Kim, Chang, Choi, and Jung: Mortality and Real Cause of Death from the Nonlesional Intracerebral Hemorrhage
Abstract
Objective
The case fatality rate of nonlesional intracerebral hemorrhage (n-ICH) was high and not changed. Knowing the causes is important to their prevention; however, the reasons have not been studied. The aims of this study were to determine the cause of death, to improve the clinical outcomes.
Methods
We retrospectively analyzed consecutive cases of nonlesional intracerebral hemorrhage in a prospective stroke registry from January 2010 to December 2010.
Results
Among 174 patients (61.83±13.36, 28-90 years), 29 patients (16.7%) died during hospitalization. Most common cause of death was initial neurological damage (41.4%, 12/29). Seventeen patients who survived the initial damage may then develop various potentially fatal complications. Except for death due to the initial neurological sequelae, death associated with immobilization (such as pneumonia or thromboembolic complication) was the most common in eight cases (8/17, 47.1%). However, death due to early rebleeding was not common and occurred in only 2 cases (2/17, 11.8%). Age, initial Glasgow Coma Scale, and diabetes mellitus were statistically significant factors influencing mortality (p<0.05).
Conclusion
Mortality of n-ICH is still high. Initial neurological damage is the most important factor; however, non-neurological medical complications are a large part of case fatality. Most cases of death of patients who survived from the first bleeding were due to complications of immobilization. These findings have implications for clinical practice and planning of clinical trials. In addition, future conduct of a randomized study will be necessary in order to evaluate the benefits of early mobilization for prevention of immobilization related complications.
Key Words: Intracerebral hemorrhage · Cause of death.
INTRODUCTION
Spontaneous or nonlesional intracerebral hemorrhage (n-ICH) is a major cause of morbidity and mortality in stroke patients 11). Overall, stroke case fatality (ischemic stroke and subarachnoid hemorrhage) has shown a gradual decrease 9). However, the case fatality rate of n-ICH has not changed and it is higher than that of ischemic stroke. Complications of ischemic stroke and the causes of the complications have been reviewed extensively 2,12), however, there has been little discussion of the complications and causes of death in hemorrhagic stroke. Compared with ischemic stroke, for which therapeutic advancements have been made for improvement of clinical outcome, management of n-ICH generally involves supportive care only, because no specific treatments have been shown to improve outcome. Therefore, knowing the causes of death is important to prevention and reduction of complication related mortality, and essential for improvement of clinical outcomes. The objective of this study was to identify and analyze the causes of death in n-ICH patients.
MATERIALS AND METHODS
Patients admitted to a single stroke center between January 2010 and December 2010 with a diagnosis of n-ICH were included in this study. The diagnosis of n-ICH was confirmed from computed tomography (CT) scan and/or magnetic resonance (MR) image and/or digital subtraction angiography. Patients were excluded if the lesions were determined to be caused by trauma, aneurysm, arteriovenous malformation, or tumor. To investigate the risk factors for cause of death in n-ICH patients, we analyzed multiple factors with review of their medical records, radiological findings, and clinical results. All statistical analyses were performed using the SPSS program (version 19.0; SPSS Inc., Chicago, IL, USA). Pearson's chi-square tests were used for comparison of categorical variables and continuous variables were reported as mean±standard deviation (SD) and compared using independent Student t-tests. Multivariate logistic regression analysis was performed for determination of risk factor variables associated with case mortality. A probability less than 0.05 was considered statistically significant.
