Kim and Kim: Anterior Cervical Discectomy and Fusion Using a Double Cylindrical Cage versus an Anterior Cervical Plating System with Iliac Crest Autografts for the Treatment of Cervical Degenerative Disc Disease
Abstract
Objective
Anterior cervical discectomy and fusion (ACDF) is often complicated by subsidence, pseudoarthrosis, kyphosis, and graft donor site morbidities. To decrease the occurrence of these complications, various types of cages have been developed. We designed this retrospective study to analyze and compare the efficacy and outcomes of ACDF using double cylindrical cages (DCC) (BK Medical, Seoul, Korea) versus an anterior cervical plating system with autogenous iliac crest grafts.
Methods
Forty-eight patients were treated with autograft and plating (plate group), and 48 with DCC group from October 2007 to October 2011. We analyzed construct length, cervical lordotic curvarture, the thickness of the prevertebral soft tissue, segmental instability, and clinical outcomes.
Results
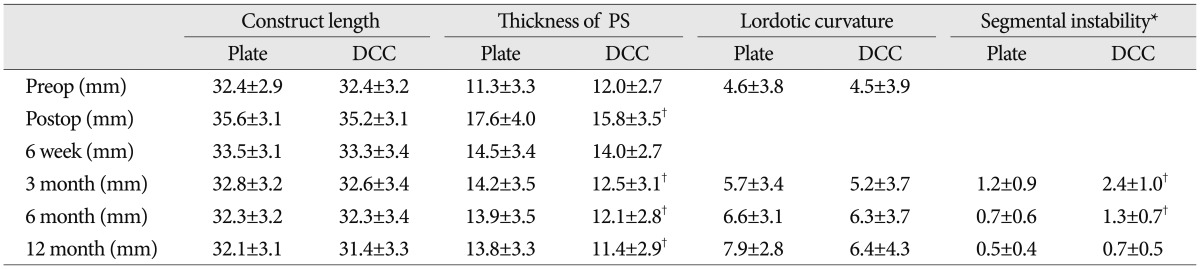
There were no significant differences between the two groups with regard to the decrease in construct length or cervical lodortic curvature at the 3-, 6-, and 12-month follow-ups. The prevertebral soft tissue was thinner in the DCC group than the plate group immediately after surgery and at the 3-, 6-, and 12-month follow-ups. The difference in interspinous distance on flexion-extension was shorter in the plate group than the DCC group at the 3- and 6-month follow-ups. However, there was no significant difference in this distance between the two groups at the 12-month follow-up.
Conclusion
A double cylindrical cage is a good alternative for fusion in patients with cervical degenerative diseases; the surgical method is relatively simple, allows good synostosis, has less associated prevertebral soft tissue swelling, and complications associated with autografting can be avoided.
Key Words: Cylindrical cage · ACDF · Subsidence · Fusion.
INTRODUCTION
Anterior cervical discectomy and fusion (ACDF) is a widely accepted surgical procedure for the treatment of cervical spinal degenerative disease 2,3,12,13). This procedure is used to decompress the spinal cord and nerve roots, stabilize the affected segments, and provide solid arthrodesis. Several technical modifications of this procedure have been developed, but there is currently no consensus regarding the optimal technique 7). Unfortunately, this procedure is often complicated by collapse of the graft bone, pseudoarthrosis, kyphotic deformity, and especially, graft donor site morbidities 1,4,7) such as prolonged donor site pain, hematomas, infection, nerve injury, and iliac crest fracture or deformity 12,19,20). In addition, plate fixation has the drawbacks of high cost, a long operative time, and risk to adjacent structures because of the retraction required for plate insertion 21). To decrease the occurrence of these complications, various types of cages have been developed and are currently being used 10,12,22). However, among those cages, cylindrical cages are underused because they are thought to have a tendency to subside, though this has not been conclusively shown 8,19). We designed this retrospective study to analyze and compare the efficacy and outcomes of anterior cervical fusion using a double cylindrical cage (DCC) (BK Medical, Seoul, Korea) ( Fig. 1) or autogenous iliac crest grafts and an anterior cervical plating system.
MATERIALS AND METHODS
This retrospective study was conducted with the approval of the medical ethics review board at our institution.
Patient population
We performed a retrospective study of patients who underwent one level ACDF by one of two different methods. The same surgeon performed all procedures. Forty-eight patients were treated with autograft and plating (plate group) and 48 with DCC group from October 2007 to October 2011. All patients initially presented with cervical radiculopathy and concordant soft disc herniation that persisted despite conservative management. Patients with confounding variables (required more than two level ACDF, previous cervical spine surgery, additional posterior decompression, trauma, or tumor) or those for who imaging data were unavailable were not included in the study.
