Endovascular Treatment of Dural Arteriovenous Fistulas: Single Center Experience
Article information
Abstract
Objective
Treatment of intracranial dural arteriovenous fistulas (dAVFs) remains a challenge. However, after introduction of Onyx, transarterial approach is the preferred treatment option in many centers. We report our experience of dAVFs embolization with special emphasis on transarterial approach.
Methods
Seventeen embolization procedures were performed in 13 patients with dAVFs between Jan 2009 and Oct 2014. Clinical symptoms, location and type of fistulas, embolization methods, complications, radiological and clinical outcomes were evaluated using charts and PACS images.
Results
All 13 patients had symptomatic lesions. The locations of fistulas were transverse-sigmoid sinus in 6, middle fossa dura in 4, cavernous sinus in 2, and superior sagittal sinus in 1 patient. Cognard types were as follows : I in 4, IIa in 2, IIa+IIb in 5, and IV in 2. Embolization procedures were performed ≥2 times in 3 patients. Nine patients were treated with transarterial Onyx embolization alone. One of these required direct surgical puncture of middle meningeal artery. Complete obliteration of fistulas was achieved in 11/13 (85%) patients. There were no complications except for 1 case of Onyx migration in cavernous dAVF. Modified Rankin scale score at post-operative 3 months were 0 in 11, and 3 in 2 patients.
Conclusion
Transarterial Onyx embolization can be a first line therapeutic option in patients with dAVFs. However, transvenous approach should be tried first in cavernous sinus dAVF because of the risk of intracranial migration of liquid embolic materials. Furthermore, combined surgical endovascular approach can be considered as a useful option in inaccessible route.
INTRODUCTION
Dural arteriovenous fistulas (dAVFs) are acquired arteriovenous shunts confined to the dura and are supplied by branches of the extracranial carotid artery, tentorial branches of the internal carotid artery, meningeal branches of the vertebral artery, and pial branches of cerebral arteries4). Persistence of cortical venous reflux in intracranial dAVFs has a high annual risk of hemorrhage and nonhemorrhagic neurologic deficits. Cognard et al.4) noted intracranial hemorrhage in 40% of patients with type III, and in 65% with type IV dAVFs. Rebleeding rates may be as high as 35% during the first 2 weeks after initial hemorrhage. As neuroendovascular technique has developed considerably, open surgery for dAVFs has become a secondary treatment option. Transvenous coil embolization and transarterial n-butyl-2-cyanoacrylate (n-BCA) injection were strong treatment methods of dAVFs. Even though transvenous access was not always possible and transarterial nBCA injection frequently resulted in partial embolization of feeding arteries. Recently, Onyx (Covidien, Irvine, CA, USA) has become the safe and feasible embolic material with higher obliteration rates than n-BCA7). Some dAVFs have an inaccessible lesion with only 1 route, so the combination of transarterial and transvenous embolization results in higher obliteration rates. Even if endovascular embolization has developed remarkably, surgery or radiosurgery are still required in certain patients for complex lesion, failure of both transvenous and transarterial embolization, or palliation9).
In this study, we reviewed our experience with a consecutive series of 13 patients subjected to the multimodal endovascular approach for intracranial dAVFs treatment. On the basis of our initial experience with multimodal management of complex dAVFs, we proposed our current treatment algorism and detailed consideration of the endovascular, combined surgical or surgical treatment options for dAVFs in the current Onyx era.
MATERIALS AND METHODS
This retrospective study was approved by institutional review board (IRB) at our center. All symptomatic intracranial dAVFs were diagnosed and treated by the neurovascular team. In our institution, endovascular intervention was selected as a primary treatment options in all patients except for anterior cranial fossa dAVF, which was treated surgically. After the introduction of Onyx and detachable microcatheter, transarterial embolization was preferred in most dAVF, since dAVF could be successfully obliterated by the arterial injection for a long time.
