Fractionated Stereotactic Radiosurgery for Brain Metastases Using the Novalis Tx® System
Article information
Abstract
Objective
To evaluate the efficacy of fractionated stereotactic radiosurgery (FSRS) performed using the Novalis Tx® system (BrainLAB AG, Feldkirchen, Germany; Varian Medical Systems, Palo Alto, CA, USA) for brain metastases.
Methods
Between March 2013 and July 2016, 23 brain metastases patients were admitted at a single institute. Twenty-nine lesions too large for single session stereotactic radiosurgery or located in the vicinity of eloquent structures were treated by FSRS. Based on the results obtained, we reviewed the efficacy and toxicity of FSRS for the treatment of brain metastases.
Results
The most common lesion origin was lung (55%) followed by breast (21%). Median overall survival was 10.0 months (95% confidence interval [CI], 4.9–15.0), and median progression-free survival was 10.0 months (95% CI, 2.1–13.9). Overall survival rates at 1 and 2 years were 58.6% and 36.0%, respectively. Local recurrence and neurological complications affecting morbidity each occurred in two cases.
Conclusion
FSRS using the Novalis-Tx® system would appear to be an effective, safe noninvasive treatment modality for large and eloquently situated brain metastases. Further investigation is required on a larger number of patients.
INTRODUCTION
Traditionally, stereotactic radiosurgery (SRS) is performed in a single session using a rigidly attached stereotactic guide device or some other immobilization technology with or without a stereotactic image-guidance system [13,16]. However, single-dose radiosurgery raises concerns of morbidity when high therapeutic doses are used or the target lesion is located in or near eloquent structures. Therefore, during recent years, SRS has increasingly been performed using up to five sessions, that is, by fractionated stereotactic radiosurgery (FSRS) [2,11].
In this study, we describe our institute’s experience of FSRS and discuss the efficacy of FSRS for the treatment of brain metastases.
MATERIALS AND METHODS
Between March 2013 and September 2016, 24 patients with 30 lesions were treated by FSRS (8–12 Gy×2–3 fractions) using the Novalis Tx® system (BrainLAB AG, Feldkirchen, Germany; Varian Medical Systems, Palo Alto, CA, USA) at a single institute. One case did not participate in follow-up and was excluded, and finally 23 patients with 29 lesions were included in the study. All patients selected for FSRS had large brain metastases, defined a tumor diameter of >3 cm or a volume of exceeding 15 mL. FSRS was also used to treat patients with brain metastases and a large postoperative remnant tumor or tumor bed. All metastatic lesions were located near an eloquent structure, which raised concerns of complications had single fraction SRS been performed. We reviewed all patient characteristics included Karnofsy performance status (KPS) scores.
FSRS
All FSRS procedures were performed using the Novalis Tx® system (BrainLAB AG; Varian Medical Systems) using a customized mask to achieve immobilization. All patients underwent a planning computed tomography (CT) scan and contrast-enhanced T1-weighted magnetic resonance imaging (MRI) for guidance purposes. Gross tumor volume was calculated using contrast-enhanced T1-weighted MRIs. To calculate planning target volume, 2–3 mm was added to enhanced margins. All 24 patients were treated using 2 or 3 fractions at fractional doses of 8–12 Gy. Fractions were administered on consecutive days. Twenty-three of the patients were followed monthly to evaluate neurologic status and complications, and 3 monthly to evaluate tumor control and radiation necrosis by contrast-enhanced MRI.
Efficacy and toxicity
Brain metastases were classified using the ‘‘Response evaluation in solid tumors (RECIST) criteria” [5]. Local tumor control was defined as an unchanged or reduced tumor volume by follow-up MRI based on RECIST definitions of stable disease or complete and partial response, respectively. If patient expired before first radiologic follow-up, we excluded these patients from local tumor control evaluation. Overall and progression-free survival were analyzed using Kaplan-Meier methods (IBM SPSS Statistics ver. 22.0 for Windows; IBM Co., Somers, NY, USA). Overall survival was defined as time elapsed between FSRS completion and date of death or last follow-up visit, and progression-free survival (PFS) was defined as time elapsed between FSRS completion and intracranial disease progression or death without intra-cranial disease progression.
Neurological status and complications were noted and rated according to Radiation therapy oncology group (RTOG) central nervous system toxicity [4].