The demographic and clinical data of the two groups were comparable ( Table 1). There were 25 males and 23 females aged between 24 years and 80 years (mean 51.2 years) in the DCC group. In the autograft and plating group, there were 24 males and 24 females who ranged in age from 19 years to 70 years (mean 46.5 years). The levels of anterior segmental cervical fusion are shown in Table 1, and the most common cervical level involved was C5-6 in both groups. The clinical manifestations included neck pain, cervical radiculopathy, and myelopathy, all of which were refractory to conservative treatment measures. Eleven (22.9%) patients in the plate group and 10 (20.8%) in the DCC group suffered from concurrent myelopathy and radiculopathy. Odom's criteria ( Table 2) were used to assess clinical outcomes.
Surgical procedure
All the operations were performed by one surgeon. A standard anterior approach to the cervical spine was used in all patients. The basic technique used for exposure, discectomy, and decompression was the Robinson and Smith technique, and this technique was performed using a right-sided skin incision.
A microscope was used in all cases during the discectomy procedure. Endplates were prepared for fusion by drilling. The bony endplate was preserved as much as possible to prevent cage subsidence. In all instances, the posterior longitudinal ligament was opened and possible osteophytes compressing the nerve root were removed with Kerrison punches or drills, and adequate exposure and decompression of the dura mater and nerve root origins were obtained.
In the DCC group, double cylindrical cages (8, 9, 10 mm ø, BK Medical, Seoul, Korea), packed with reamed bone and Orthoblast II (IsoTis Orthobiologics, Irvine, CA, USA) were placed on either side by turning the implant inserter clockwise and applying a light pressure.
In the autograft and plating group, anterior plating was performed using the Smith-Robinson technique; tricortical autologous iliac bone was harvested from the iliac crest and grafted between the vertebral bodies under traction. Supplemental anterior plate fixation was performed using the Atlantis plate system of hybrid construct in which inferior (fixed-angled) screw act as buttress while variable-angle (superior) screws rotate at the plate-screw interface (Medtronic Sofamor Danek, Minneapolis, MN, USA).
A soft collar was prescribed for 12 weeks postoperatively in both groups.
Radiologic evaluation
MRI scans were obtained before surgery and anteroposterior and lateral plain radiographs including dynamic views were obtained before surgery, immediately after surgery, at 6 weeks, 3 months, 6 months, and 12 months after surgery.
The construct length was measured as the distance between the middle margin of the upper end plate of the upper vertebra and the middle margin of the lower end plate of the lower vertebra ( Fig. 2A). Subsidence was defined as ≥3 mm reduction in the construct length between immediately after surgery and the 6-week follow-up. Cervical spinal curvature was measured by the method of Profeta et al. 18) ( Fig. 2B). A straight line was drawn from the posterior border of the dens to the posterior-inferior border of C7. Another line was drawn from the posterior-inferior border of C4 perpendicular to the first line, whose intersected length was measured in millimeters as the degree of spinal curvature, with a length of 0 mm corresponding to straight lateral spine curvature. Negative values denoted kyphotic spine curvature and positive values lordotic spine curvature. The thickness of the prevertebral soft tissue was measured as the distance between the soft tissue shadow and the anterior margin of the lower endplate of the caudal vertebra ( Fig. 2C). Nonunion was defined as the appearance of segmental instability with ≥2 mm widening of the interspinous distance on flexionextension lateral views at the last follow-up ( Fig. 2D). In addition, radiolucency >50% over the anteroposterior distance of the interface between the endplates and implants was defined as nonunion.