We determined which patients were candidates for embolization. If dAVFs was not amendable to endovascular treatment because of a lack of appropriate arterial or transvenous access, the patient was treated by combined surgical endovascular embolization. Type I fistulas (4 patients) were treated only if the patient had intractable symptoms that did not respond to conservative treatment.
A review of the records of cerebrovascular center at our hospital identified 13 patients with dAVFs treated by endovascular embolization (transarterial, transvenous embolization, or both) or combined surgery between December 2009 and May 2014. The clinical and angiographic features were retrospectively reviewed from prospectively collected endovascular records. Data collected included age, sex, presenting symptoms, location, type of fistula by Cognard et al.4), feeders, approaches, embolization materials, onyx amount, injected artery, angiographic result and prognosis (Table 1).
Endovascular procedures
All endovascular procedures were performed under general anesthesia and monoplane (before 2013 June) or biplane angiographic suite with 3-dimensional rotational angiographic capability (Philips Medical Systems, Best, The Netherlands). After femoral arterial access, diagnostic angiography was performed on both common carotid artery (CCA), internal carotid artery (ICA), external carotid artery (ECA) and both vertebral artery (VA). A 6 Fr guiding catheter was placed to the ECA for transarterial approach and to the internal jugular vein for transvenous approach. Heparin (3000 units) was injected intravenously after guiding catheter placement.
Transarterial approach
After femoral sheath insertion, the patients were heparinized with an average 3000 unit initially and 1000 unit per hour intravenously, to maintain an activated coagulation time of between 250 and 300 seconds. A 6 Fr guiding catheter was introduced and advanced to the ECA. An Onyx compatible microcatheter (Apollo, Marathon, or Echelon-10) was navigated through the guiding catheter into the feeding artery as close as possible to the fistula point, allowing for an adequate distance for reflux of embolic agent. If dAVFs had multiple feeders, mostly the MMA feeder was chosen to target artery to inject Onyx to the fistula. The endpoint of embolization was angiographic obliteration of the fistula. When the fistula was very complex or the reflux set in earlier than expected, more than 1 session of embolization through another feeders were performed. When some extracranial feeding artery had tortuous and long pathway, embolization was successfully performed by the combined surgical transarterial approach.
Transvenous approach
The transvenous approach was selected as a primary treatment modality before the introduction of Onyx for the treatment of dAVF. However, this approach was still used as a primary option for indirect CCF because of dangerous anastomotic channel between dural branches of ECA and ICA.
After diagnostic angiography, the femoral vein was punctured and using the roadmap obtained from an intra-arterial injection, a 6 Fr guiding catheter was introduced and advanced to the internal jugular vein. Through this guiding catheter, the microcatheter was advanced to the target lesion. When some sinus pathway was occluded or had severe stenosis, transvenous embolization with coil was successfully performed by the combined surgical transvenous approach.
Combined surgical and endovascular approach
In case of the inaccessible endovascular route, endovascular embolization was performed after surgical exposure of target artery or venous sinus under general anesthesia. Direct puncture of the target vessel was done under the roadmap obtained through the intra-arterial injection. Subsequently, transarterial Onyx injection or transvenous coil embolization was done in the same manner described above.
Demonstrative cases
Transarterial embolization
A 56-year-old man presented with semicomatose consciousness. Brain computed tomography (CT) showed intracerebral hemorrhage and subdural hematoma with midline shifting. Cerebral angiography demonstrated dAVF involving the transverse sigmoid sinus (TSS) with multiple feeders from middle meningeal artery (MMA) and occipital artery (OA). DAVF was completely obliterated with 4.5 cc of Onyx through the petrosal branch of MMA in a single session followed by surgical evacuation of hematomas. He was discharged home at 2 months with mild disability (Fig. 1).

