INTRODUCTION
Syringomyelia is a disease that produces fluid-containing cavities in the parenchyma of the spinal cord. Syringomyelias are mainly divided into hindbrain-related and nonhindbrain-related forms. Chiari type I malformation with a herniation of the cerebellar tonsil through the foramen magnum is the most frequent form, and post-traumatic syringomyelia is the most common nonhindbrain-related form of this condition.
Various surgical procedures for the treatment of post-traumatic syringomyelia have been introduced recently. Depending on the cause and type of syringomyelia, the procedures chosen to correct this condition include posterior fossa decompression, spinal subarachnoid space reconstruction, bisecting the filum terminale, spinal cord transection, myelotomy, and various cerebrospinal fluid (CSF) diversion procedures, such as lumbo-peritoneal, syringe-pleural, syringe-subarachnoidal, and syringe-peritoneal shunting4,7,14). However, most surgical strategies have been unreliable, especially in cases of shunt procedures.
We introduce the concept and technique of a new shunting procedure: syringo-subarachnoid-peritoneal shunt.
CASE REPORT
A 54-year-old patient presented to our hospital with a 5-day history of progressive impairment of motion and position sense on the right side. Sixteen years before this admission, he had been treated by a decompressive laminectomy against a burst fracture of L1, and has suffered from incomplete paraplegia. Five days before his recent admission, he was in a minor traffic accident. Afterwards, an impairment of his motion and position sense developed on the right lower extremity which has gradually aggravated to the right upper extremity.
His neurological examinations revealed impairment of all sensory functions including motion and position sense on his right side, and a newly developed motor weakness of the right upper extremity (Grade IV). He complained of paresthesia on his whole right side. MR images of the whole spine revealed the presence of a huge syrinx extending from the medulla to the L1 level (Fig. 1). No evidence of hindbrain herniation or hydrocephalus was revealed.
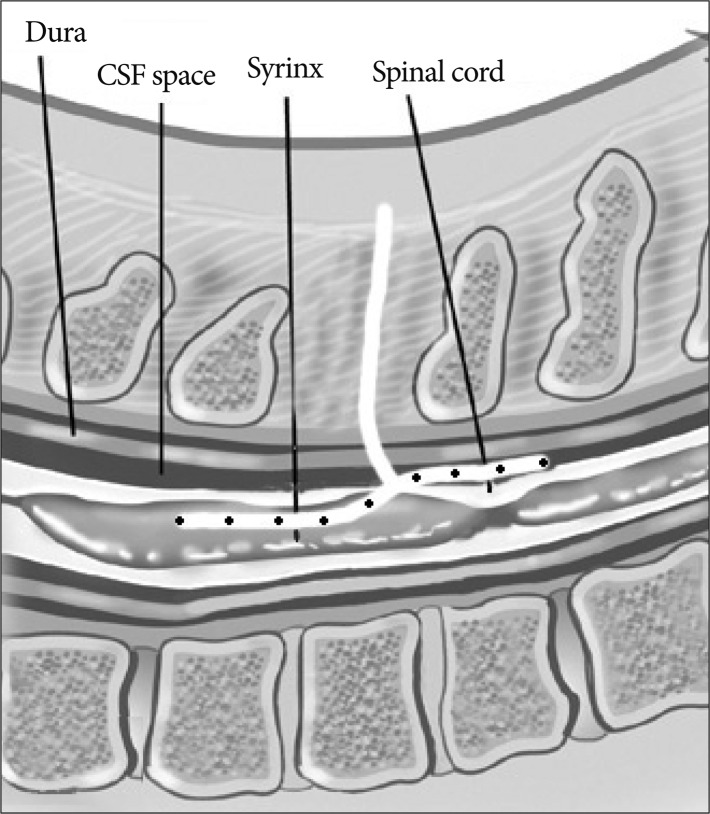
We performed the syringo-subarachnoid-peritoneal shunting procedure with T-tube (CSF-Lumboperitoneal Shunt, T-tube; Medtronic Neurosurgery, Goleta, CA, USA). The patient was placed in a prone position. We choose T9 vertebral level for the myelotomy site, because it was the widest portion of syrinx, the thinnest portion of the spinal cord and the least potential site for a new neurological deficit. After the T9 laminectomy, incision of dura and arachnoid membrane, we made a small myelotomy at the dorsal root entry zone. The T-tube arms which have many side holes, are cut to the desired length and one arm is inserted into the syrinx (rostral direction), the other arm into subarachnoid space (caudal direction) (Fig. 2). After a tight suture of the dura, fascia and skin, we passed the distal tip through subcutaneous space, and connected to the reservoir in the subcutaneous pocket at a costovertebral angle. After positioning the patient in a supine position, we inserted a peritoneal catheter into the peritoneal cavity using the standard technique.
