Narrative Review of Pathophysiology and Endoscopic Management of Basivertebral and Sinuvertebral Neuropathy for Chronic Back Pain
Article information
Abstract
Chronic lower back pain is a leading cause of disability in musculoskeletal system. Degenerative disc disease is one of the main contributing factor of chronic back pain in the aging population in the world. It is postulated that sinuvertebral nerve and basivertebral nerve main mediator of the nociceptive response in degenerative disc disease as a result of neurotization of sinuvertebral and basivertebral nerve. A review in literature is done on the pathoanatomy, pathophysiology and pain generation pathway in degenerative disc disease and chronic back pain and management strategy is discussed in this review to aid understanding of sinuvertebral and basivertebral neuropathy treatment strategies.
INTRODUCTION
Chronic back pain is a leading cause of disability in patients presenting to spine surgeons [103]. Despite changes in terms of health care and geopolitical advancement, the pattern of lower back pain as a leading cause of musculoskeletal disability is still unchanged from 1990 to 2010 [100]. Diverse biopsychosocial associations had been attributed as a cause of lower back pain [93,95]. Among the various spinal conditions, degenerative disc disease is the commonest cause of lower back pain globally [22]. Lower back pain is also one of the most common symptoms leading to lumbar spinal fusion [67,101]. Sinuvertebral and basivertebral neuropathy were described by several authors as the one of the key contributing factors for discogenic lower back pain [29,43,44,80,88]. In this narrative review, we discussed the pathophysiology and management of sinuvertebral and basivertebral neuropathy.
TYPES OF LOWER BACK PAIN
Borenstein et al. [13] described six categories of spinal pain. The categories are : 1) superficial somatic pain which involves skin and subcutaneous tissue mediated by cutaneous A fibers, it presents with sharp pain in condition like cellulitis and burning pain in herpes zoster. 2) Deep somatic (spondylogenic) pain felt by muscles, fascia, periosteum, ligaments, joints, vessels and dura are mediated by sinuvertebral nerve and posterior primary ramus (medial branch) which is unmyelinated, it can present acutely with sharp pain such as muscle strain or chronic dull ache in arthritis. 3) Radicular pain is mediated by spinal nerves presents with segmental radiating and shooting pain described by patients with conditions such as herniated intervertebral disc, foraminal and/or spinal stenosis. 4) Neurogenic pain mediated by mixed motor sensory nerves which present with burning pain. 5) Viscerogenic referred pain mediated by autonomic sensory, unmyelinated C fibers involving large surface area which presents with various manifestation such as deep heaviness, boring, tearing or colicky pain. And 6) psychogenic pain. Among these six categories, spine surgeon often treats patient with deep somatic and radicular pain. These categories of pain are mediated by medial branch, sinuvertebral nerves and basivertebral nerves (BVNs) for deep somatic and spinal nerves for radicular pain [13]. Centralization of pain can occur when pain becomes chronic with pathological neuronal pathways formed (neurotization) and sensitization of nociceptive nerves [31].