RESULTS
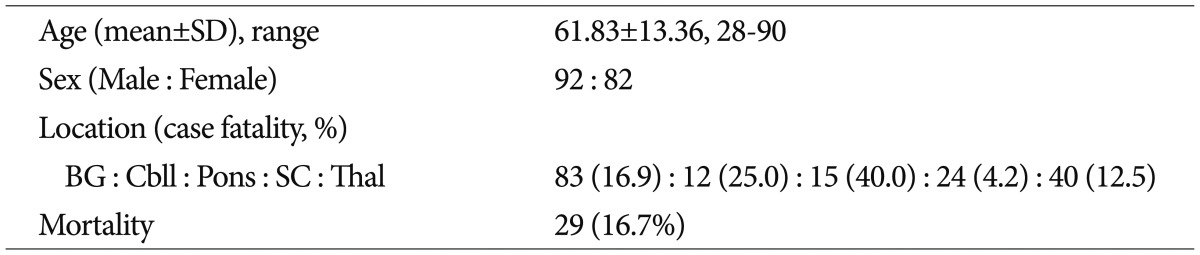
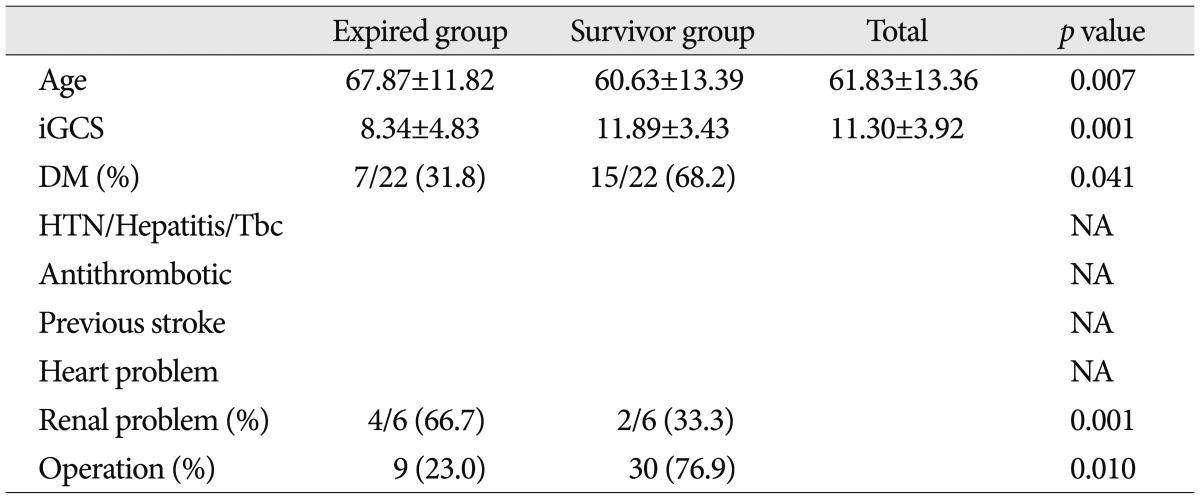
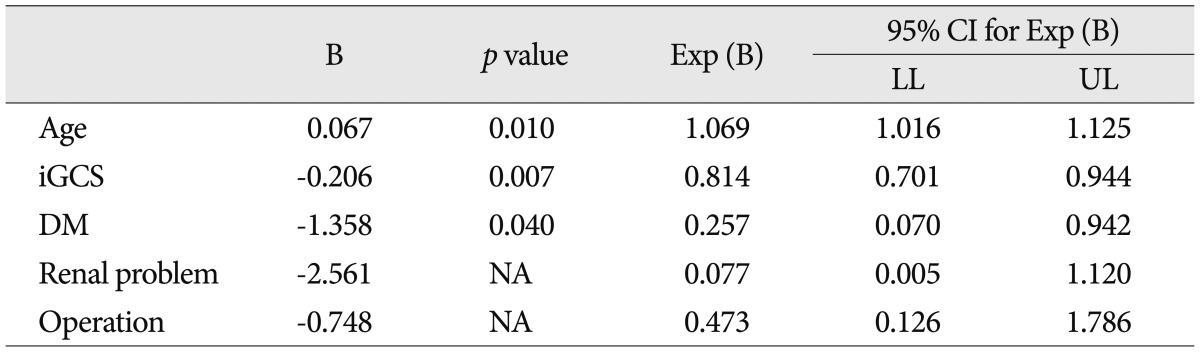
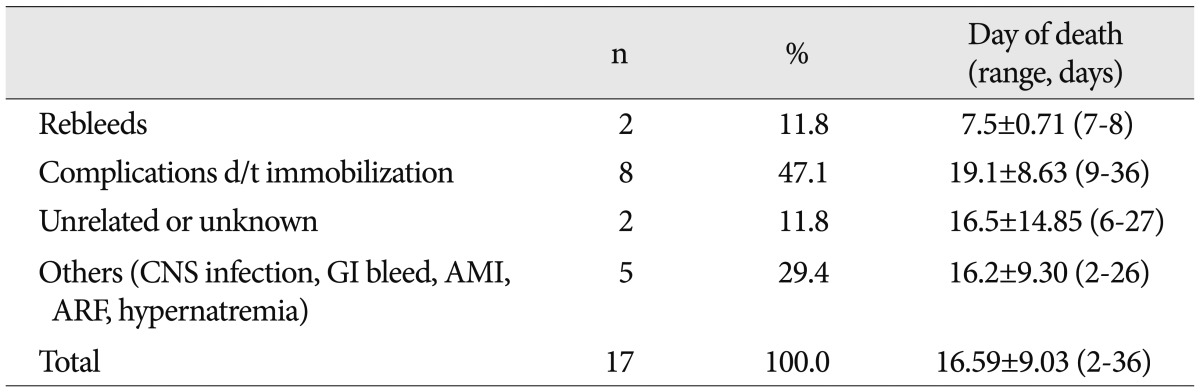
All 174 patients were enrolled in this study. There were 92 males and 82 females (mean age±SD : 61.83±13.36 years, range 28-90). According to the location of hemorrhage, basal ganglia was the most common site in 83 cases, and thalamus was the second in 40 cases. Among them, 29 patients (16.7%) died during hospitalization. Case fatality was the highest for pontine hemorrhage (40%, 6/15), followed by cerebellar hemorrhage (25%, 3/12). The lowest case fatality rate was observed for subcortical white matter hemorrhage (4.2%, 1/24) ( Table 1). However, the location of the hematoma did not show a statistically significant difference. In univariate analysis, diabetes mellitus and previous renal problem and surgical operation of the hematoma showed an association with case fatality ( p<0.05); previous hypertension, hepatitis, tuberculosis, and heart problem did not show an association with case fatality. Previous stroke history and whether taking antithrombotics or not also did not influence the mortality ( Table 2). In multivariate analysis, age and diabetes mellitus and initial Glasgow Coma Scale (GCS) showed significant correlation with n-ICH related mortality ( Table 2, 3). In our study, the most common cause of death was initial neurological damage due to herniation of edematous brain tissue ( Table 4). In more than half of (58.6%, 17/29) mortality cases, the initial GCS was below eight points. However, the scores of the initial GCS of the remaining patients (41.4%, 12/29) were above eight points. This means that other factors could also influence mortality. After having survived the first few days by direct brain damage, patients may then develop various potentially fatal complications. In addition, findings of the current study showed that not only the initial neurological damage but also other factors influenced the case fatality of n-ICH. Seventeen patients (58.4%) died due to other factors, except initial neurological damage. Except for death due to the initial neurological sequelae, infection was the leading cause of death in eight cases (27.6%). One patient expired due to central nervous system infection due to ventriculitis after insertion of the external ventricular drainage system. Seven other patients expired due to hospital acquired infection in five cases, and aspiration pneumonia in two cases. Death due to early rebleeding was not a common cause in only two cases (6.9%, 2/29). Death due to acute myocardial infarction, acute renal failure, gastrointestinal bleeding, hypernatremia, and pulmonary thromboembolism occurred in one case each.
DISCUSSION