Results
Patient characteristics
Twenty-three patients (29 metastatic lesions) were included in the study. There were 11 men and 12 women of median overall age 61 years (range, 48–78 years) (Table 1). Median KPS score before treatment was 71 (range, 50–90) and 31.0% of patients had a score of <70. Primary cancer sites were; lung (16 lesions/55%), breast (6 lesions/21%), stomach, colon, and ovary (Table 1). Brain metastases were located in cerebellum (12 lesions/41%) or frontal lobe (7 lesions/24%) (Table 1). Twentyone lesions (72%) were treated initially by FSRS, and the remaining eight (28%) underwent FSRS to treat resection cavities after surgical resection or to treat tumors that were difficult to approach or too close to eloquent structures to be removed. Mean planning target volume was 18.0 cm3 (range, 1.4–54.0) at time of FSRS, and three fractions were used in treat all lesions except one (2 fractions). Mean total FSRS dose was 30.17 Gy (±2.66).
Efficacy and toxicity
The 1-year local control rate was 91.7% and it was equal to the overall local control rate. Median overall survival and median progression-free survival were both 10.0 months (95% confidence interval [CI], 4.9–15.0 and 95% CI, 2.1–13.9, respectively) (Fig. 1). Overall survival rates were 58.6% and 36.0% at 1 and 2 years, respectively, and progression free survival rates were 58.4% and 31.3 % at 1 and 2 years.
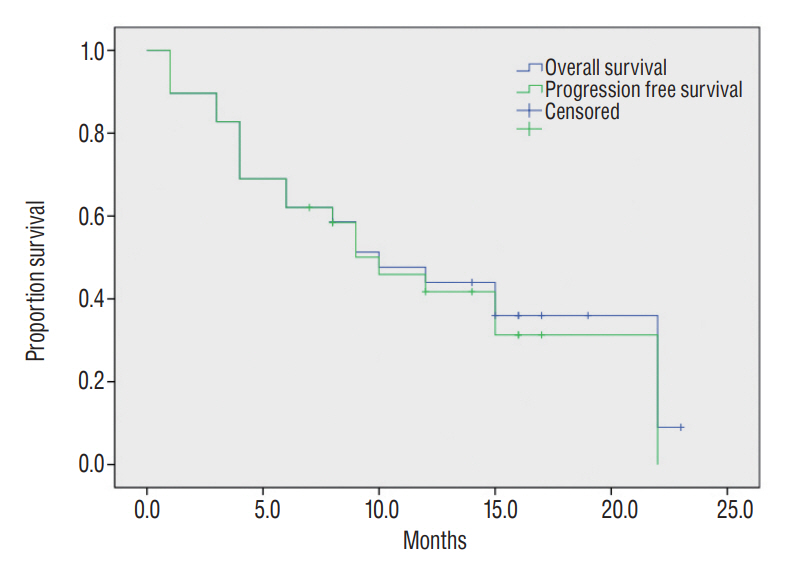
Overall and progression free survivals of patients that underwent FSRS for brain metastases. FSRS : fractionated stereotactic radiosurgery.
RTOG toxicity was ≥grade 3 for 2 of the 29 lesions (6.9%). Radiation necrosis post-FSRS, as indicated by imaging study occurred after treating 3 lesions (10.3%). Neurological complications occurred after treating five lesions (seizure for 3 and ataxia for 2). Therefore, the overall complication rate after FSRS was 17.2%.
DISCUSSION
In 1951, Leksell [13,14] coined the term “stereotactic radiosurgery” for a technique involving a combination of stereotaxy, a guide device, and radiotherapy, and in 1967, was the first to use SRS to treat a patient using a gamma knife. SRS has since evolved into a universal therapy in parallel with developments made in radiotherapeutic machines and imaging techniques [15], and in particular, it now includes multi-dose procedures. The biological effects of SRS are due to irreversible cellular damage and vascular occlusion, and thus, SRS has the potential to damage normal tissues around target volumes [3]. However, if radiation is administered in a fractionated manner it does not damage surrounding tissues to the same extent, because it better enables cellular reoxygenation and target volume redistribution, and thus, FSRS better preserves normal tissues than single dose SRS [7].