Cerebral angiograms demonstrating complete obliteration of dural arteriovenous fistula (dAVF) using transarterial Onyx embolization in a 56-year-old man. Lateral view of right external carotid artery (ECA) angiograms show a transverse sigmoid sinus dAVF, supplied by multiple feeders from middle meningeal artery (MMA) and occipital artery on early arterial phase (A), and drained retrogradely into an engorged cortical vein on late arterial phase (B). Postoperative lateral view of right ECA angiogram after transarterial injection of 4.5 cc Onyx via petrosal branch of MMA demonstrated complete obliteration of the fistula in single session (C). Postoperative lateral skull radiograph shows the Onyx cast (D).
Combined surgical and transarterial approach
A 66-year-old woman presented with intermittent paraparesis and generalized tonic-clonic seizure. Cerebral angiography demonstrated dAVF involving SSS, which was associated with SSS occlusion on the posterior one third. The dAVF was fed by bilateral MMAs, superficial temporal arteries (STAs) and OAs with marked retrograde cortical venous reflux. Transfemoral arterial Onyx embolization was performed through right MMA and STA, but it was insufficient resulting in partial obliteration of dural AVF because of tortuous MMA preventing the microcatheter from reaching the fistula closely enough. Second procedure was performed through left MMA accessed by direct MMA puncture following small decortications of cranium overlying the MMA using a diamond drill 1 week later. Microcatheter could be located far distally to the fistula through 4 Fr sheath placed into the MMA and complete obliteration of dAVF was achieved using 3.9 cc of Onyx. Postoperatively, she recovered well and her paraparesis returned to normal (Fig. 2).

Transcranial transarterial Onyx embolization of superior sagittal sinus (SSS) dural arteriovenous fistula (dAVF) in a 66-year-old woman. Right external carotid artery (ECA) angiography showed dAVF on superior sagittal sinus (SSS) fed by both middle meningeal arteries (MMAs), superficial temporal arteries (STAs) and occipital arteries (OAs) and drained into the SSS which was occluded in the posterior one third. Marked retrograde bilateral superficial cortical venous reflux was also demonstrated (A and B). Final ECA lateral angiograms of transarterial Onyx embolization through MMA and STA still showed the partial obliteration of dAVF after first session (C). After one week, on second session, roadmap image shows the drilling point of MMA for transcranial transMMA approach (D). Photograph shows the placement of 4 Fr sheath in the MMA and fixation with black silk tie to prevent accidental removal during the procedures (E). Microcatheter angiogram shows the dAVFs clearly (F). Postoperative ECA anterioposterior angiograms showing the complete obliteration of dAVFs without cortical venous reflux (G). Postoperative skull anterioposterior and lateral radiographs shows the Onyx cast after complete obliteration of dAVFs (H and I).
Combined surgical and transvenous approach
A 72-year-old woman presented with tinnitis, intermittent aphasia and generalized tonic-clonic seizure. Brain magnetic resonance image (MRI) showed the abnormal signal void lesions on left temporal and occipital lobe. Cerebral angiography demonstrated dAVF involving left TSS, which were fed by MMA, meningohypophyseal artery, and OA. We tried to introduce the microcatheter to dAVF through controlateral TS or ipsilateral jugular vein, but we could not access the fistula point because she had isolated left TS. In the first session, dAVFs were partially treated by transarterial n-BCA injection through MMA and OA. On second session, the left TSS was exposed through a minimal craniectomy. After exposure of the left TSS, 4 Fr sheath was placed to the TS directly using a micropuncture needle. Then, Prowler select plus microcatheter was advanced into the sheath placing the tip into the isolated TS. Sixteen coils were deployed into the isolated sinus under the roadmap guidance. Post-embolization angiography demonstrated total occlusion of DAVF. Postoperatively, the patient showed improvement in speech and tinnitis (Fig. 3).