Systemic review of stroke incidence and case fatality in 56 population-based studies showed a moderate decrease in stroke incidence and a slight decrease in overall case fatality 9). However, it was still high and the 30-day case fatality rate with stroke (including ischemic and hemorrhagic stroke) was 14.3% (17-30%) 9). It was higher in primary intracerebral hemorrhage, compared to ischemic stroke (hemorrhagic stroke in 30-48%, ischemic stroke in 13-23%) 9). In the current study, the case fatality rate of n-ICH (16.7%, 29/174) was lower than that of the previous study. Our results showed that the direct effect of brain damage due to the massive hematoma appeared to be the most significant factor in n-ICH related death, similar to previous reports 3), and medical complication was the second cause of death. In this study, approximately half of patients (41.4%, 12/29) died due to the direct effect of the hematoma. However, reduction and prevention of death due to direct neurological sequelae is very difficult, because the extent of brain damage is determined at the moment of the bleeding points, so that the clinician could not influence that damage. Although the initial GCS was the most affecting factor of n-ICH related fatality, the remaining half of patients died due to other complications unrelated to hemorrhage. The problem is that a large number of people die due to other causes without direct neurological damage. Having survived the first few days, patients may then develop various potentially fatal complications, the most common being pneumonia and pulmonary embolism. Findings of this study showed that 15 patients died due to non-hemorrhagic related complications. The most common cause of death was infection in eight cases. Central nervous system infection occurred in one case and the remaining seven cases were due to hospital acquired pneumonia in five and aspiration pneumonia in two. Acute myocardial infarction, acute renal failure, gastrointestinal bleeding, electrolyte imbalance, and pulmonary embolism occurred in one case each. The main cause of death was pneumonia. Bacterial pneumonia, mainly caused by aspiration 10), is known as one of the most important complications in stroke patients 16), and is the major influencing factor in clinical outcomes. Aspiration is frequently observed in patients with reduced consciousness and in those with swallowing disturbances. Reflux of liquid feed, hypostasis, diminished cough, and immobilization increase the risk. Not only aspiration pneumonia but many other complications related to immobility also occurred (deep venous thrombosis, skin breakdown, contracture formation, and constipation) 13). In this situation, the precipitating factors of the non-neurological related complications were reclassified. Immobilization related complications were the most common in eight cases (pneumonia in seven cases, pulmonary thromboembolism in one case). Immobilization related case fatality was the largest proportion (47.1%, 8/17) of causes of death, except death due