RESULTS
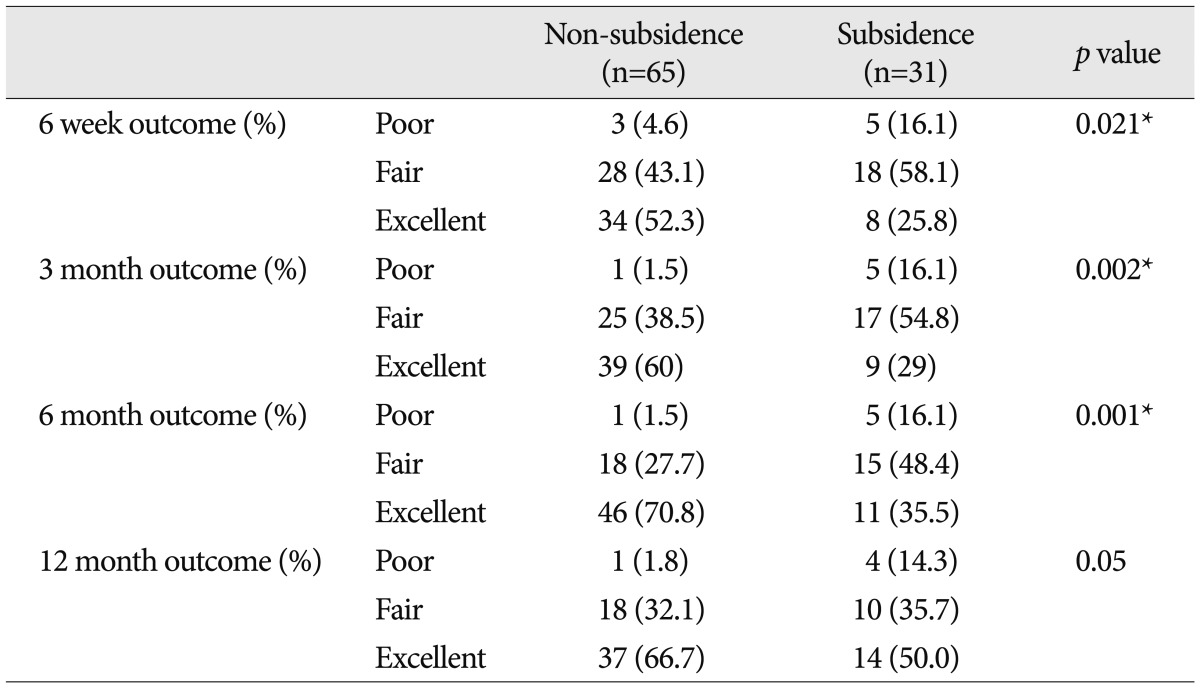
The construct length was not statistically different between two groups on the first day, 6 weeks, 3, 6, or 12 months post-operatively. The prevertebral soft tissue was significantly thinner in the DCC group than in the plate group on the first day and 3, 6, and 12 months post-operatively. Clinically, one patient in each group developed postoperative dysphagia, but both patients recovered in 1 month. There was a trend towards increased lordotic curvature over time at 3, 6, and 12 months in both groups without any significant difference between the groups. The difference in the interspinous distance at flexion and extension, reflecting segmental instability, was significantly smaller in the plate group than in the DCC group at 3 and 6 months postoperatively, but no difference at 12 months ( Table 3). In each group, nonunion was observed in one patient. Clinical outcomes were significantly more favorable in the DCC group at the follow-up assessment 6 weeks after surgery, but not at 3, 6, and 12 months postoperatively ( Table 4). The incidence of subsidence was lower in the DCC group than in the plate group (27.1% vs. 37.5% respectively), but this difference was not statistically significant ( Table 5). Furthermore, the existence of subsidence was significantly associated with more unfavorable clinical outcomes at all follow-up assessments ( Table 6). Postoperative complications such as hematoma revision, hoarseness, infection, and dysphagia were observed in both groups, but were not fatal and patients healed in about 3 months. Furthermore, there were no significant differences in the incidence of postoperative complications between the two groups (p=0.294).
DISCUSSION
Stand-alone interbody cages can be inserted using a simple surgical technique and there is less damage to adjacent structures as there is no need for retraction, which is required for plate insertion. Furthermore, insertion of stand-alone interbody cages requires a shorter operating time and there is less blood loss than plate insertion 4,6). A biomechanical study demonstrated that stand-alone cages provide adequate resistance to pullout and migration without anterior or posterior cervical fixation 20). An ideal stand-alone interbody cage for ACDF would have to provide immediate postoperative stability, maintain disc height and cervical lordosis, achieve a solid fusion, and avoid complications due to the use of autogenous or allogenous bone grafts 17). However, the exact relationships among cage subsidence, malalignment, fusion rate, and clinical outcomes remain unclear 5), and the optimal shape and material type for stand-alone cage procedures are highly debated, as is the utility of the stand-alone cage itself 13,15).
Subsidence
Although many types of cervical single cages have been developed and used, postoperative subsidence is commonly reported.
Single cylindrical cages are widely used worldwide. However, these are larger in size than double cylindrical cages and have to be inserted at the center, which is a vulnerable area. Therefore, complications such as subsidence occur frequently, which has led to decreased use of these cages.