ANATOMY OF INTERVERTEBRAL DISC AND PATHOANATOMY OF DEGENERATIVE DISC DISEASE
Intervertebral disc allows load distribution as a shock absorber, it distributes the weight and impact sustained during the movement of spine [68]. The shape, structure and mechanical properties of intervertebral disc adapts to the loads and stress patterns experienced daily [77]. Degenerative disc is a cause of spinal malalignment [73]. It is known that matured intervertebral disc is avascular and aneural, the supply of nutrients is achieved by passive diffusion from adjacent end plate vessels and pre-disc vessels reaching outwards in centrifugal pattern from the inner layer to outer layer of disc [81]. Intervertebral disc consists of nucleus pulposus (NP), annulus fibrosis (AF) and the cartilage of adjacent vertebral endplates [10]. Degenerative disc disease occurs due to multifactorial causes which can be divided into : 1) non traumatic degeneration triggered by decrease in nutrient distribution coupled with changes in the composition of extracellular matrix due to aging [69]. Central to pathoanatomical changes in degenerative disc disease is chondrocyte like cells necrosis in NP which occurs naturally but tends to occurs in accelerated rate as patient ages. This necrosis process leads to cartilage-collagen interphase degradation, subsequent formation of syndesmophyte and calcification at adjacent vertebra [2]. 2) Traumatic degeneration in the intervertebral disc in response to microtrauma accumulated over time and leads to mechanical annular fissure and nucleus damage [35]. After traumatic and/or non traumatic event happened in lumbar intervertebral disc, numerous macro and microscopic changes in the disc eventually lead to degeneration and pain sensitization of lumbar intervertebral disc. Microscopic damages in the disc triggers cytokine secretion which in turn leads to immune cell migration with more cytokine secretion. These cytokine signals the increase in neutrophils proliferation and associated nerve ingrowth and sensitization of spinal nerve contributing to lower back pain [20,98]. Genetics, aging, smoking, repetitive mechanical movements over time leads to decrease nutrient availability, structural changes, inflammation of intervertebral disc and neovascularization and neoinnervation in the inflamed degenerated discs which subsequently leads to back pain [51].
PATHOGENESIS OF LOWER BACK PAIN
Progressive damage to intervertebral disc in disc degeneration leads to decrease in disc height [33]. Loss of disc height leads to a series of changes in spinal segment. Loss of disc height leads to microsubluxation of facet joints which often required a healthy disc height to maintain its optimal joint function [89]. Microsubluxation leads to pathoantomical changes of facet joints such as facet hypertrophy, capsular contracture and hypertrophy, increase stiffness of spinal segment and subsequent muscular contracture of the spinal segment [4]. There is an increase incidence of spinal instability among patients with discogenic lower back pain [96]. The decrease in disc height also leads to buckling of ligamentum flavum into spinal canal secondary to disc generation is a leading cause of ligamentum flavum hypertrophy [5]. Overall effect on the spine ranges from lower discogenic axial back pain to radicular and/or neurogenic claudication.
ASSOCIATION OF MODIC CHANGES ON ADJACENT VERTEBRA END PLATES AND BODIES WITH DISCOGENIC BACK PAIN
There are studies showing adjacent vertebral end plates changes are evident in patients with discogenic back pain and suggested that pathological innervation focal points are at end plates region [24,59]. Modic changes (MC) are demonstrated as T1W and T2W signals in magnetic resonance imaging (MRI). They are the hallmark of degenerative disc disease. MC is more prevalent in patients with lower back pain (43%) compared to asymptomatic population of 6% median prevalence. It is postulated that end plates and adjacent vertebral bodies sustained damages during degenerative disc disease and manifested as MC in MRI [23]. Size of MC is associated proportionally to the severity of lower back pain [38]. Evaluation of disc, bone and cartilaginous tissue demonstrated similar gene expressions and cytokine pathways in the disc, end plate and vertebral bodies with MC suggesting cross molecular communication in pain generation for degenerative disc disease [24]. Perhaps target therapy should not be isolated in the disc alone, as evidence by radiofrequency ablation applied to adjacent endplates, pedicle region and vertebral bodies deployed in management discogenic back pain [39,48,50].
