INTRODUCTION
The diagnosis of a peripheral nerve lesion depends primarily on the patient's history, physical examination, and electrophysiologic studies. However, accurate localization of a peripheral nerve lesion is sometimes difficult without the aid of imaging studies. The visualization of peripheral nerve lesions can be accomplished with ultrasonography or magnetic resonance imaging (MRI). Ultrasound can be very useful in the diagnosis of peripheral nerve lesions because it provides a dynamic image and it can be used to trace a nerve's course towards the site of the suspected lesion. Gross abnormalities of a nerve that may benefit from surgical intervention, such as entrapment neuropathy due to ganglion, nerve sheath tumor, or traumatic disruption of the nerve, can be easily detected15).
When a peripheral nerve lesion is suspected after history and physical examination or electrophysiologic studies, an ultrasound tracing of the involved nerve along its whole anticipated course can be expected to have diagnostic value in detecting the cause of the neuropathy.
Here, we present 3 cases of peripheral neuropathy wherein the causative lesion was diagnosed via simple tracing of the affected nerve using ultrasound.
CASE REPORT
Case 1
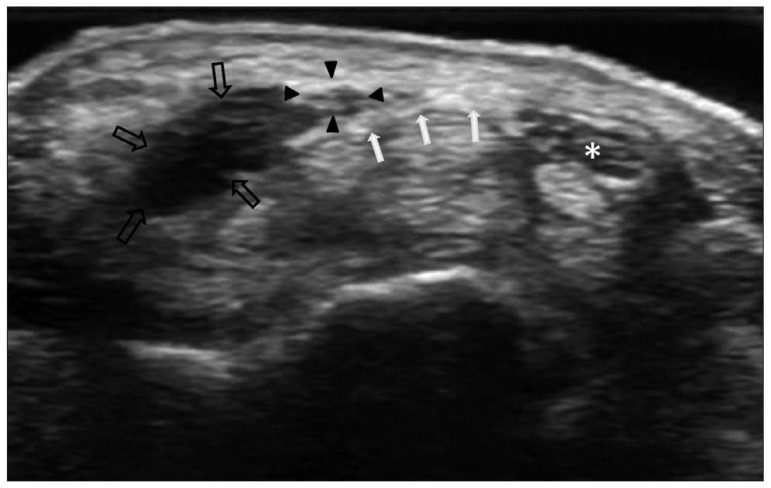
A 50-year-old female presented with one week of numbness and tingling over the ulnar side of her right wrist, hand, and fourth and fifth fingers. There was no known history of trauma or injury to her head, neck, or right upper extremity. There was no evidence of muscle atrophy or skin changes in the affected extremity on physical examination. The hypothenar aspect of the right hand and the palmar side of the fourth and fifth fingers showed decreased sensation to light touch. Tinel's sign over the right ulnar nerve at the elbow and wrist and the median nerve and Phalen's test were all negative. Squeezing power of the fourth and fifth fingers of the right hand was decreased. Froment's sign was positive. Under the impression of right ulnar neuropathy, electromyogram (EMG) and nerve conduction velosity (NCV) were performed. Surprisingly, the electrophysiologic studies showed only mild median nerve abnormalities, and there were no abnormal findings on the right ulnar nerve. We had little confidence in these findings because of the short duration of the patient's symptoms, and ultrasound scanning of the right ulnar nerve along its expected course from the level of the elbow level distally was performed, revealing a mucoid cystic mass compressing the ulnar nerve at the proximal portion of Guyon's tunnel (Fig. 1).
Case 2
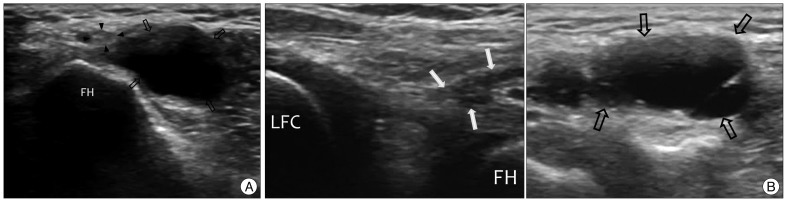
A 55-year-old male presented to the outpatient department complaining of left foot drop that had developed 4 days previously. He had neither back pain nor leg pain. He first noticed the symptom after mountain climbing. He was initially seen by a spine specialist and had undergone a lumbar MRI, which showed only mild central disc bulging at the L3-L4 intervertebral space. The findings were not concordant with the patient's symptoms. Sensation over the anterolateral aspect of the left lower leg and dorsum of the left foot was decreased to light touch and there was weakness of left ankle dorsiflexion with a grade of 2 on the Medical Research Council scale for muscle strength. The presumptive diagnosis was a left peroneal neuropathy, and ultrasound scanning along the left peroneal nerve was performed from the distal sciatic nerve, revealing a mucoid cystic lesion compressing the left common peroneal nerve near the fibular head (Fig. 1A). The cyst was connected to the posterolateral aspect of the knee joint (Fig. 2B, C).