On his neurological examination 6 months after the operation, motor power of the right upper extremity was normalized, and sensory function, including proprioceptive sense, was markedly improved except for the right fingers. Several magnetic resonance (MR) images performed during two years after surgery have shown a considerable reduction in the size of the syringomyelic cavity (Fig. 3).
DISCUSSION
The goal of surgery for syringomyelia should be to reverse any anatomical abnormality that is presumed to have caused the syrinx. The hydrodynamic theory, based on Gardner6) and Williams18), states that CSF pressure gradients between the cranium and the spine in patients with hindbrain herniation allow for the development of a syrinx as CSF is drawn into the more yielding areas of the spinal cord. Therefore, the procedure of choice in this hindbrain-related syringomyelia is posterior fossa exploration for hindbrain decompression.
After trauma, spinal injury produces numerous abnormalities, such as subarachnoid adhesions, spinal deformity or stenosis that could disturb CSF flow and contribute to syrinx enlargement. The presence of uncorrected kyphosis and stenosis correlate with syrinx formation and symptom severitiy8,10-12), and subarachnoid adhesion results in obstruction of CSF pathways5). Therefore, subarachnoid space reconstruction from correction of causative deformity, decompression of the spinal cord, or adhesiolysis of subarachnoidal scarring and duroplasty should be considered preferentially to diversion of CSF flow1,4,14).
Shunt operations were widely used in the 1970s and 1980s with encouraging early results, although long-term effectiveness has been questioned recently. Various cerebrospinal fluid diversion procedures, such as syringe-subarachnoidal, theco-peritoneal, syringe-pleural, and syringe-peritoneal shunting have been introduced recently, but most have been unreliable and have limitations2,3,9,13,15,16). Sgouros and Williams observed that a large proportion of patients with syringe-pleural shunts needed subsequent surgery within one year. They also observed a high number of postoperative neurological complications13), Batzdorf roreported a higher rate of shunt failure (approximately 50%) and poor long-term outcome from his various shunting procedures including syringe-peritoneal shunt, syringo-pleural shunt, subarachnoid shunt and lumbo-peritoneal shunt3). Most recently, Aghakhani et al.1) reported a considerable number of recurrences (73%), and aggravation of symtoms (40%) after the shunting procedure, for a mean follow-up of 86 months.
The main cause of the high recurrence rate and poor outcome after shunting procedure is shunt obstruction1,3). It is probably most often the result of the collapse of the syrinx cavity around a shunt tip. Batzdorf identified proximal obstruction as the most common source of shunt malfunction, and demonstrated ingrowth of glial tissue into the perforations of the tube as the cause of shunt failure3). We tried to overcome the proximal obstruction by using a T-tube having many side holes on its two arms. Some authors used the T-tube in the past, but their techniques had some limitations2,9,17). One is the fact that the rotational forces of the T-tube can damage the spinal cord. The other limitation is the difficulty in removing the T-tube without cord injury, when there are complications such as obstruction, infection or cord compression. However, in our new shunting procedure, we inserted just one arm of the T-tube into the syrinx cavity and located the other arm outside the cord, in the subarachnoid space. Therefore, we can not only protect the cord from tube rotation, but also remove the tube easily.
The linear catheter used in various shunting procedures also has some limitations. Another main cause of shunt malfunction is shunt dislocation, frequently occurring in syringostomy or syringosubarachnoidal shunt using the linear catheter. However, using T-tube has another advantage: we can easily anchor the tube to the dura, and thus prevent migration resulting in shunt malfunction (Fig. 2).
The greatest advantage of our method is that there are free connections between the three spaces: syrinx, subarachnoid space, and the peritoneal cavity. CSF can flow from syrinx to subarachnoid space and peritoneal space or from subarachnoidal space to peritoneal cavity according to the pressure gradient. Our shunt system can theoretically operate as syringe-subarachnoidal shunt, syringe-peritoneal shunt and theco-peritoneal shunt.
Currently, subarachnoid space reconstruction by combining arachnolysis and duroplasty appears to be one best treatment in posttraumatic syringomyelia. Shunt placement may be elected when other causative treatments have failed, when adhesiolysis is impossible due to extensive adhesion, or when combined with subarachnoid space reconstruction. If it is needed, we recommend the syringo-subarachnoid-peritoneal shunt operation.
CONCLUSION
The syringo-subarachnoido-peritoneal shunt using T-tube has many advantages and makes up for the defects of other shunts. First, fluid can communicate freely between the syrinx, the subarachnoid space, and the peritoneal cavity according to the pressure gradient. Secondly, we can prevent the shunt catheter from migrating because dural anchoring of the T-tube is easy and solid. Finally, we can perform shunt revision easily because only one arm of the T-tube is inserted into the intraspinal syringx cavity. The treatment of choice is subarachnoid space reconstruction and augmentation in posttraumatic syringomyelia, but, when a shunt is needed, we think that this procedure is the most beneficial method among the various shunting procedures.