PATHOGENESIS OF NEURONAL SENSITIZATION LEADING TO HYPERESTHESIA
Inflammatory response from disc degeneration
As disc degeneration occurs, exposure of NP fragment from damaged AF leads to release of growth factors and cytokines with subsequent increase inflammatory cells in the region of damaged disc [16,72]. Several proposed growth factors, such as basic fibroblast growth factor and transforming growth factor-beta1; tumour necrosis factor (TNF)-α, interleukin (IL)-1β, nerve growth factor stimulates the production of macrophages and mast cells which attempt to repair the damaged annulus fibrosus in degenerated disc [74]. IL-1, IL-6, and COX 2 are some of the cytokines which are induced and postulated to be associated with pain related in degenerative disc disease [83]. Systematic review showed three biomarkers; i.e., TNF-α, IL-6, and interferon alpha, were linked with persistent back pain [11]. There is neovascularization and hypervascularity in end plates, and perineural fibrosis were found in patients who presented with symptomatic back pain who underwent endoscopic radiofrequency ablation. Kim et al. [48] further postulated that neovascularization and inflammation with adhesion formation is associated with pathological neuronal sensitization of nerve fibers at the annular fissures. Inflammation may leads to hypoxia and/or acidic local condition which increased bradykinin- stimulated calcium response which increased intervertebral disc and dorsal root ganglion susceptibility to pain [60]. As normal disc under physiological echanical stress does not result in pain, there is postulation that diseased disc are sensitized with ingrowth of nerve fibres in normally aneural disc, extending even to the deeper layers. These nerve fibers providing sensation of pain are the sinuvertebral and BVNs which are branches of the posterior primary ramus [57,90].
Anatomy of sinuvertebral nerve
Sinuvertebral nerve was first described by Dr. Hubert von Luschka in 1850 [99]. There is bilateral innervation by sinuvertebral nerve in every vertebral level. It innervates posterior longitudinal ligament (PLL), vertebral body and pedicles. It also gives rise to branches to intervertebral foramen and anterior spinal canal through neural anastomosis [14]. Studies showed that sinuvertebral nerve innervates posterior annulus fibrosus [25,52]. The sinuvertebral nerve receives contributions from two main sources : 1) somatic supplies from the ventral ramus of spinal nerve or directly from spinal nerve and 2) the contributions from gray ramus communicans which provides the autonomic supplies [12]. The classic description of sinuvertebral nerve, which is given rise by dorsal branch of posterior primary ramus as a somatic branch providing proprioceptive and nociceptive fibers and subsequently joined by grey ramus communicans to provide the sympathetic supply to sinuvertebral nerve. After the union of the somatic and autonomic nerve, sinuvertebral nerve runs a recurrent course to re-enter the spinal canal through the spinal foramen via the deep anterior intraforaminal ligament, lying medial to the pedicle cephalad to the corresponding disc [25]. Sinuvertebral nerve travels next to spinal branch of lumbar artery just ventral to dorsal root ganglion at the foramen of spinal canal. At the region just lateral to PLL, sinuvertebral nerve divides into a main ascending branch and a lesser descending branch where they interconnect with adjacent sinuvertebral nerve of the above or below level [32]. Sinuvertebral nerve takes a course at the superior part of Kambin’s triangle and Harm’s describe safe zone [34,64]. Care in transforaminal endoscopic approaches is important and there is a role of transforaminal approach to treat pain related to sinuvertebral nerve [45,48,50]. While the precise role sinuvertebral nerve plays in generation of discogenic back pain is yet to be fully understood, it is described as the most likely mediator of lower back pain related to the degenerative disc disease [14]. There is also debate in cadaveric dissection on whether sinuvertebral nerves are only autonomic origin [32], dual somatic in upper lumbar segment and purely autonomic at lower lumbar levels [82] while others are dual origin [14]. Breemer et al. [14] found at L2, 90% are derived from somatic and autonomic roots and at L5, 40% are somatic and autonomic roots, while the remaining are purely autonomic roots. Distribution of sinuvertebral nerve distribution is a matter of controversy as well, whether it is segmented at the spinal nerve of origin level or branching out rostrally and caudally in spinal canal [88]. It was described that the nerve divides into superficial and deep networks adjacent to the PLL. It is understood that the superficial network is primarily sympathetic and deep network is primarily somatic supplying annulus and PLLs [52]. Nakamura et al. [70] performed sympathectomy in rats and found that after sympathectomy, up to 90% loss of sensory fibres to the posterior annulus fibrosus in the rats. Other than supplying the annulus and PLL, sinuvertebral nerve supplies several other anterior spinal structures such as ventral and lateral surface of the dura mater and sparing the dorsal surfaces of dura, it also provides somatic supply to the periosteum of the vertebrae and the ligaments of facet joints. However, the sensation to the facet joint is supplied by medial branch of the posterior ramus rather than sinuvertebral nerves [87,94]. The sympathetic fibers of sinuvertebral nerves also innervate surrounding anterior spinal vasculature in the vertebral marrow, vertebral bodies, end plates, and outer annulus.