Case 3
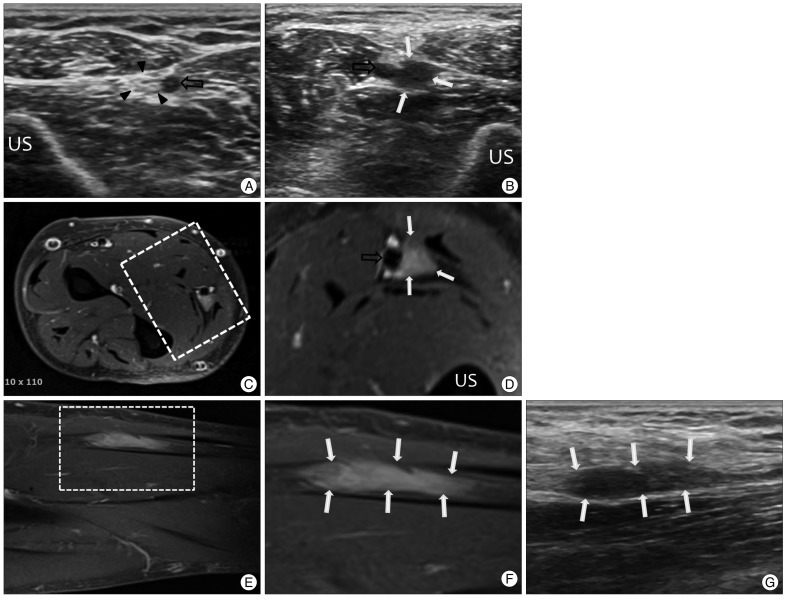
A 48-year-old female presented with intermittent weakness of the left hand that had manifested as dropping of spoon or cup while eating. On physical examination, there was no gross atrophy or skin change noted on the affected hand. There was a mild decrease in sensation over the left ulnar nerve territory, but the motor power of the hand was relatively intact. Tinel's sign over the left ulnar nerve at the elbow and wrist was negative. CT of the cervical spine was negative with regard to the corresponding physical findings. EMG and NCV studies indicated a left ulnar neuropathy below the elbow level, and ultrasound scanning of the left ulnar nerve along its expected course from the elbow level distally was performed, revealing a mass lesion surrounding the left ulnar nerve at the mid-forearm level (Fig. 3A, B, G). A subsequent MRI showed a 3.7√ó0.5√ó0.5 cm tubular enhancing mass along the left ulnar nerve (Fig. 3C-F), consistent with neurogenic tumor (neurofibroma or schwannoma).
DISCUSSION
Over the last decade, ultrasonography of peripheral nerves has advanced technically, and multiple studies have confirmed that ultrasound is highly sensitive and specific in the diagnosis of peripheral nerve lesions, sometimes rivaling the efficacy of electrophysiologic studies14). In diagnosis of carpal tunnel syndrome, sensitivity of ultrasound is reported to reach over 96%7).
Electrophysiologic studies, MRI, and ultrasound are the main modalities for the evaluation of peripheral nerves. Electrophysiologic studies are sensitive tests used to evaluate patients with suspected peripheral neuropathy, but it cannot visualize the exact anatomical peripheral nerve lesion. Moreover, the interpretation of nerve conduction studies is complex and sometimes vague.
