDB investigators include Bo-Ra Seo (Chonnam National University Hospital), Byeong-Cheol Rim (Chungbuk National University Hospital), Byung-Moon Cho (Hallym University Kangdong Sacred Heart Hospital), Sang Koo Lee (Dankook University Hospital), Ki-Seong Eom (Wonkwang University Hospital), Hyun-Ho Jung (Wonju Severance Christian Hospital), Jae-Hoon Kim (Eulji University Hospital), Jeong-Ho Lee (Daegu Fatima Hospital), Jong-Hyun Kim (Korea University Guro Hospital), Min-Su Kim (Yongnam University Hospital), Taek-Kyun Nam (Chung-Ang University Hospital), and Young-Jin Song (Dong-A University Hospital).