The neuronal message mediating substances and peptides had been investigated in several studies as the neuronal message carrier of sinuvertebral nerve. Substances such as tyrosine vasoactive intestinal polypeptide, substance P and calcitonin gene related peptide are found in superficial and deep divisions of sinuvertebral nerve. Similar substances are found in sympathetic nerve transmission peptides, providing evidence of sympathetic nerve supply of sinuvertebral nerve [1,19,36].
26% to 39% of patients who suffered from lower back pain has sinuvertebral nerve increased activity [62,86]. Sinuvertebral nerve is found to penetrate the annulus in differently in normal and diseased state, as there is a deeper penetration in the diseased state up to NP [8,63,75]. The mediator for the degree of penetration is hypothesized to be due to vascularized granulation formation triggered by degeneration of the disc, bringing in neurotropic factors to promote the pathologic deeper penetration of sinuvertebral nerve fibers to inner disc [75,78]. It is found that sinuvertebral nerve fibers are more densely populated in the end plates of degenerated disc than normal disc [27]. Studies demonstrated that once sinuvertebral nerve penetrated deeply to encroach NP, there is associated side effects such as inflammatory cells accumulation, neural irritation and increased capillary permeability and nerve stimulation [16,71]. Kim et al. [48] found that patients who had sinuvertebral and BVN pain may present with radicular pattern of pain despite no direct neural compression seen in radiological and endoscopy, however there is inflammation around the region of sinuvertebral nerve distribution observed in the endoscopic radiofrequency ablation [18,44].
Anatomy of BVN
BVN derived from sinuvertebral nerve as a paired nerve branches supplying the end plate as pain nociceptive transmission [23,24,59]. Sinuvertebral nerve gives rise to BVN upon entering through central vascular foramen into vertebral body alongside basivertebral vessels and continues to branch out to supply different parts of the end plate [15,29]. The pain mediating substances are found to be substance P, protein S-100, PGP 9.5 and CGRP [6,9,30,53]. Similar to sinuvertebral nerve, BVN has increased density in proportion to the amount of disc damage, playing an important role in generation of chronic back pain [59].
Hyperesthesia and centralization of pain
As inflammation and subsequent neuronal sensitization occurs, normal mechanical movement can generate a painful response. Mackenzie [61], as far back as 1893 proposed that increased sensitivity of structures in central nervous system due to injury creates an “irritable focus” in the spinal cord segment at where the signals are transmitted. Centralization describes a theory that pain which started in spine referred distally and subsequently retreats back to axial back pain in response to repeated movements and/or guided positioning. Understanding of centralization can help guide physiotherapy and psychotherapy management in these patients [3]. Chronic pain in degenerative disc disease with subsequent hyperesthesia and centralization leads to some of the patients feeling significant axial back pain from performing routine spinal movement, over time avoidance behavior may occur and leading to subsequent paraspinal muscle atrophy and contracture (Figs. 1 and 2) [28].

A : Axial cut of nerve distribution in a normal patient. Sinuvertebral and basivertebral nerve supplies the disc and adjacent end plate while medial branch of posterior primary ramus supplies facet joint. B : Axial cut of nerve distribution in a patient with facet subluxation. Facet subluxation leads to capsular laxity and subsequent widening of the facet joint, medial branch perceived subluxation as pain stimulation leading to the facet joint paint(red stained facet joint). C : Axial cut of nerve distribution in a patient with facet subluxation as well as advanced degenerative disc. Facet subluxation leads to capsular laxity and subsequent widening of the facet joint, medial branch perceived subluxation as pain stimulation leading to the facet joint pain (red stained facet joint) and there is also concurrent neuronal sensitization of sinuvertebral and basiverterbral nerve (red stained end plate) as well as facet joint pain.