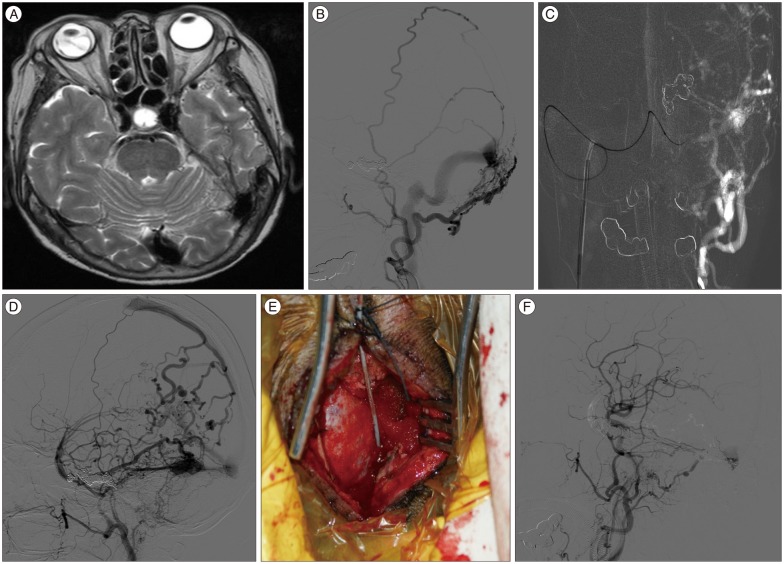
A case of transvers sigmoid sinus (TSS) dural arteriovenous fistula (dAVF) showing the usefulness of direct sinus exposure. A 72-year-old woman with left TSS dAVF had intractable tinnitus. Brain T2 weighted magnetic resonance image shows the marked low signal intensity on temporo-occipital lobe nearby TSS (A). Left external carotid artery (ECA) lateral angiography shows a left TSS dAVF, supplied by multiple feeders from the ECAs, and draining into the TSS (B). Roadmap anterioposterior image shows that failed transvenous approach because of ipsilateral sinus occlusion and severe stenosis near torcular (C). Although transarterial n-butyle-2-cyanoacrylate embolization was performed through the middle meningeal artery and occipital artery, lateral ECA angiogram shows the partial obliteration on first session (D). Intraoperative photography shows the direct puncture on TSS (E). In the second session, remnant dAVF had successful complete obliteration with transvenous coil embolization through surgically opened and direct punctured on the sinus. And final lateral common carotid angiogram shows the markable obliteration, but remained the a little flow from meningohypophyseal artery (F).
Complication case
A 49-year-old woman presented with exophthalmos and conjunctival injection. Cerebral angiography demonstrated the indirect CCF, which was mainly fed by the accessory meningeal artery and drained into engorged superior ophthalmic vein as a retrograde fashion. Even though manual carotid compression was performed for two months, her symptoms did not improve.
Transvenous embolization was tried first through inferior petrosal sinus, but failed. Thus, transarterial Onyx embolization was performed. After placement of microcatheter into the accessory meningeal artery, Onyx injection was started carefully. During Onyx injection, sudden migration of Onyx cast into the cerebral artery was detected. Despite several efforts to retrieve the Onyx cast using endovascular technique, Onyx cast was not retrieved. Thus, emergent microsurgical removal of Onyx cast from the MCA bifurcation was performed with one piece successfully. Follow-up magnetic resonance angiography showed complete restoration of MCA flow (Fig. 4).

A complication case showing the risk of Onyx migration in a 49-year-old woman with indirect carotid cavernous fistula. Left internal and external carotid artery angiography shows indirect carotid cavernous fistula, supplied by a feeder from the accessary meningeal artery, and draining into the cavernous sinus (CS) (A and B). Intra-procedural angiogram and skull radiographs shows the migrated Onyx casts (arrows) on intracerebral artery during 0.4 cc Onyx injection (C). Pre and post microsurgical findings of onyx cast removal on middle cerebral artery and photography of removed Onyx cast (D and E). Well recanalized intracerebral artery flow on magnetic resonance angiography (F).
