INTRODUCTION
Reports of penetrating craniofacial injuries due to construction equipment are increasing around the world4). Such injuries are typically caused by metal or biological tissue fragments (bone, teeth). Angle grinders consist of high speed revolving discs that can cut concrete or metal2) and can cause high velocity penetrating injuries if they are broken during use.
We present a case that illustrates the utility of computed tomography (CT) as an adjunct not only in the detection and localization of intracranial foreign bodies but also to evaluate the hemodynamic status of cerebral blood flow5). Appropriate management of the compromised cavernous sinus and intracranial carotid artery (ICA) using the skull base approach can prevent fatal injuries.
CASE REPORT
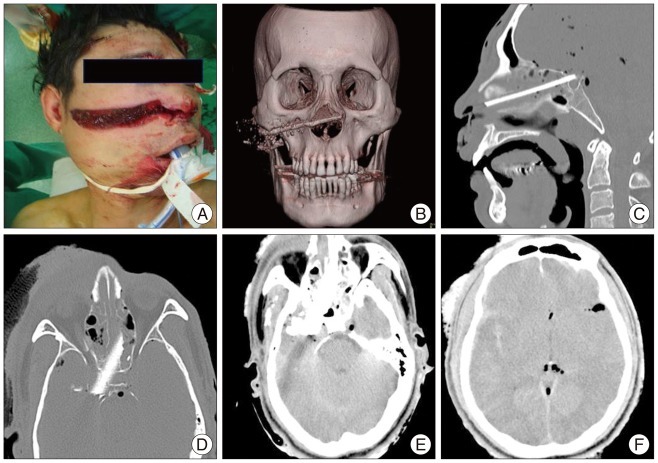
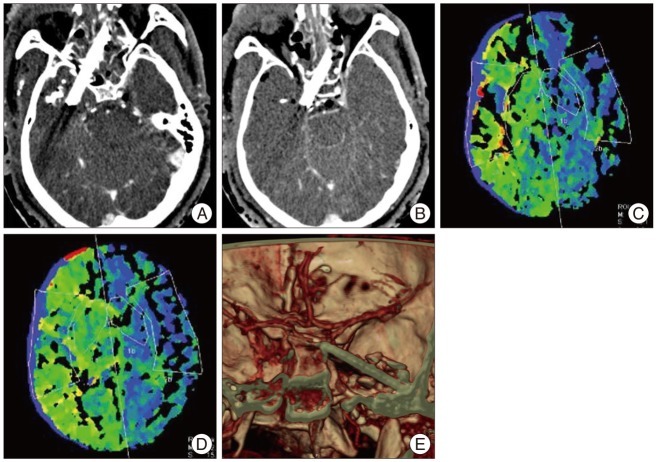
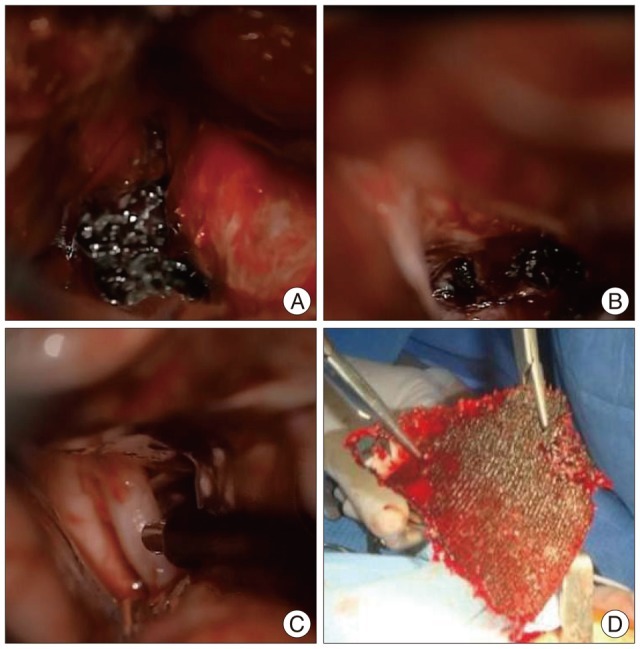
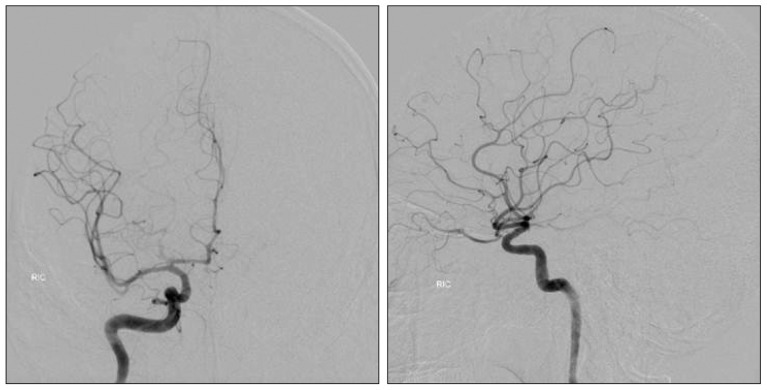
A 46-year-old man suffered a penetrating injury to the face from the broken blade of an industrial grinder while doing demolition work. He was transferred to the emergency room with fading mental awareness. The facial laceration was 15 cm in length from nose to right cheek (Fig. 1A). A piece of the broken blade was observed in the deep portion of the facial wound. Facial bone CTs revealed a blade fragment in the anterior skull base from his nose to the dorsum sellae area (Fig. 1B-D). Brain CTs demonstrated the involvement of the right temporal lobe, cavernous sinus, paraclinoid segment of the carotid artery (Fig. 1E). Also there were traumatic subarachnoid hemorrhage, pneumocephalus without apparent low attenuation area of the right ICA (Fig. 1F). Raw data from CT angiography revealed non-visualization of the right carotid artery while left carotid artery density was visible (Fig. 2A, B). The paraclinoid area was occupied by the foreign body, suggesting ICA encroachment. Delayed time to peak of the right side was noticed on perfusion CT suggesting right carotid artery occlusion (Fig. 2C, D). Progressive left side weakness developed after admission. Because of the patient's critical condition, we needed prompt management to restore blood flow without digital substraction angiography (DSA). Emergency skull base surgery was planned to unblock the cavernous sinus. And then we considered extracranial to intracranial high flow arterial bypass in case of flow decrement on the right ICA. Conventional craniotomy was performed on the right pterional area. After extradural removal of the anterior clinoid process, micro-Doppler revealed restoration of carotid flow to the paraclinoid segment (Fig. 3B). Intradural inspection revealed displacement of the carotid artery due to the foreign body (Fig. 3B). The carotid artery was found to be impinged between the foreign body and anterior clinoid process, as expected from the CT angiography image (Fig. 2E). Microscopic investigation of the intracranial lesion revealed disruption of the pituitary stalk and fracture displacement of the dorsum sellae, but not open injury to the intracranial ICA. A flow meter revealed 40 mL/min flow to the paraclinoid ICA (Fig. 3C). The planned bypass surgery was cancelled. Eight hours elapsed from occlusion to reopening. Surgical glue was injected into the cavernous sinus to restore hemostasis. The broken blade was extracted from the face (Fig. 3D) without no massive bleeding. The wound was irrigated and the bone defect was closed with artificial dura and the temporalis muscle. Lumbar puncture and draining was performed to prevent leakage of cerebrospinal fluid (CSF) from the wound. And then, the surgery for Lefort I fracture and soft tissue defect on the right cheek was done by plastic surgeon. The patient recovered from his left side weakness and additional surgery to treat an infected wound was successful. The patient suffered from severe brain swelling due to ischemic brain injury on the lesion side but recovered fully after barbiturate coma therapy with the ICP monitoring for a week. He was treated with hormone replacement, including hydrocortisone and T4, due to the pitutitary stalk injury. Complete recanalization of the right ICA was confirmed by the DSA which was performed at 2 months after surgery (Fig. 4). He was discharged three months after admission without any motor weakness.
DISCUSSION
High resolution CT (HRCT) is useful for evaluating the severity of damage to intracranial structures. When HRCT is performed alongside CT angiography or perfusion CT, it is possible to assess vascular injuries at the same time4).
Since damage to the carotid artery by penetrating foreign bodies can cause fatal consequences, action for the immediate restoration of blood flow is always necessary. Arterial dissection by foreign bodies often develops, and bypass surgeries or endovascular approaches can be applied to restore blood flow3). In the present case, the foreign body was located in the paraclinoid ICA and distal ICA was not observed on the source image from CT angiography. We presumed that there was no blood flow in the right ICA due to a delay in the time to peak on the right side from perfusion CT. Prompt treatment was needed to restore blood flow, similar to stroke management from acute ICA occlusion, but it was impossible to apply endovascular therapies because the ICA was displaced and compressed by the foreign body. Therefore, we planned emergency high flow bypass surgery without DSA considering the patient's critical condition.
Because a blade penetrated our patient's cranium from the nose to the dorsum sellae area and right cavernous sinus, we anticipated that there would be massive sinus bleeding if we extracted the blade from the external wound. Therefore, we took appropriate measures to control massive sinus bleeding before extraction. Among these measures, Sekhar et al.6) reported that the injection of glue is effective to prevent bleeding in cases of possible cavernous sinus or venous plexus bleeding during removal of a foreign body penetrating the cavernous sinus.
Using the same method to control sinus bleeding, we removed anterior clinoid process and performed sinus unroofing. After these manipulations, the compressed ICA was decompressed, blood flow was restored and the bypass surgeries became unnecessary.
We were concerned about severe brain edema and ischemic brain injury, and therefore acted to prevent secondary brain injury by performing decompressive craniectomy and administering barbiturate coma therapy.
The main complications after penetration of the foreign body were infection and CSF leakage1). Devitalized tissues and clots should be removed followed by meticulous homeostasis and watertight dural closure, to avoid CSF fistulae, prevent cerebral infestation, and provide an important barrier to infection1). If the defect is large, it can be closed with pericranium, fascia lata, or temporalis fascia and fibrin glue as a sealant followed by prophylactic CSF lumbar drainage. In the present case, the wound was irrigated and the bone defect was closed with artificial dura and the temporalis muscle. Lumbar puncture and draining were performed for the prevention of CSF leakage from the wound.
CONCLUSION
Prompt treatment is very important in acute carotid artery occlusion. Especially, the injection of glue is effective to prevent bleeding in cases of possible cavernous sinus or venous plexus bleeding during removal of a foreign body penetrating the cavernous sinus. We have presented photos and illustrations describing the appropriate management of ICA occlusion due to penetrating head wounds.