Because the cylindrical cage has to be drilled into the intervertebral space, this procedure is destructive to the endplates, leaving them far from intact. The contact surface between the cage and osseous bony part of the endplate is reduced as a result of both endplate preparation and the cylindrical shape of the cage 12). The contact surface between the cage and the vertebral body, and the anterior intraoperative distraction have been confirmed to be risk factors for cage subsidence 22). Authors emphasized that double cylindrical cages address many of the issues associated with single cages; they are smaller in size and have a larger contact surface together with endplates, and are inserted into both foramen nervosum, resulting in less subsidence and a greater probability of symptom improvement in foraminotomy procedures 5). In our study, interestingly, the incidence of subsidence was lower in the DCC group than in the plate group (27.1% vs. 37.5%, respectively), without statistical significance.
Fusion rate
Advantages of a solid fusion include a reduction in potential instability, preservation of disc height, maintenance of alignment, and protection of the size of the neural foramen.
Wang et al. 20) found that the porous wall of the cylindrical cage allowed ingrowth of the surrounding bone of the adjacent vertebrae, and previous animal studies have suggested that the cavernous wall promotes bone fusion. In this series, the fusion rate reached 100% at one year. Our findings were similar. Another study showed that fusion time was significantly delayed, and that the fusion rate was significantly lower when ACDF was performed using a cage in comparison to a plate 6). However, we found that although the fusion time was significantly delayed in the DCC group until 6 months after the operation, there were no significant differences between the plate and cage groups at 12 months. This delay in fusion in the DCC group implies the lack of a strong fixation force in this group, allowing postoperative micromotions to occur continuously between the contact surface of the cage and the vertebral body.
Cervical lordosis
Theoretically, the loss of lordosis increases biomechanical stress on the anterior vertebral elements in neighboring segments 16). Therefore, the long-term success of spinal surgery appears to be dependent on the maintenance of cervical lordotic curvature. Martins 14) classified spine alignment as excellent if lordosis was preserved, good if there was a loss of <5°, and fair and poor when kyphosis was >5°. In our study, excellent or good alignment was achieved in most patients (100% in the plate group, 97.9% in the DCC, p=0.420), and this good alignment was maintained or improved up to 12 months postoperatively.
According to Kolstad et al. 12), insertion of a cage improved the curvature toward lordosis, but at 12 months postoperatively, this effect was lost and there was even more degeneration to kyphosis than observed before surgery. However, in other studies 9,18), better alignment was obtained by ACDF with a cylindrical cage than ACDF with allografts or autografts, which might have contributed to the lower incidence of ASD.
Prevertebral soft tissue swelling
Prevertebral soft tissue swelling is frequently implicated as a cause of postoperative dysphagia, but quantitative analysis of postoperative swelling after ACDF is not often performed.
In our study, the prevertebral soft tissue was significantly thinner in the DCC group than in the plate group at the first day and 3, 6, and 12 months post-operatively. Anterior plating may be responsible for the higher rates of dysphagia reported in contemporary series because of the plate's mass effect on the adjacent esophagus and because contralateral screw placement requires more retraction past the midline than is necessary when a plate is not used 11). Cylindrical cages are inserted by torque, unlike rectangular cages that require the impact of a surgical hammer for insertion, and do not affect the cervical cord at all, making them easy to insert. Furthermore, partial invasion of the vertebral body surface can decrease the risk of cage displacement immediately after the operation.
Unfortunately, we do not have long-term radiologic or clinical data, an obvious weakness of this study. Therefore, long-term follow-up studies are necessary, and we plan to conduct these in the future. Another weakness of this study is that it is retrospective. To address this weakness, a prospective randomized study should be performed.
CONCLUSION
Double cylindrical cages relatively showed no tendency of decreasing construct length when used for anterior cervical fixation compared to use of a plating system and iliac crest autografts. Even though fusion was delayed when a DCC was used, there was no difference in the nonunion rate at 12 month between the DCC and plate patient groups. Furthermore, the prevertebral soft tissue was significantly thinner in the DCC group than in the plate group, and most patients in both groups achieved excellent or good alignment. Double cylindrical cages is one of good alternatives for fusion in patients with cervical degenerative diseases; the surgical method is relatively simple and less invasive than the plate method, allows good synostosis, maintains or improves cervical lordotic curvature, causes less prevertebral soft tissue swelling than the plate method, and avoids many of the complications associated with autografting.
References
1. Banwart JC, Asher MA, Hassanein RS : Iliac crest bone graft harvest donor site morbidity. A statistical evaluation. Spine (Phila Pa 1976) 1995, 20 : 1055-1060,   2. Bohlman HH, Emery SE, Goodfellow DB, Jones PK : Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am 1993, 75 : 1298-1307,   3. Connolly PJ, Esses SI, Kostuik JP : Anterior cervical fusion : outcome analysis of patients fused with and without anterior cervical plates. J Spinal Disord 1996, 9 : 202-206,   4. Fujibayashi S, Neo M, