Posterior Atalntoaxial Fusion with C1 Lateral Mass Screw and C2 Pedicle Screw Supplemented with Miniplate Fixation for Interlaminar Fusion : A Preliminary Report
Article information
Abstract
Objective
To investigate the feasibility of C1 lateral mass screw and C2 pedicle screw with polyaxial screw and rod system supplemented with miniplate for interlaminar fusion to treat various atlantoaxial instabilities.
Methods
After posterior atlantoaxial fixation with lateral mass screw in the atlas and pedicle screw in the axis, we used 2 miniplates to fixate interlaminar iliac bone graft instead of sublaminar wiring. We performed this procedure in thirteen patients who had atlantoaxial instabilities and retrospectively evaluated the bone fusion rate and complications.
Results
By using this method, we have achieved excellent bone fusion comparing with the result of other methods without any complications related to this procedure.
Conclusion
C1 lateral mass screw and C2 pedicle screw with polyaxial screw and rod system supplemented with miniplate for interlaminar fusion may be an efficient alternative method to treat various atlantoaxial instabilities.
INTRODUCTION
Atlantoaxial instability can be caused by various reasons like trauma, malignancy, congenital malformation, or inflammatory diseases and it is usually treated by reduction and stabilization of the C1-C2 joint. Since the first description of the sublaminar wiring technique by Gallie in 19399), various modification of the techniques had been suggest by Brooks, Sonntag, Magerl and Harms3,6,11,17,23,31). Although these techniques had been developed and modified to achieve the better result of stabilization of atlantoaxial complex, the operations are still challenging due to devastating complications or technical difficulties. Based on individual screw placement in C1 and C2 suggested by Harms and Melcher17), we have added our new technique to reinforce stabilization and accomplish successful bone fusion. With an expectation to acquire better outcome, less complication, and technical facility, we have performed this technique to thirteen patients over the past 4 years. In this study, we present our technique for posterior C1-C2 fusion by using miniplate for interlaminar fusion which supplements C1 lateral mass and C2 pedicle screw fixation. In addition, a retrospective review of thirteen patients treated by this technique is also presented.
MATERIALS AND METHODS
Patient demographics and bone fusion evaluation
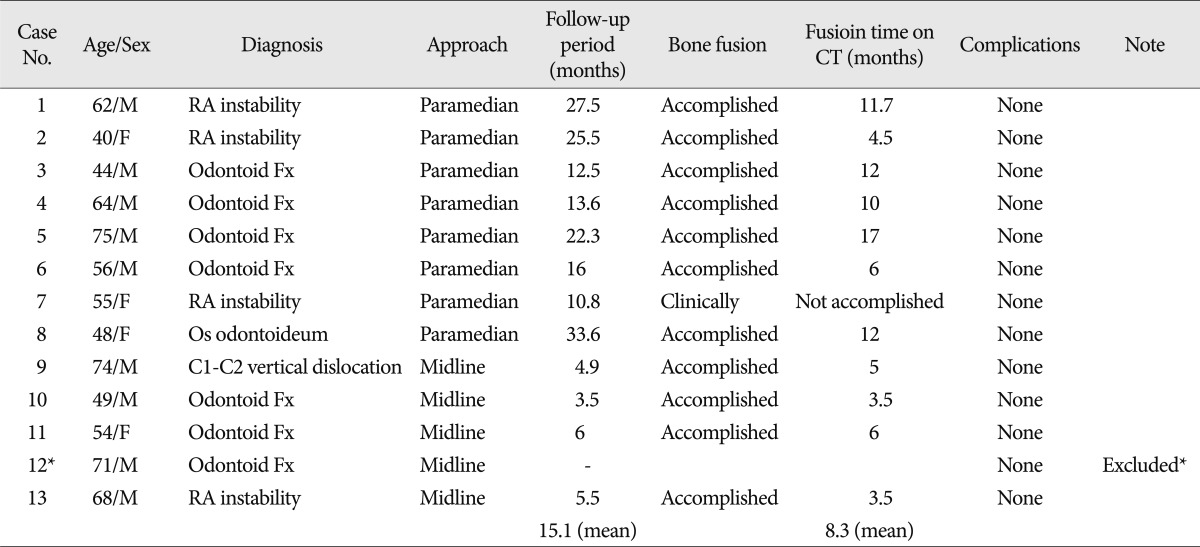
Thirteen patients underwent the procedure from March 2006 to October 2010 (Table 1). Nine patients were male, and four patients were female. The average age was 58.5 years (range 40-75 years). Seven of these patients had odontoid process fracture with transverse ligament injury, four had rheumatoid arthritis and one had os odontoideum. One patient had C1-2 vertical dislocation injury after traffic accident. Mean follow-up period was 15.1 months. Eight patients were approached with paramedian incision for the procedure and five patients including C1-2 vertical dislocation injury was approached with classical midline incision. After the operation, all patients underwent computed tomography or plain X-ray with dynamic image during the follow-up except one with odontoid process fracture. Three criteria were evaluated with these images : 1) Presence of bridging bone in computed tomography; 2) Absence of lucency around implant; 3) Less than 2 degrees of segmental motion and less than 2 mm change of interspinous distance of atlantoaxial spine on its dynamic view.
Surgical technique
Under general anesthesia, the patient was placed in the prone position and the neck was held in alignment with Mayfield. The position of the C1-C2 complex was verified by use of fluoroscopy. Classical midline incision or bilateral paramedian incision was used for the operation. Bilateral paramedian incision was made 1.5-2 cm off to midline and muscle was dissected with the use of Metrx Quadrant system (Medtronics®) (Fig. 1). The cervical spine was exposed subperiosteally from the C1 to C3. The atlantoaxial complex was exposed to the lateral border of the C1-C2 articulation. Bleeding typically arose from dissection around the epidural venous plexus along the C1-C2 joint. This was controlled with a bipolar electrocautery, Gelfoam or cotton pledgets. The bleeding was controlled most effectively with a combination of Gelfoam powder and thrombin. The C1-C2 joint was exposed and opened by dissection over the superior surface of the C2 pars interarticularis. The dorsal root ganglion of C2 was retracted in a caudal direction to expose the entry point for the C1 screw, which was in the middle of the junction of the C1 posterior arch and the midpoint of the posterior inferior part of the C1 lateral mass. The entry point was marked with a 2 mm high speed burr drill. Then the pilot hole was drilled in a slightly convergent trajectory in an anterior-posterior direction and parallel to the plane of the C1 posterior arch in the sagittal direction, with the tip of the drill directed toward the anterior arch of C1. The drilling was accomplished with guidance from intraoperative landmarks and the lateral view of fluoroscopy. The hole was tapped and a 4 mm Vertex polyaxial screw (Medtronics®) of an appropriate length was inserted bicortically into the lateral mass of C1. A number 4 Penfield was used to delineate the medial border of the C2 pars interarticularis, and the entry point for placement of a C2 pedicle screw was marked with a high speed burr. The entry point of C2 pedicle screw was in the cranial and medial quadrant of the isthmus surface of C2. The pilot hole was prepared with a 2 mm drill bit, just perforating the opposite cortex. The direction of the bit was approximately 20° to 30° in a convergent and cephalad direction, guided directly by the superior and medial surface of the C2 pedicle. The hole was tapped, and a 4 mm polyaxial screw of the appropriate length was inserted bicortically. If necessary, reduction of the C1 ring was performed by manipulating C1 and C2 using the screws, followed by fixation to the rods to maintain the alignment. Then the posterior arch of C1 and C2 lamina were decorticated and tricortical bone taken from the posterior iliac crest was placed between decorticated surfaces of C1 and C2. Miniplate was molded manually to maximize its contact with surface of bone. 5 to 7 mm length screws were placed on inferior surface of C1 posterior arch, center of tricortical bone and C2 lamina bilaterally (Fig. 2). Intraarticular fusion could be also performed by decorticating the joint surfaces under direct vision. Patients were mobilized on the first postoperative day and wear a soft cervical collar for 2 to 3 weeks.

A : Preoperative plan for paramedian approach. 3-4 cm length incision was made 1.5-2 cm off to midline bilaterally. B : Tubular retractor and Quadrant of METRX system (Medtronics®) was used to dissect paravertebral musculature.
RESULTS
Satisfactory screw placement and reduction were achieved in all patients. No instance of dural injury or vertebral artery injury was observed. There was no case of neurologic deterioration after surgery or at follow-up related to the procedure. One patient who was lost during the follow up was excluded from data analysis. Patients were followed up with radiographs and clinical examinations. Eleven people have satisfied all three bone fusion criteria. One patient failed to achieve bridging bone on her postoperative CT. However, she has satisfied the other two criteria of bone fusion. Therefore, fusion rate of this technique was 91.7% and considered as 100%, clinically. Mean fusion time was 8.3 months. The results are summarized on Table 1.
Case 1
A 40-year-old female was transferred from rheumatology department due to the posterior neck pain for 2 years. She was suffered from rheumatoid arthritis for 10 years. Preoperative cervical X-ray showed instability of atlantoaxial segment (Fig. 3). After taking CT and MRI she was diagnosed to C1-C2 instability due to rheumatoid arthritis. She had posterior C1-C2 fixation with bilateral paramedian incision (Fig. 4). Bilateral paramedian incision was made 1.5-2 cm off to midline and muscle was dissected with the use of Metrx Quadrant system. The bleeding from epidural venous plexus impeded the dissection but it was controlled with a combination of Gelfoam powder and thrombin. After the screw fixation on C1 and C2, autologous bone harvested from her iliac bone was placed between C1-C2 lamina and fixed with miniplate. After 4.5 months we could confirm bone fusion through CT scan (Fig. 5).
Case 2
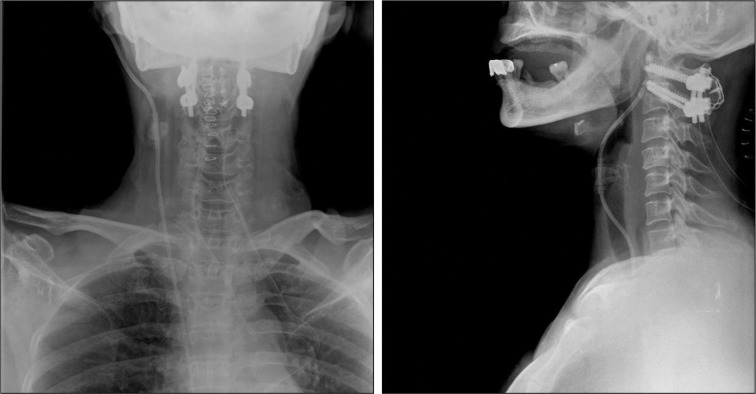
A 54-year-old female was admitted via emergency room with posterior neck pain after traffic accident. She was diagnosed to odontoid process fracture with transverse ligament injury (Fig. 6). She was operated with midline approach (Fig. 7). Paraspinal muscles were dissected subperiosteally from cervical spine carefully trying to save nuchal ligaments. Preoperative X-ray after prone positioning revealed normal alignment of atlantoaxial segment so intraoperative reduction of C1-C2 was unnecessary. After the screw fixation on C1 and C2, autologous bone harvested from her iliac bone was placed between C1-C2 lamina and fixed with miniplate. After the operation, she complained mild posterior neck pain. After medical treatment with analgesics, her condition was improved and she was able to be discharged with soft neck collar.

Preoperative MRI of case 2. White arrow shows type II odontoid process fracture. Bold white arrow shows transverse ligament injury.
DISCUSSION
Traditionally, the atlantoaxial instability had been treated using C1-2 posterior wiring and bone graft. Because of the high mobility of the C1-2 motion segment, fusion rates at this level have been substantially lower than those at the subaxial spine. Therefore, since the first description of the sublaminar wiring technique by Gallie in 19399), various modification of the techniques like wedge compression method and interspinous wiring method had been suggest by Brooks and Sonntag3,6,31).
Although the posterior wiring procedure is easy to accomplish, this technique carries possible risk of dural or neuronal injury during procedure and the halo vest immobilization is required to accomplish successful bone fusion.
Since the transarticular screw fixation had suggested by Magerl and Seemann in 198723), supplemental halo brace became no longer necessary due to immediate rigid multidirectional stability25). Although the transarticular screw fixation provided superior stability and bone fusion rate to wiring or the use of Halifax clamps13,14,16,19,25,27,33), this technique requires meticulous preoperative planning and precise operative techniques are mandatory to achieve successful result and to avoid vertebral artery injury.
In 2001, Harms and Melcher17) described a technique for individual fixation using polyaxial screw and rod system and similar study was published by Goel et al. in 200211). By using C1 lateral mass and C2 pedicle screw with polyaxial screw followed by fixation to the rods to maintain its alignment, intraoperative reduction of the C1 ring became possible if necessary and the guidance of drill became no longer restricted by patient's osseous axial anatomy. Moreover, this procedure has shown to confer excellent stability in biomechanical studies18,21,22), so the result of the procedure was good as transarticular screw fixation, especially during flexion and extension21,22).