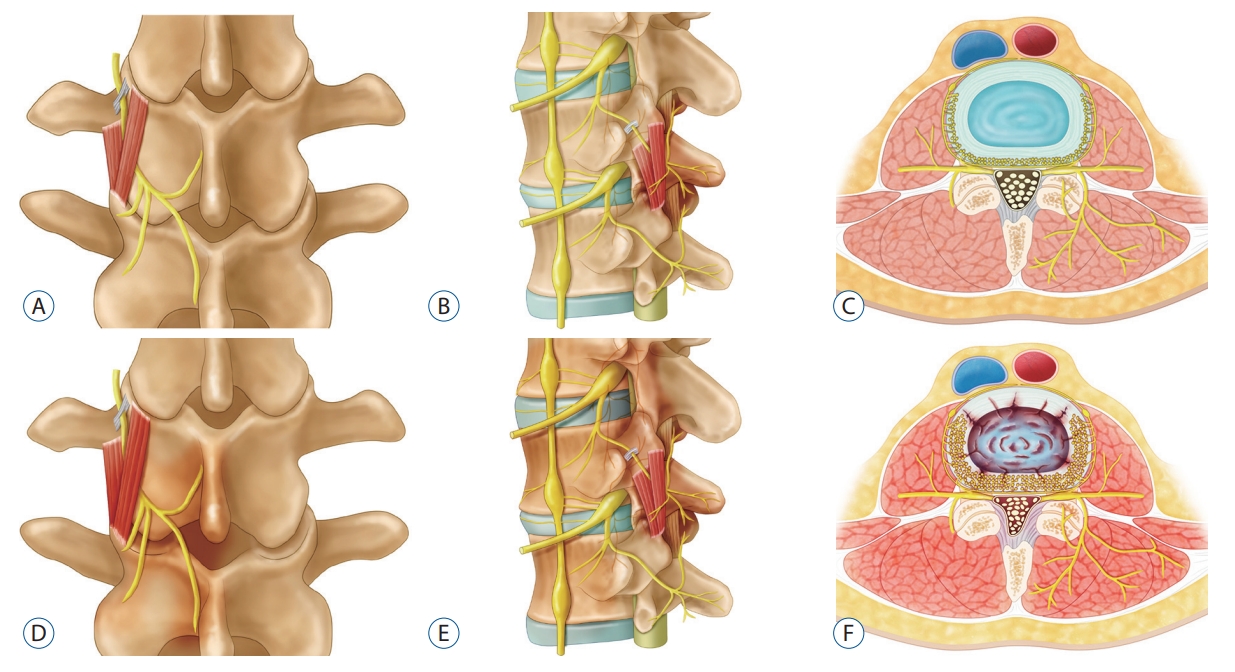
A-C : Coronal and sagittal picture of medial branch of posterior primary ramus in normal patient which traverses through fibro-osseous canal bounded by accessory process, the mammillary process and mammilloaccessory ligament and subsequently exits through the intermammillary fascicle and mamillostyloid fascicle of multifidus muscle, in Fig. 2c sinuvertebral and basivertebral branches of medial branch nerve supplies the disc. D-F : Coronal and sagittal picture of medial branch of posterior primary ramus in patient with degenerative disc disease and facet arthropathy. There is increased vascularity and granulation tissue at the region of posterior primary ramus supplying the facet and sinuvertebral and basivertebral nerve supplying the disc and end plates.