RESULTS
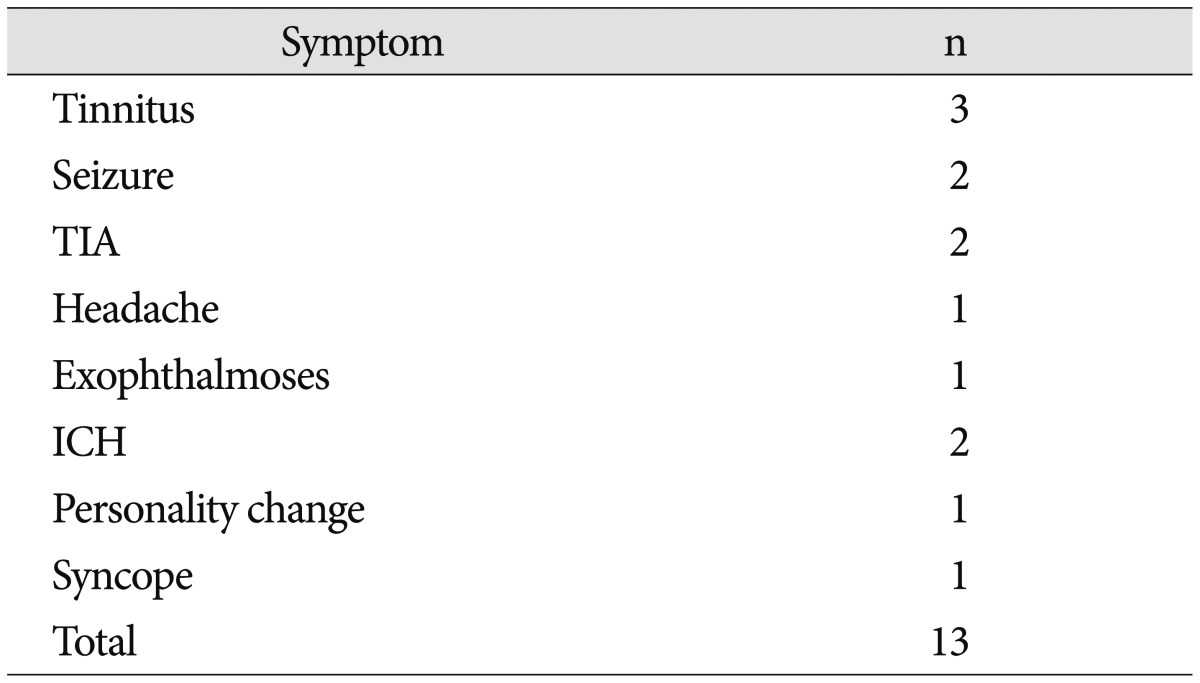
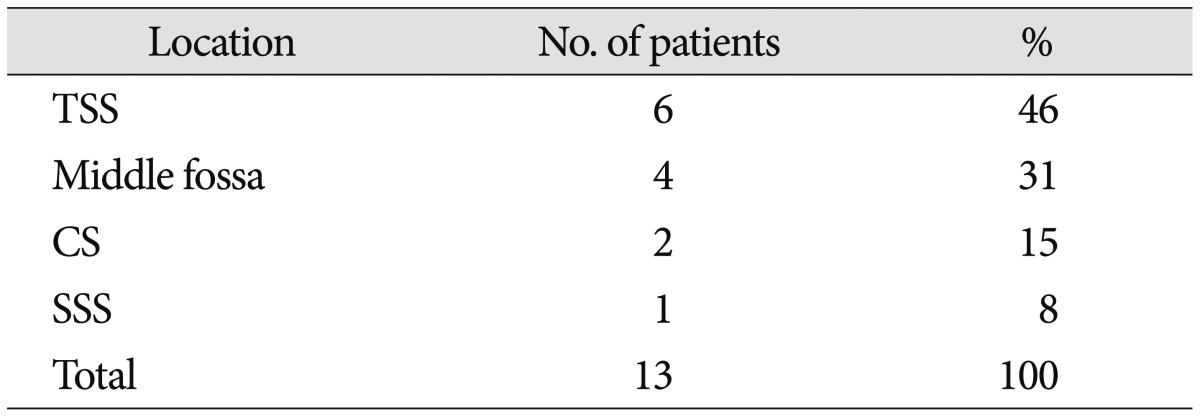
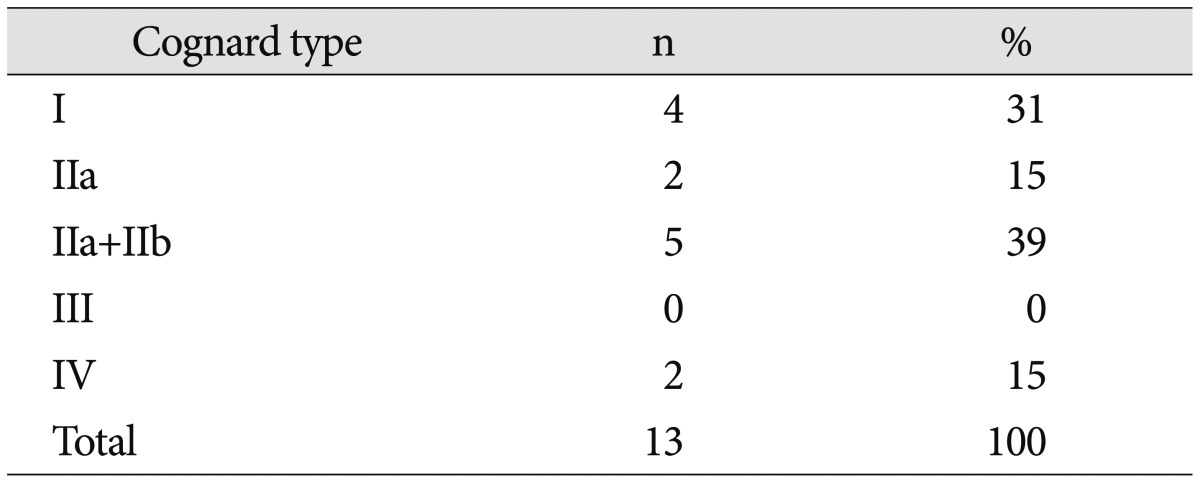
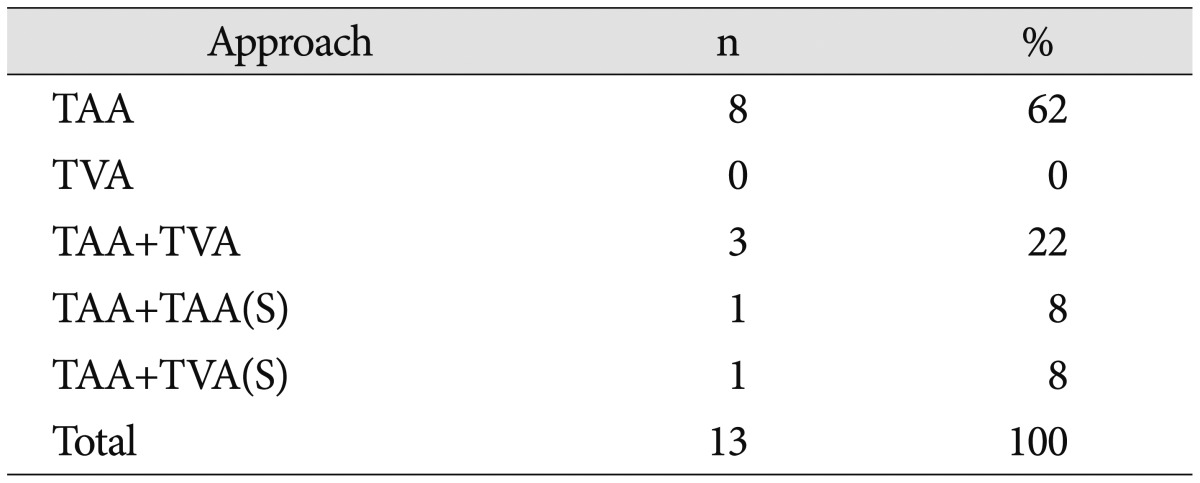
The average age at presentation was 72 years (range, 28–78 years). Six patients were men (46%) and 7 were women (54%). All 13 patients had symptomatic lesions. Pulsatile tinnitus was most common followed by seizure, and transient ischemic attack. Other symptoms were headache, intracerebral hemorrhage, exophthalmos, personality change, and syncope (Table 2). The locations of fistulas were TSS in 6 (48%), middle fossa dura in 4 (31%), CS in 2 (15%), and SSS in 1 (8%) patient (Table 3). Cognard types were as follows : I in 4 (31%), IIa in 2 (15%), IIa+IIb in 5 (39%), and IV in 2 (15%) (Table 4). Embolization procedures were performed more than 2 times in 3 patients. Transvenous approach was tried in 4 patients with or without the transarterial approach (1 surgical sinus puncture, 2 transvenous followed by transarterial, 1 transarterial followed by transvenous). Nine (62%) patients were treated with transarterial Onyx embolization alone (Table 5). One of these required direct surgical exposure and puncture of MMA. Complete obliteration of fistulas was achieved in 11/13 (85%) patients after multimodal treatment. Onyx migration into cerebral artery was observed in 1 patient with indirect CCF, who was treated with transarterial Onyx injection after failed transvenous approach (Fig 4). Open surgical removal of migrated Onyx cast after unsuccessful endovascular retrieval resulted in a good clinical outcome. There were no other complications, such as cranial nerve palsy or cerebral infarction. Modified Rankin score (mRS) was acquired at post-operative 3 months. Eleven patients had mRS 0, 2 patients had mRS 3 (1 patient was admitted on Hunt and Hess grade V with subarachnoid hemorrhage, and the other patient had Parkinson disease).
DISCUSSION
The pathogenesis of dAVFs is controversial. There are two known pathogenic mechanisms based on sinus thrombosis. The first is that arteriovenous shunts between meningeal arteries and dural venous sinuses enlarge in response to elevated local venous pressure, resulting in a pathologic shunt3812). The second is that venous hypertension due to outflow obstruction causes decreased cerebral perfusion and promotes neoangiogenesis310). Predisposing risk factors for venous thrombosis such as antithrombin, protein C and S deficiencies, and trauma are associated with dAVFs development56). In pediatrics, the result of birth trauma, infection, in utero venous thrombosis, or maternal hormones are regarded as the etiology of dAVFs. In our series, sinus occlusion was observed in 2 patients who were treated by the combined surgical approach. Another 2 patients had trauma history. While the dAVFs are more commonly diagnosed in perimenopausal women with underlying hormonal influence, the ratio of male to female was similar and mean age was 58 years old in our series.
The incidence of DAVFs by location is as follows : TS, 50%; CS, 16%; tentorium, 12%; SSS, 8%; and anterior fossa, 2%19). The symptoms could arise from these locations. Borden and Cognard classification systems associate cortical venous reflux with high risk of intracranial hemorrhage and nonhemorrhagic neurologic deficits24). In our series, the most common initial symptom was intractable tinnitus, location was TS sinuses, and they were mostly Cognard I and IIa+IIb.