MRI and ultrasound provide high-resolution images of the peripheral nerves. They provide supplementary information to the clinical history and physical examination and electrophysiologic studies regarding the possible cause of a peripheral neuropathy. Conventional MRI and magnetic resonance (MR) neurography have good resolution and provide much information on peripheral nerve lesions5). MRI also has the advantage of being able to detect minor nerve edema and perfusion abnormalities, and can be used for preoperative evaluation and surgical planning in patients with peripheral nerve lesions9). However, the use of MRI is limited by difficulty in its accessibility as well as cost and time constraints.
Ultrasound, in spite some shortcomings, such as a long learning curve and an operator dependent nature, provides an effective method of scanning an entire peripheral nerve along its course in the limbs, and it is cost effective and non-invasive. It also enables dynamic scanning and can sometimes provide better resolution than MRI. Most of all, ultrasound is quick and easily accessible, which are major advantages over MR imaging.
Ultrasound scanning of peripheral nerves can detect minimal changes in nerve size and echotexture. It is useful for diagnosis of entrapment neuropathy, traumatic injury, and tumors and inflammation of the peripheral nerves8). Furthermore, measuring the cross sectional area of a peripheral nerve with ultrasound is known to have diagnostic value in nerve entrapment syndromes10). This has been widely studied, particularly in carpal tunnel syndrome11).
Normal nerves are oval-to-round echogenic structures with internal punctate echoes on transverse scan, and can sometimes look honeycombed2). Nerve tracing methods using ultrasound can be very easy if the operator has some knowledge about the course of the peripheral nerves and their function. The standard technique for examining nerves is by tracing of the nerve through its expected course. The nerve is centered in the field of view of the ultrasound image with short-axis scanning technique. The transducer is swept upwards or downwards along the course of the nerve. Bianchi and Martinoli3) call this method the "lift technique". This method is very simple and reliable for the evaluation of long nerve segments. The operator can detect possible intrinsic and extrinsic abnormalities with simple scanning and tracing of the suspected nerve.
In Cases 1 and 3, ulnar nerve pathologies were suspected after physical examination and electrophysiologic studies. The entire ulnar nerve was scanned with ultrasound, which led in each case to the detection of the causative lesion along the nerve course.
In contrast to carpal tunnel syndrome, there are multiple potential sites of entrapment neuropathy of the ulnar nerve at the elbow12), and the sensitivity of electrophysiologic studies for patients with ulnar neuropathy at elbow is much lower than for median mononeuropathy at the wrist17). The sensitivity of ultrasound evaluation of ulnar neuropathy, however, is as high as that of MRI13). Thus, ultrasound is expected to play an increasingly important role in diagnosis of ulnar neuropathy.
Case 2 was a case of entrapment neuropathy of the common peroneal nerve induced by a ganglion cyst. As seen in Fig. 2B and C, the pedicle of the ganglion cyst was connected to the posterolateral corner of the knee joint. Ultrasound guided aspiration of the ganglion was performed in this case, which allowed immediate decompression of the nerve and assisted in formulating the subsequent therapeutic plan.
Ultrasound has potential as a first-line confirmatory test, instead of electrophysiologic studies6), in peripheral neuropathy, and occasionally ultrasound will reveal abnormalities than the clinical or electrophysiological examination do not detect. It will also show nerve pathology that is not noted in those examinations1,17), as was demonstrated here with Case 1.
Ultrasonography can provide a reliable diagnosis of soft tissue tumors with accurate estimation of the volume of the lesion and precise three-dimensional localization of the abnormality4). Ultrasound has also demonstrated high diagnostic accuracy for peripheral nerve sheath tumors, with neurilemmoma indicated by an ovoid or lobulated encapsulated hypoechoic mass oriented longitudinally in the nerve distribution with tapered ends of the nerve at both sides16), as noted in Case 3.
We propose that more frequent application of ultrasound for the evaluation of peripheral nerve lesions can provide more accurate and expeditious diagnosis.
CONCLUSION
The cases presented here illustrate the value of ultrasound tracing of peripheral nerves as a useful and dynamic screening tool in the evaluation of peripheral nerve lesions. Ultrasound has high sensitivity and specificity, and it has been well-documented that ultrasound is a very useful diagnostic modality for peripheral entrapment neuropathy and peripheral nerve sheath tumors. If a lesion of the peripheral nerve is suspected after history and physical examination or electrophysiologic studies, an ultrasound scan tracing the peripheral nerve of interest throughout its entire course can be very helpful for diagnosis of the causative lesion.