Capsular and ligamentous reconfiguration due to segmental instability
As disc degenerates, disc height collapses and the normal tension in spinal segment ligamentous structures and facet stress pattern changes. Capsular and ligamentous laxity occurs as complex spatial patterns of cellular responses to external forces changes due to segmental instability secondary to loss of disc height, leading to subsequent facet abnormal subluxation during physiological range of motion of spinal segment [109]. Anomalous fiber realignment and collagen kinematics changes occurs with loss of structural integrity of the spinal segment. This abnormal realignment during loading of diseased tissue explains the development of laxity of capsular tissue in facet, collagen fiber disorientation as a response to abnormal movement of spinal segment [79]. Facet joint is supplied by posterior primary ramus, medial branch. Abnormal stretching of facet can lead to stretching of medial branch of posterior primary ramus which is enclosed in fibro-osseous canal bounded by accessory process, the mammillary process and mammilloaccessory ligament and subsequently exits through the intermammillary fascicle and mamillostyloid fascicle of multifidus muscle [21,91]. Capsular stretching leads to pain induced during spinal movement (Figs. 1 and 2).
Sympathetic dysfunction
Sinuvertebral nerve and basiverterbral nerve has large contributions from sympathetic nervous system. El-Badawy and El Mikkawy [26] demonstrated that in patients who suffered from chronic lower back pain and failed back surgery syndrome, there was sympathetic dysfunction in the electrophysiological study. Yeater et al. [105] have similar findings with autonomic dysregulation with blunted sympathetic reactivity from measured skin conductance level in patients in chronic back pain compared to normal control. They further concluded that chronic pain may negatively impact typical autonomic responses needed for walking performance and there was potential impact on the brain [105]. As sympathetic responses are hard to be detected clinically, more studies are required to evaluate the clinical significance in sympathetic responses in prediction and treatment of chronic back pain syndrome.
TREATMENT OF CHRONIC BACK PAIN SECONDARY TO SINUVERTEBRAL AND BASIVERTERBAL NEUROPATHY
Discogenic back pain typically presents mechanical lower back pain aggravated on flexion. This is due to increased compressive stress on intervertebral disc during flexion. Classically, the referred pain from the disc radiates to gluteal region without radiation below the level of the knees. However, Kim et al. [48] found that radicular pain in degenerative disc disease might occur without radiological evidence of significant compression. MRI of lumbar spine may showed various grade of degeneration of lumbar intervertebral disc, presence of hyperintenisty zone suggestive of annular tear and MC [66,76,108]. There is high incidence of MRI imaging for lumbosacral spine due to back pain. Interpretation of abnormal MRI finding with back pain should be practice with prudence, careful clinical assessment is important [41]. Rule out other causes of back pain such as facet arthropathy, prolapsed intervertebral disc, spondylolisthesis and spinal instability, Bertolotti syndrome, superior and middle cluneal nerve entrapment syndrome [37,104]. The gold standard test for discogenic pain is provocative discogram. During provocative discogram, a contrast is injected into the disc and clinical assessment of the patient’s pain response to the contrast is recorded. If the pattern of pain is close to the pattern of patient’s symptom, a positive discogram is recorded. A detailed well executed discogram is more specific than MRI findings. Discogram confirmed degenerative disc disease treatment options varies from injection of anesthetic (4% xylocaine or 0.75%) bupivacaine mixed with contrast during discogram to relieve pain and provide a short to medium term therapeutic relief of chronic back pain [85]. Other commercially available electrothermal based intervention are intradiscal electrothermal annuloplasty, disc-FX [55] and transforaminal epidurosopic laser ablation of sinuvertebral nerve, transpedicular intraosseous probe insertion (Fig. 3A) [29,108] and epiduroscopic BVN laser ablation with good clinical outcomes [7,45]. Kim et al. [43] treated BVN with epiduroscopic BVN laser ablation (TEBLA) to ablate BVN. Fischgrund et al. [29] performed intraosseous BVN ablation and found to have sustained benefits at 2 years.

Two radiofrequency ablation techniques for basivertebral neuropathy currently in practice. A : Transpedicular approach. B : Peripedicular approach.
