Indications and Surgical Results of Twist-Drill Craniostomy at the Pre-Coronal Point for Symptomatic Chronic Subdural Hematoma Patients
Article information
Abstract
Objective
Twist-drill craniostomy (TDC) with closed-system drainage and burr-hole drainage (BHD) with a closed system are effective treatment options for chronic subdural hematoma (CSDH). The aim of this study was to analyze clinical data and surgical results from symptomatic CSDH patients who underwent TDC with closed-system drainage at the pre-coronal point (PCP).
Methods
We analyzed data for 134 symptomatic CSDH patients who underwent TDC at the PCP with closed-system drainage. We defined the PCP for TDC to be 1 cm anterior to the coronal suture at the level of superior temporal line. TDC at the PCP with closed-system drainage was selected in patients with CSDH that extended beyond the coronal suture, confirmed by preoperative CT scans. Medical records, radiological findings, and clinical performance were reviewed retrospectively.
Results
Of the 134 CSDH patients, 114 (85.1%) showed improved clinical performance and imaging findings after surgery. Catheter failures were seen in two cases (1.4%); the catheters were inserted in the epidural space. Recurrent cases were seen in eight patients (5.6%), and they were improved with a second BHD with a closed-system operation.
Conclusion
TDC at the PCP with closed-system drainage is safe and effective for patients with symptomatic CSDH whose hematomas extend beyond the coronal suture.
INTRODUCTION
The incidence of chronic subdural hematoma (CSDH) is about 3 per 100000 people, but it is 20 times more common among the elderly9). Indeed, its incidence is the highest in persons over 70 years of age8,22). Although CSDH can be treated quite easily, it can sometimes lead to disastrous results due to recurrence and complications. As the population suffering from CSDHs includes many elderly patients with co-morbid medical conditions, less invasive surgical techniques have become the initial procedures of choice1,5,17). Current surgical treatment options also include a variety of less invasive neurosurgical modalities, such as burr-hole drainage (BHD) or twist-drill craniostomy (TDC) with closed-system drainage22).
It is well known that TDC carries a risk of hemorrhagic complications because it is a blind technique4,5,20). However, TDC at the pre-coronal point (PCP) with closed-system drainage for symptomatic CSDH was shown to be a safe entry point in a previous report from our institution5). The aim of this study was to provide more clinical data and surgical results for patients who had appropriate indication and underwent TDC at the PCP with closed-system drainage as a continuation of the previous report; we would like to emphasize its superiority, in terms of convenience and good outcome.
MATERIALS AND METHODS
Definition and indications for TDC at PCP with closed-system drainage
This retrospective study was performed on consecutive symptomatic patients with CSDH who were treated surgically at a single institution from January, 2005 to December, 2010. Among the 208 patient with CSDH, 134 patients underwent TDC at the PCP with closed-system drainage; 74 patients underwent BHD with a closed system and were excluded from the study. TDC at the PCP with closed-system drainage was selected in patients with CSDH that extended beyond the coronal suture, as confirmed by preoperative CT scans. We defined the PCP for TDC in CSDH to be 1 cm anterior to the coronal suture at the level of the superior temporal line (STL). On brain CT scans, the level of the STL was defined as the top of the densest part of the temporalis muscle around the coronal suture. The coronal suture and the STL could be identified clearly on brain CT scans.
Operative procedures
The PCP was identified in each patient in the operation room before draping; it was measured in the usual manner with reference to the external landmarks of the coronal suture and the STL. After scalp preparation with alcohol and a povidone-iodine solution, 2% lidocaine was infiltrated. A stab incision was made using a No. 15 scalpel at the drill entry point. First, a hand drill equipped with a 4 cm-long Steinman pin was placed perpendicular to the surface of the skull, and a mark was made on the outer skull to keep the twist drill from slipping on the surface of the skull. Then, using a 6 cm-long twist drill, the skull and dura were penetrated at a 45° angle to the surface of the bone to prevent the catheter from entering the cortex. The typical direction of the drill was posteroinferior toward the auricle. A standard No. 5 ventriculostomy catheter was introduced into the subdural cavity for 5 cm. The contents of the catheter flowed freely due to the downward orientation of the catheter. Neither aspiration with negative pressure nor flushing with normal saline was performed. The closed-system drainage was formed by attaching the catheter to a ventricular drainage bag and the catheter remained in the hematoma cavity for a few days to drain it slowly (Fig. 1).
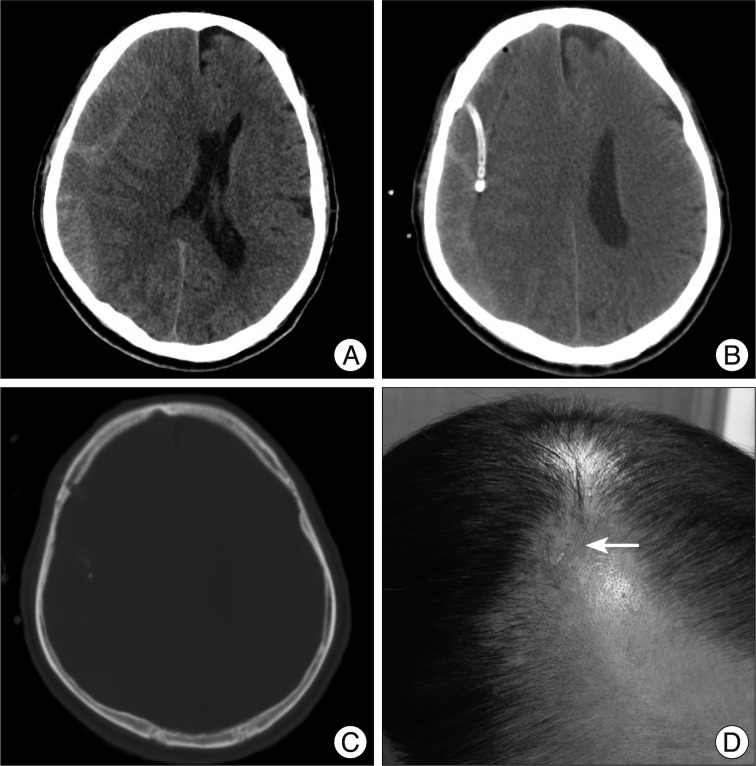
Brain CT scans obtained in a 68-year-old man who presented with drowsy consciousness and motor weakness who underwent TDC at the normal safe entry point. A : Preoperative axial image showing a mixed density lesion compatible with a CSDH in the right frontal and parietal area. B : Axial soft tissue algorithm obtained 3 h after TDC at the PCP with closed-system drainage showing appropriate catheter direction and depth. C : Axial bone algorithm obtained 3 h after TDC at the PCP with closed-system drainage showing an appropriate craniostomy at the normal safe entry point. D : Small operative scar 1 month after TDC at the PCP (arrow). TDC : twist-drill craniostomy, CSDH : chronic subdural hematoma, PCP : pre-coronal point.
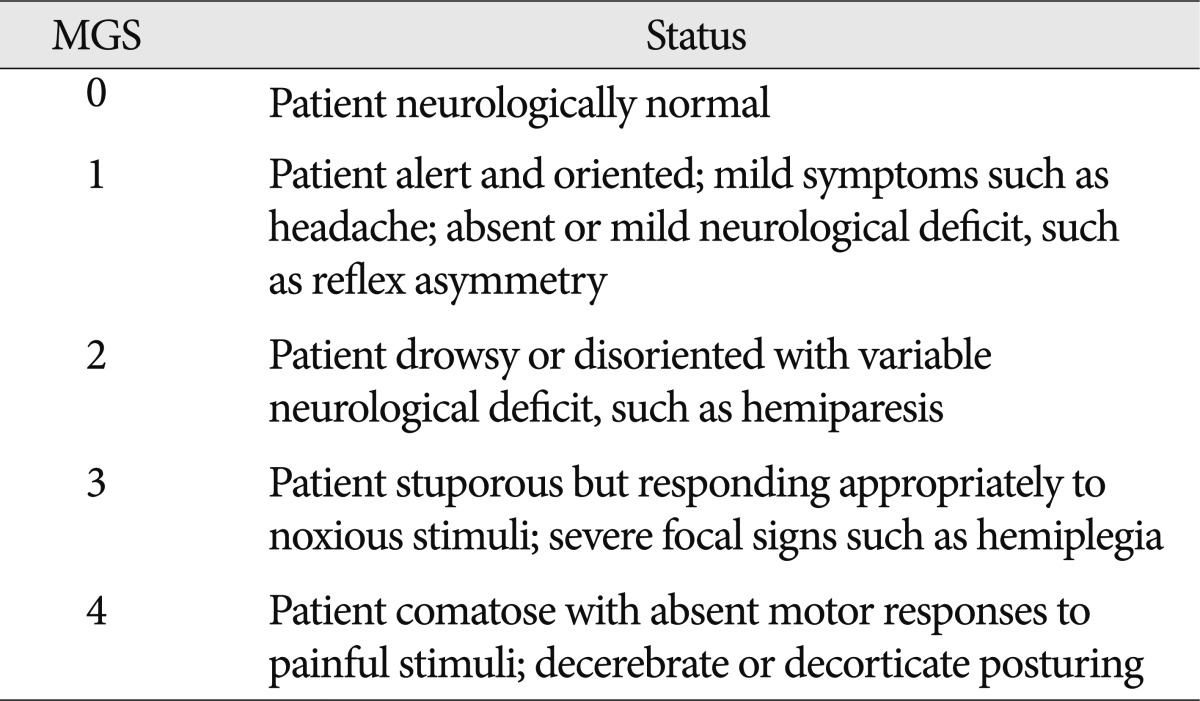
Estimation of surgical results
We recorded demographic data, such as age, gender, coexisting disease, and major neurological functions. Clinical performance was graded and compared using the clinical grades in Markwalder's grading scale at the preoperative period and 3 months after surgery (Table 1). We performed CT scans during the preoperative period. Postoperative CT scans were routinely performed at 3 hours, 3 days and 3 months after surgery. Postoperative air accumulation was defined as dense air around the subdural catheter. CSDH density of preoperative CT scans was classified into 4 categories : high density, isodense, low density, and mixed density.
Catheter failure was defined as an inappropriate position, i.e., not in the subdural space. Postoperative CT scans at 3 hours after the operation confirmed the catheter's position. Recurrence of CSDH was defined as a confirmed post-operative hematoma expansion on postoperative CT scans and aggravation of neurological dysfunction.
RESULTS
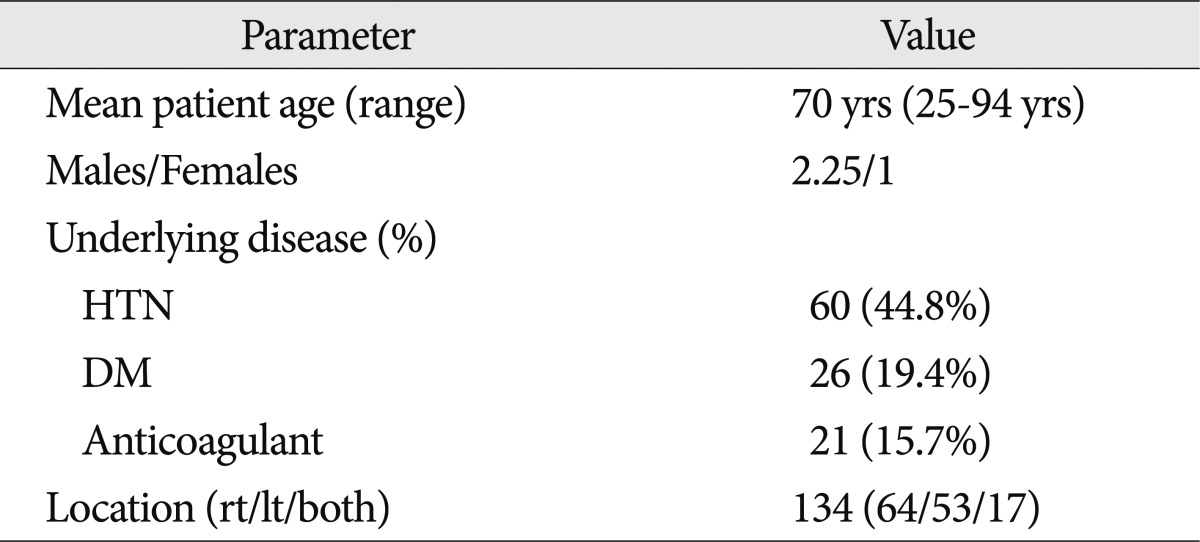
Patient demographic data
Demographic data of the enrolled patients are shown in Table 2. The mean patient age was 70 (range, 25-94) years. The male to female ratio was 2.25 to 1. Of the CSDH patients, 60 (44.8%) had hypertension, 27 (20.1%) had diabetes mellitus, and 21 (15.7%) had taken anticoagulant medications. CSDH developed in the right hemisphere in 64 (47.8%), in the left in 53 (39.6%), and bilaterally in 17 (12.7%).
Preoperative radiological imaging
Preoperative CT findings are shown in Table 3. The mean thickness of the CSDH at the PCP was 21.1 (range, 7.1-39.9) mm on brain CT scans. The mean mid-line shift of brain parenchyma was 10.45 (range, 0-27.34) mm on brain CT scans at the PCP. Many cases showed isodense hematomas (58 cases, 43.3%). Low-density CSDH was seen in 38 cases (28.4%), high-density CSDH in 16 cases (11.9%), and mixed density CSDH in 22 cases (16.4%). Hematoma septation was identified in 43 cases (32.1%).
Postoperative parameters
Clinical postoperative parameters were analyzed, and results are shown in Table 4. The mean operation time was 21 min for both unilateral and bilateral cases (range, 7-63 min). The mean duration of subdural catheter indwelling was 4 (range, 1-8) days. The mean hospital stay was 13.1 (range, 2-67) days. All postoperative TDC except two had congruent points with the measured area in the preoperative brain CT scans. We found air accumulation in 11 patients (7.7%) on postoperative brain CT scans.
Outcome of clinical performance
Clinical performance data as analyzed by the Markwalder Grading Scale (MGS) are shown in Table 5; a lower grade on this scale indicates better cognitive functioning. On admission, the MGS results showed that 109 (81.3%) patients were in Grade 1, 21 (15.7%) in Grade 2, four (2.8%) in Grade 3, and none in Grade 4. Postoperative performance scores were lower; 114 (85.1%) were Grade 0, or normal; 15 (11.2%) were Grade 1, one (1.4%) was Grade 2, and three (2.3%) were Grade 3. The mean value of MGS decreased from 1.21 to 0.21.
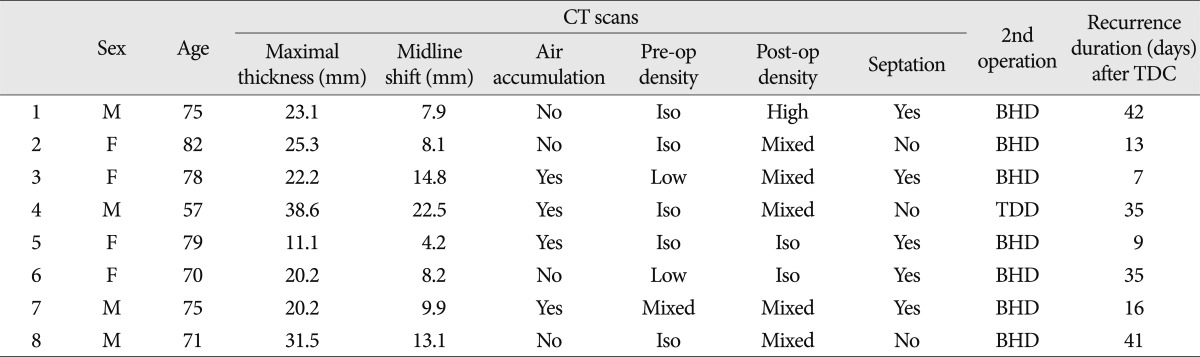
Catheter failures and recurrences
Catheter failure was seen in two cases on postoperative brain CT scans. In both, catheters were inserted in the epidural space. In the first case, we removed the catheter immediately and performed a craniotomy and hematoma evacuation due to the occurrence of an acute epidural hematoma. In the other patient, we performed BHD at the same entry point (Fig. 2). The two patients recovered neurological function fully and were discharged without sequelae.
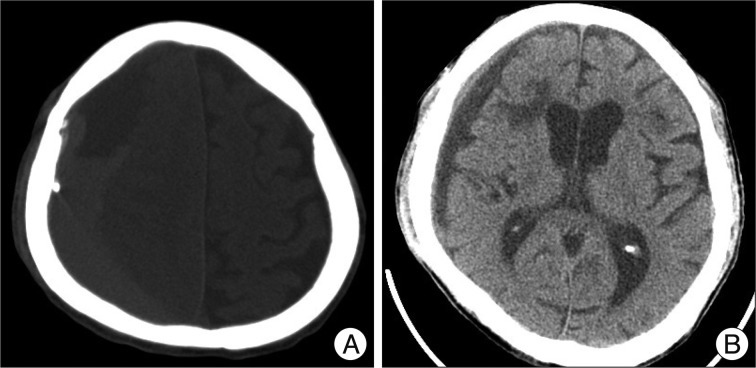
Brain CT scans obtained in a 71-year-old patient who presented with stuporous consciousness and underwent TDC at the PCP with closed-system drainage. However, the subdural catheter was positioned into the wrong space. A : Postoperative axial brain CT scans showing catheter positioned in the epidural space. B : Axial soft tissue algorithm brain CT scan obtained 1 month after BHD. The hematoma had resolved completely, and the patient's neurological function had improved. TDC : twist-drill craniostomy, PCP : pre-coronal point, BHD : burr-hole drainage.