The fusion rates of Brooks and Gallie technique are 70% to 85%1,7,29) although the rate ranges from 60% to 100% in smaller studies1,2,12,26). The fusion rate among the patients with fracture is higher with interspinous method suggested by Sonntag6). With transarticular screw fixation by Magerl, the fusion rate became higher from 82.6% to 100%5,8,15,19). C1 lateral mass and C2 pedicle screw fixation with polyaxial screw and rod system have been considered to show similar outcome with transarticular screw fixation11,17), however, to maximize the bone fusion rate of these technique, the combination with either a Gallie or a Brook's fusion is necessary28).
Possible complications of sublaminar wiring technique is neuronal injury during the wire passage, especially at the C2 level where the spinal canal narrows compared to C1 level4). Early breakage of wire is also a devastating complication of these techniques. Wires and instrumentation provide only temporary fixation, therefore halo vest immobilization is necessary for successful osseous fusion6).
In spite of great advantage over the wiring technique, the transarticular screw fixation has several drawbacks. Since this procedure requires preliminary reduction of C1 on C2 before the screw insertion and patient's neck flexed to obtain proper guidance of the drill, in some cases, such as irreducible C1 on C2 or the patient with pronounced thoracic kyphosis, the feasibility is restricted. In addition, sufficient space must be available in the pedicle for placement of the screw around the vertebral artery20,24,30). A screw trajectory that is too lateral or too medial can injure the VA or the spinal cord, with disastrous consequences. The incidence of vertebral artery injury has been reported to range between 2.6% and 4.1%10,34).
Harm's technique has technical advantage over transarticular screw fixation in the point of possible vertebral artery injury or the necessity of less operation field during the procedure. However, the procedure has a same risk of neuronal injury with Gallie method when they are combined with sublaminar wiring technique to achieve maximal bone fusion as previously described.
In this study, we have performed Harm's technique with interlaminar fusion using autologous bone and miniplate to maximize bone fusion and minimize complications. The mechanical strength of interlaminar wiring or interspinous wiring might be much superior to miniplate fixation. However, in Harm's technique, wire does not need to support or stabilize C1-C2 segment itself, unlikely in Gallie, Brook, or Sonntag's technique. Because the C1-C2 segment is firmly stabilized with C1 lateral mass and C2 pedicle screw, the miniplate only needs to provide strength enough to stabilize autograft bone between the interlaminar space until successful bone fusion is accomplished. The result of this study that bone fusion between interlaminar space were occurred in eleven out of twelve cases has proven the efficacy of miniplate as a stabilizing device of autograft bone between interlaminar space. Even in case with failed bridging bone formation, the placement of miniplate was not changed. We suspected less decorticated C1 posterior arch or soft tissue might hinder bridging bone formation. By using this miniplate fixation for interlaminar fusion, neuronal or dural injury is no longer concerned. There is no need of dissecting cranial end of posterior arch of the atlas for lack of the necessity of wire passage on it. Dissection on C1 can be reduced to minimal because the exposure to only postero-inferior margin is required for miniplate fixation. Osseous bone fusion rate is as high as other known techniques. Moreover, this procedure can be applied even when the posterior arch of atlas is compromised as long as the posterior arch is partially remained.
Major complications of cervical surgery with posterior approach are due to dissection of midline structures. Patients often complain postoperative neck pain after surgery. In this study, paramedian approach was used in eight cases. We could assure that paramedian approach was possible with this technique because miniplate fixation was technically much easier than the wiring technique. Therefore, we could save nuchal structures which lead to reduction of possible complication after midline incision, result from extensive dissection of midline musculature32).
Yet this study has limitations because the size of data was small and the clinical outcome was not evaluated. In the future, the study with larger group and comparative study with other method will be needed and the assessment of clinical outcomes of patients should be evaluated.
CONCLUSION
Posterior atlantoaxial fusion technique has been constantly developed and modified to achieve better fusion rate and to avoid complications. With our technique using miniplate to supplement C1 lateral mass and C2 pedicle screw fixation, the procedure can be easier and safer to be performed due to the low rate of complications as well as technical facility. Moreover, as minimal invasive surgery becomes possible with this technique, better clinical outcome is expected.