Endoscopic radiofrequency ablation
Kim et al. [48] described the treatment of discogenic back pain with endoscopic radiofrequency ablation of sinuvertebral and BVN. They were selective in the inclusion criteria with patients who presented with lower back pain and radicular leg pain with MRI which demonstrated degenerative disc changes classified by Pfirrmann classification [97] and significant MC of the adjacent vertebral body [65]. They subsequently performed a provocative discogram to affirm the diagnosis of discogenic back pain and offered a trial of conservative treatment with physiotherapy [17,92], injection. In selected patients who failed conservative treatment, endoscopic radiofrequency ablation with either transforaminal endoscopic approach or interlaminar approach to direct radiofrequency ablation probe on sinuverterbral nerve and basiverterbral nerve. They achieved good clinical outcomes in their series [48]. They also introduced a neovascularization grading system, with grade 1 (no vascular changes), grade 2 (presence of neovascularization) and grade 3 (presence of neovascularization and adhesions to neural elements) were found in their patients endoscopic view. They found patients who had discogenic back pain tend to have at least grade 2 neovascularization or grade 3 neovascularization and adhesion (Fig. 4).
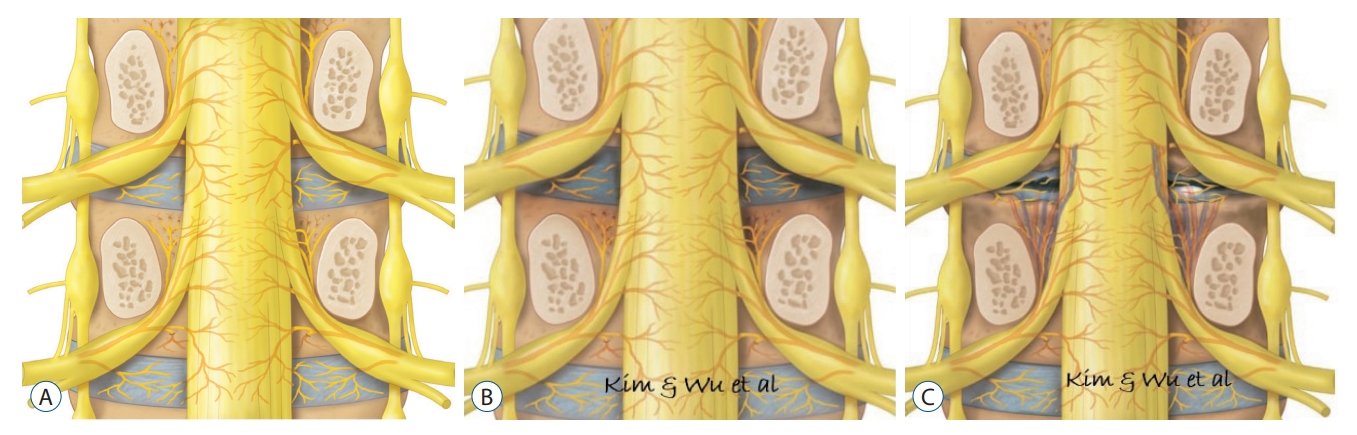
A : Mid coronal picture of normal patient which demonstrates lumbar spine with posterior spinous process, lamina, ligaments and half pedicle removed to demonstrate the distribution of sinuvertebral and basivertebral nerve. B : In corresponding mid coronal picture of patient who had sinuvertebral and basivertebral nerve neurotization. Red shaded area demonstrates the region of neurotization with peridiscal region being sinuvertebral nerve and intraosseous nerve branches being basivertebral nerve. C : In corresponding mid coronal picture of patient who had degenerative disc disease and lower back pain demonstrates corresponding neovascularization around region of sinuvertebral and basivertebral nerve. Modified from Kim et al. [48] with permission.
Endoscopic radiofrequency ablation surgical technique
The principle of endoscopic radiofrequency ablation are firstly to decompress any bulging degenerative disc [40], secondly thermal shrinkage of disc protrusion by radiofrequency coagulator and thirdly, direct application of radiofrequency ablation in the region of sinuvertebral and BVN [29]. There are two target areas for BVN : 1) the transpedicular approach is direct application of heat energy through the pedicle. This often involve using a trochar cannula under fluoroscopic guidance to position inside the pedicle to introduce radiofrequency ablator into the region of basiveretberal nerve (Fig. 3A); and 2) the parapedicular approach which the heat energy is applied to the dorsal surface of vertebral body and around the medial and superior aspect of pedicle where there is dense supply of sinuvertebral nerves before they branch into BVN (Fig. 3B). The radiofrequency ablator can be introduced endoscopically through either interlaminar or transforaminal route for the parapedicular approach.