to initial direct neurological damage, indicating that immobilization was more likely to lead to complications ( Table 5). In addition, frequent changes of the patient's position in bed and pulmonary physical therapy may prevent pneumonia 8), and increasing the patient's chest motion and early ambulation with adequate antibiotics is very important to treatment of pneumonia. However, due to the risk of rebleeding and the lack of clarity with regard to optimal timing of the first mobilization, the decision of whether to start early ambulation or not in patients with n-ICH is difficult. In addition, due to the risk of rebleeding, most physicians are hesitant regarding early ambulation of patients. Among 202 professionals interviewed, 60% were not in favor of mobilization within 24 hours of stroke onset 15). In our institution also, the gait of patients with n-ICH is started after a minimum of one week or more of bed rest. However, it is questionable that early ambulation was related to increased rebleeding. Serial CT scan in patients with hypertensive hemorrhage showed that the hemorrhage was enlarged in the first six hours after presentation in a subset of patients 1,5,6). In a prospective series, significant hematoma growth occurred over the first 24 hours in 38% of patients 6). There has been no report indicating that early ambulation increases rebleeding in n-ICH patients. In other words, permitting ambulation at 24 hours after the ictus in patients without related risk factors of rebleeding such as antithrombotic therapy, sustained elevated blood pressure, large hematoma size, and evidence of contrast extravasation on initial CT imaging 1,14) is relatively safe. In addition, some authors have reported that mobilization within the first few days appears to be well tolerated 7). Preliminary results from the ongoing A Very Early Rehabilitation Trial for Stroke study of rehabilitation within 24 h suggest that immediate physical therapy is well tolerated with no increase in occurrence of adverse events 4).
CONCLUSION
Mortality of n-ICH is decreasing, but still high. The inevitable initial brain damage is the leading cause of death; however, the non-neurological damage that is possible for prevention and reduction with clinicians' efforts will occupy a large portion. Most cases of death of patients who survived from the first hemorrhagic sequelae were due to immobilization related complications (in particular, pneumonia and pulmonary embolism). These findings indicated that early ambulation in n-ICH patients should be encouraged in order to prevent such complications and mortality. In addition, conduct of a further prospective randomized study will be necessary in order to provide the benefit of early mobilization for prevention of immobilization related complications.
Acknowledgements
This research was supported by a grant of Yeungnam University Research Grant 2013.