Management of dAVF is controversial. DAVF is a spectrum of disease that has different severity and various locations. Traditionally anterior fossa dAVF has been treated with surgical disconnection of AVF. However, most dAVF can be treated with endovascular technique with various success rates. Transvenous coil embolization of fistula has been considered gold standard for the treatment of dAVF. Transarterial feeder embolization with nBCA usually resulted in partial embolization because it is very difficult to penetrate multiple feeders with nBCA completely. However, after introduction of Onyx in the treatment of dAVF, single feeder injection could result in complete obliteration of fistula because of good penetration capability of Onyx. Onyx can penetrate the single feeder and fistula and then retrograde obliteration of multiple feeders from different arteries. Slow steady injection using reflux hold reinjection technique is very important to penetrate multiple feeders and fistulas completely from single feeder injection. Even though transarterial approach is preferred option in post-Onyx era, transvenous approach is still primary option in dAVF on the specific location such as cavernous sinus or anterior condylar confluence because there are so many dangerous anastomoses between ECA and ICA. In our complication case, Onyx cast migrated from ECA to ICA through dangerous collaterals. If we tried transarterial approach in this specific location, we'd better to occlude the cavernous ICA with balloon temporarily during transarterial Onyx injection to prevent Onyx migration to cavernous ICA through dangerous anastomosis between accessory meningeal artery and inferolateral trunk of cavernous ICA.
In the technical point of view, location of microcatheter tip is also important to achieve complete obliteration of dAVF with single feeder injection. The tip of microcatheter is placed as close as possible to fistula point. The disadvantage of Onyx injection was long injection time and subsequent radiation exposure. To reduce the injection time, balloon microcatheter can be very useful. When we use balloon microcatheter, we don't need to make Onyx plug around the microcatheter tip because Onyx injection under balloon inflation in the feeder makes onyx go forward instead of going backward. Onyx could not reflux proximally beyond the balloon. Therefore, faster injection of Onyx is possible without the risk of microcatheter gluing.
A review of literature on multimodal treatment results of dAVFs indicated that they were different before and after Onyx1415). Mean obliteration rate of dAVFs was 70% (37.5–75%) in the pre-Onyx Era, and 81% in the post-Onyx Era13). In our series, complete obliteration rate was 85% in overall, and 80% in high grade (III and IV) dAVFs. The reason of high complete obliteration rate at our center was that endovascular embolization with combined surgical approach could overcome the inaccessible route of transarterial or transvenous approach. In our center, 8 patients were successfully treated by the transarterial approach alone and 2 patients by the combined surgical approach. All patients were successfully treated.
MMA was used as a main access route of transarterial Onyx embolization because the MMA was anchored on the dura, and superselection of MMA with microcatheter was not difficult in most of the cases. In addition, MMA diameter was usually smaller than other more dilated feeders such as OA.
Literature review indicated that the common complication during endovascular Onyx embolization was cranial nerve palsy, and sometimes trigeminocardiac reflex. The petrous branch of MMA is often the main supply for dAVFs in the petrotentorial region. It also supplies the cranial nerve at the middle cranial fossa, and permanent cranial nerve palsy can occur. Therefore, we always tried to locate the microcatheter tip into petrous MMA far distally to avoid complications11). There was no complication of cranial nerve palsy.
Onyx migration into cerebral circulation may cause disturbed cerebral blood flow and subsequent cerebral infarction, as well as partial obliteration of dAVF. In our complication case of indirect CCF, Onyx migration occurred from accessary meningeal artery to internal carotid artery beyond the fistula through probably, infero-lateral trunk. In this situation endovascular retrieval using microsnare, or retrieval stent should be tried first. Unfortunately, if this retrieval procedure was not successful, prompt surgical retrieval of Onyx cast may result in favorable outcome in a selected patient. Recently, balloon assistance has been used to prevent Onyx migration to the cerebral arterial system16). However, the neurosurgeon should consider the risk of Onyx migration when it was injected transarterially in patient with indirect CCF, and that the primary treatment route of indirect CCF is the transvenous route.
CONCLUSION
Transarterial Onyx embolization is a potential first line therapeutic option in patient with dAVFs. However, the transvenous approach should be tried first in cavernous sinus dAVF because of the risk of intracranial migration of liquid embolic materials. Furthermore, combined surgical endovascular approach can be considered as a useful option in case of inaccessible endovascular route.
Acknowledgements
This research was supported by the Soonchunhyang University Research Fund.