SRS is one of treatment options for brain metastases [1,23]. FSRS is also an effective treatment for brain metastases and has advantage over SRS. FSRS can treat larger tumors than SRS. Larger lesions are usually considered to be radioresistant because they contain many hypoxic cells. FSRS promotes cellular reoxygenation to tumor cells, and can cause them to go through a radiosensitive phase [21].
We used a thermoplastic mask for patient immobilization as this reduces intrafraction motion to <7 mm and interfraction motion to ~2 mm [8,25]. However, the effectiveness of noninvasive immobilization systems have not been clearly demonstrated for FSRS, although advanced image guidance systems and the addition of margins to target volumes improve accuracy and precision [10,24]. Furthermore, the dose per fraction for FSRS is under 10 Gy, which the tolerable limit for single fraction radiation administered to critical intracranial structures [12,17,18].
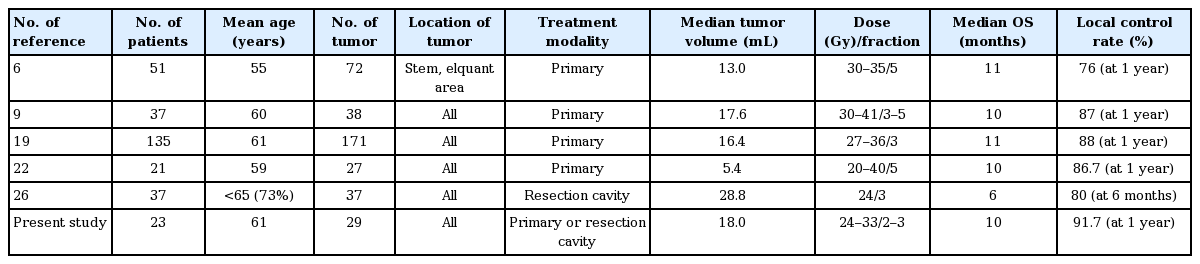
Previous studies showed FSRS provides an effective means of treating brain metastases (Table 2), and that the 1-year survival rate is ~60% and the local control rate ~90%, which are equivalent to results obtained using other modalities [6,19,22]. In the present study, mean planning target volume was 18.0 cm3 (range, 1.4 to 54.0). Usually a lesion diameter of >3 cm is considered a controversial indication for SRS, which provides encouraging empirical evidence that FSRS, unlike SRS, is effective for large lesions. Furthermore, FSRS has also been demonstrated to provide a substantial measure of local control, as average lesion size in these previous studies ranged up to 16 mL [19,26]. Accordingly, reports indicate FSRS probably provides effective treatment for large tumors.
Normal tissue protection is an expected benefit of FSRS. In present study, the rate of all complications was 17.2%, which is higher than reported by others [6,9,19,22,26], although the RTOG toxicity rate was similar to that reported in these previous studies. We speculate that the larger tumors enrolled in the present study explain the higher mild complication rate. According to Murai et al. [21], 27–30 Gy in three fractions or 31–35 Gy in five fractions might increase brain necrosis more than other regimens. In the present study, FSRS was performed in most cases using 30 Gy in three fractions, and although not detected during post-FSRS radiologic examinations, it is likely that this schedule was associated with the high rate of mild symptoms observed. Minniti et al. [20] compared SRS with FSRS and reported that incidence rate of radiation necrosis of SRS was twice as higher than FSRS (20% vs. 8%). In the present study, the rate of radiation necrosis was 10%, which is similar to those reported in previous studies [6,9,19,22,26].
The obvious limitation of the present study is its small cohort size. However, the results obtained, like those of previous studies, indicate FSRS provides an effective means of treating brain metastases, especially when tumors are large or surrounded by a critical structure. In order to prove the efficacy of FSRS, a large cohort study and a randomized controlled trial versus conventional radiotherapy are needed.
CONCLUSION
We conclude FSRS, using the Novalis Tx® system (Brain-LAB AG; Varian Medical Systems), offers an effective and safe noninvasive treatment modality for different intracranial lesions. Furthermore, based on our experiences, we consider FSRS a safe modality for brain metastases that are large or located in an eloquent area. However, this study is limited by its small cohort, especially with respect to the assessment of the treatment. Therefore, we suggest additional studies be undertaken to determine the efficacy of FSRS for brain metastases.
Notes
No potential conflict of interest relevant to this article was reported.
INFORMED CONSENT
Informed consent was obtained from all individual participants included in this study.