References
1. Balami JS, Buchan AM : Complications of intracerebral haemorrhage. Lancet Neurol 2012, 11 : 101-118,   2. Balami JS, Chen RL, Grunwald IQ, Buchan AM : Neurological complications of acute ischaemic stroke. Lancet Neurol 2011, 10 : 357-371,   3. Bamford J, Dennis M, Sandercock P, Burn J, Warlow C : The frequency, causes and timing of death within 30 days of a first stroke : the Oxfordshire Community Stroke Project. J Neurol Neurosurg Psychiatry 1990, 53 : 824-829,    4. Bernhardt J, Dewey H, Thrift A, Donnan G : Inactive and alone : physical activity within the first 14 days of acute stroke unit care. Stroke 2004, 35 : 1005-1009,   5. Broderick JP, Brott TG, Tomsick T, Barsan W, Spilker J : Ultra-early evaluation of intracerebral hemorrhage. J Neurosurg 1990, 72 : 195-199,   6. Brott T, Broderick J, Kothari R, Barsan W, Tomsick T, Sauerbeck L, et al : Early hemorrhage growth in patients with intracerebral hemorrhage. Stroke 1997, 28 : 1-5,   7. Diserens K, Michel P, Bogousslavsky J : Early mobilisation after stroke : review of the literature. Cerebrovasc Dis 2006, 22 : 183-190,   8. European Stroke Organisation (ESO) Executive CommitteeGuidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis 2008, 25 : 457-507,   9. Feigin VL, Lawes CM, Bennett DA, Barker-Collo SL, Parag V : Worldwide stroke incidence and early case fatality reported in 56 population-based studies : a systematic review. Lancet Neurol 2009, 8 : 355-369,   10. Horner J, Massey EW, Riski JE, Lathrop DL, Chase KN : Aspiration following stroke : clinical correlates and outcome. Neurology 1988, 38 : 1359-1362,   11. Julian RY, Richard WH : Youmans Neurological Surgery. ed 6. Philadelphia : Saunders/Elsevier, 2011
12. Kumar S, Selim MH, Caplan LR : Medical complications after stroke. Lancet Neurol 2010, 9 : 105-118,   13. Langhorne P, Stott DJ, Robertson L, MacDonald J, Jones L, McAlpine C, et al : Medical complications after stroke : a multicenter study. Stroke 2000, 31 : 1223-1229,   14. Park SY, Kong MH, Kim JH, Kang DS, Song KY, Huh SK : Role of 'spot sign' on CT angiography to predict hematoma expansion in spontaneous intracerebral hemorrhage. J Korean Neurosurg Soc 2010, 48 : 399-405,    15. Sjöholm A, Skarin M, Linden T, Bernhardt J : Does evidence really matter? Professionals' opinions on the practice of early mobilization after stroke. J Multidiscip Healthc 2011, 4 : 367-376,   16. Weimar C, Roth MP, Zillessen G, Glahn J, Wimmer ML, Busse O, et al : Complications following acute ischemic stroke. Eur Neurol 2002, 48 : 133-140,  
Table 1
Patients' profiles and location of the hemorrhage 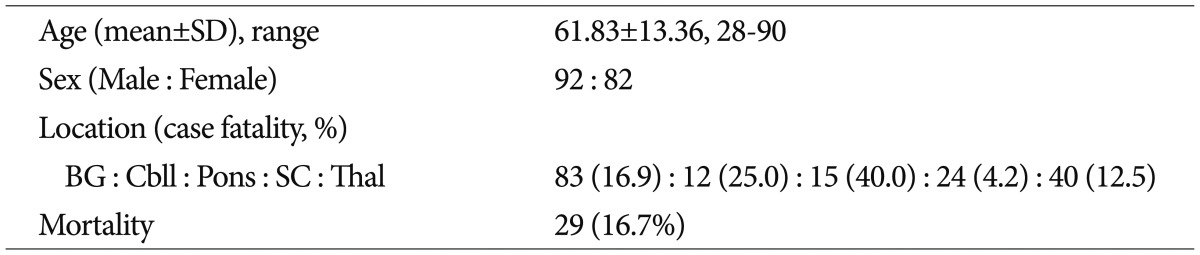
Table 2
Risk factors of case fatality (univariate analysis) 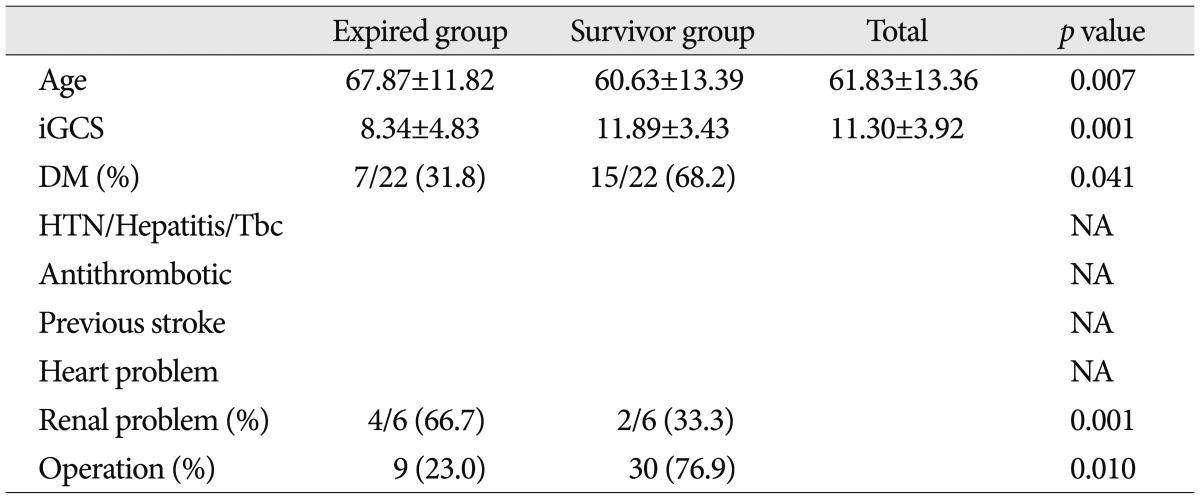
Table 3
Risk factors of case fatality (multivariate analysis) 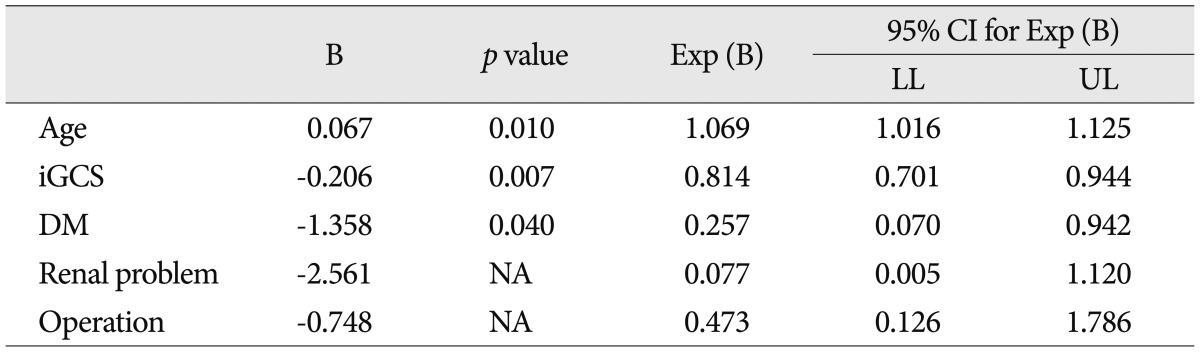
Table 4
Cause of death due to nonlesional intracerebral hemorrhage 
Table 5
Cause of death due to nonlesional intracerebral hemorrhage except direct neurological sequelae 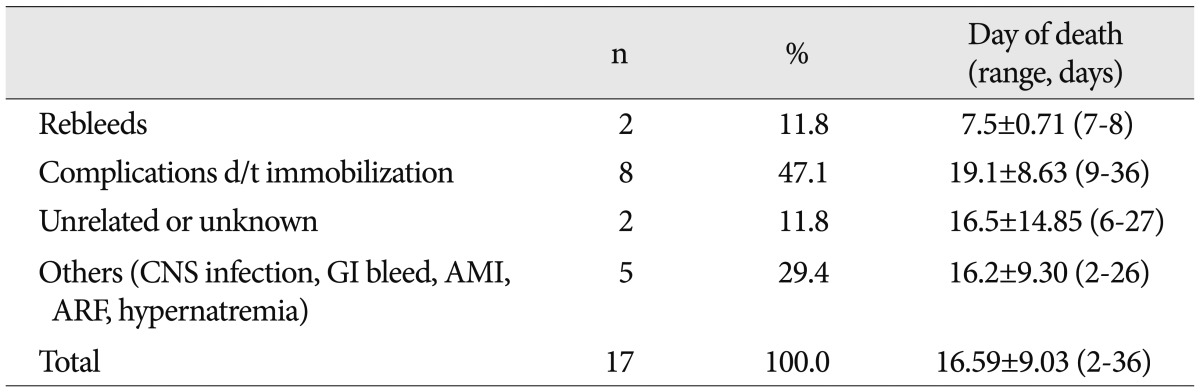
|
|