Interlaminar endoscopic lumbar approach for radiofrequency ablation [46,47,84,102]
Patient underwent epidural or general anesthesia, in prone position on Wilson frame over a radiolucent table. Endoscope is docked on the junction of laminofacet line confirmed on intraoperative image intensifier. Interlaminar endoscope is introduced under fluoroscopic guidance after serial dilation. Soft tissue is dissected to expose ligamentum flavum. Splitting or cutting of ligamentum flavum using a probe and endoscopic Kerrison rongeur is performed and working channel is introduced into the spinal canal with neural elements protected out of harm’s way by working retractor tube. Disc was inspected for any loose fragment or annular tear which would be removed and annuloplasty is performed on annular tear. If there is a concurrent thickening of ligamentum f lavum, sometimes stenosis endoscope is used to performed decompression of ligamentum flavum prior to application of radiofrequency ablation [49,58]. If there is no spinal stenosis, there is no difference in outcomes in ligamentum flavum removal or splitting technique in the interlaminar approach [56].
Transforaminal endoscopic lumbar approach for radiofrequency ablation [42]
Patient underwent local anesthesia with moderate sedation, in prone position on Wilson frame over a radiolucent table. Skin marking was made 8–12 cm away from midline in the same principle approach as transforaminal approach. Docking is performed on the Kambin’s triangle near the intervertebral disc the triangle consisted of hypotenuse as exiting nerve root, height as traversing nerve root and base as superior border of the inferior vertebra [107]. Transforaminal endoscope is introduced through serial dilation [54,106]. A mobile outside in technique with endoscopic drilling of ventral superior articular facet was performed to gain access to the intervertebral disc space [42]. Parts of disc were typically removed to accommodate the introduction of transforaminal endoscope to sinuvertebral nerve and BVN.
Ablation of neuropathic BVN and sinuvertebral nerve [45]
In both endoscopic approaches, after dealing with discogenic bulge or discectomy performed, exposure of sinuvertebral nerve region was performed. Radiofrequency ablation probe is used in ablation of neuropathic BVN around the suprapedicular area and sinuvertebral nerve in mid disc region between posterior annulus and PLL. The working retractor was in place to protect the neural elements. There is often a finding of buttock twitching when radiofrequency ablation was applied to the area of pathological neurotization of basivertebral and sinuvertebral nerves. The BVN is not directly visualized but radiofrequency energy is applied to suprapedicular region to pass on the energy through the nutrient foramen to BVN. While sinuvertebral nerve is treated by applying energy caudal to mid disc region of the intervertebral disc in the space between the posterior annulus of the disk and the PLL, again, either buttock of the patient may twitch accordingly and once sinuvertebral nerve is ablated, the twitching would stop (Fig. 4).
CONCLUSION
The understanding of sinuvertebral and BVN in contribution of lower back pain is developing. Literature supports the pathological neurotization of sinuvertebral and BVN is strongly associated with chronic lower back pain. A targeted approach by fluoroscopic and endoscopic guidance to sinuvertebral and BVN can improve chronic lower back pain.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Informed consent
This type of study does not require informed consent.
Author contributions
Conceptualization : HSK, PHW, ITJ; Data curation : HSK, PHW; Formal analysis : HSK, PHW; Funding acquisition : ITJ; Methodology : HSK, PHW; Project administration : HSK, PHW; Visualization : HSK, PHW; Writing - original draft : HSK, PHW; Writing - review & editing : HSK, PHW
Data sharing
None
Preprint
None
Acknowledgements
Mr. Keong Rae Kim and Seong Hee Park for coordination of scientific research.