Recurrence was seen in eight (5.9%) patients at a mean of 24.8 (range, 7-42) days after TDC at the PCP with closed-system drainage (Table 6). Of these, seven patients underwent revised BHD at the hematoma maximal point. One patient underwent a revised TDC at the same point. The mean hematoma thickness was 19.2 (range, 11.1-31.5) mm. In seven of the eight (87.5%) patients with recurrence, the hematoma location was on the right. In seven patients, the hematoma density of the postoperative CT scan was higher than that of the preoperative CT scans. Hematoma septation was seen in five cases.
DISCUSSION
Chronic subdural hematoma is a frequently encountered problem in neurosurgical practice10). Many elderly patients with co-morbid medical condition suffer from CSDH. They needed simple and short time technique to treat CSDH18). Many studies have demonstrated that TDC using closed-system drainage is an effective operation technique for CSDH5,13,18). It was first introduced as a diagnostic procedure in 196614). Since then, many studies have demonstrated that TDC using closed-system drainage is an effective procedure for CSDH as a definitive treatment modality16,22). However, the reports to date make reference to the craniostomy performed in many different locations, such as the rostral or anterior part2,4,21) or the maximal thickness site15,20,22). We hypothesized that TDC is more comfortable, easy and fast procedure if definite entry point was set up5). Therefore, our institute set up PCP for TDC based on the brain image and the surface landmark of the scalp. We defined PCP for TDC against CSDH to be 1 cm anterior to coronal suture at the level of the STL. To prevent the twist drill and catheter from entering the cortex, we outlined the two steps of surgical techniques. First, a hand drill equipped with a Steinman pin with 4 cm length is placed perpendicularly to the surface of the skull and a mark was made on the outer skull to keep the twist drill from slipping down the skull. Second, using the twist drill with 6 cm length, the skull and dura are penetrated at 45° angle to the surface of the bone.
Our study was analyzed concerning patients' good outcome to compare with other reports. As the result of our study, patient's clinical performance was downgraded 1.21 to 0.21. One-hundred-and-fourteen (85.1%) of total 134 patients showed improved clinical symptom and neurological function. Muzii et al.11) reported a prospective series of 22 patients treated with TDC and closed suction drainage. There was 90.9% of recovery rate at only MGS 0. Camel and Grubb2) obtained a good outcome in 86% of their patients. Although operation method was different from other reports, outcome was better than other reports. In our series, operation time including measuring PCP was average 21 minutes. Muzii et al.11) reported a prospective series of 22 patients treated with TDC and closed suction drainage. The mean operation time was 25.2 minutes and their operation time was faster than BHD. Williams et al.22) reported the mean operation time as 25 minutes. The major difference from other reports was definite set up entry point. The point measuring accuracy was 98.5% in our cases. The PCP has advantage as it allows surgeons to confirm from scalp land mark. Also, it is easier and less stressful to operator. However, TDC carries the risk of hemorrhagic complications because it is blind technique. Injury of middle meningeal artery during TDC may cause the development of epidural hematoma. Acute epidural hematomas may result from detachment of dura from the inner surface of the skull as a result of a relatively blunt drill, without penetrating into the SDH cavity20), or rapid decompression of CSDH. We have experienced catheter failure on epidural space in 2 cases. Based on our experience, we recommend two important things during TDC; first is to confirm crank-oil color hematoma draining, and second is to twist fast to penetrate dura mater. Slow drilling might make dura mater detached from cranial bone. It is easy to twist slowly because the inexperienced operator may fear from penetration brain injury. Unintentional brain damage can be avoided by drilling through the skull and passing the catheter into the subdural cavity tangentially1,3,5).
In our series, the recurrence rate was 5.9% (8 case). The patients undergone TDC had range of 9-64% in previous reports. So, many other reports did not recommend first line choice to treat TDC in CSDH patients because of high recurrence rate9,19,22). Other reports are to propose post-operative hematoma density6,8,12) and air accumulation in recurrence factor7,8,19). Our series showed relatively low recurrence rate (5.9%) possibly because of low incidence of air accumulation than other reportsr7,19). We had only 7.7% in postoperative air accumulation rate. However, our recurrent cases had higher density than preoperative hematoma density and showed air accumulation in 7 cases. In addition, brain expansion and compliance function decreased due to aging process. Patients with recurrent accumulation underwent second operation with BHD with closed-system in maximal thickness point and the patients improved after surgery.
CONCLUSION
The PCP for TDC was defined as 1 cm anterior to the coronal suture at the level of the STL. This point can be accurately estimated on the scalp using surface landmarks. TDC at the PCP with closed-system drainage is proved to be safe and effective for patients with symptomatic CSDH whose hematomas extended beyond the coronal suture.
Acknowledgements
This work was supported in part by the Soonchunhyang University Research Fund.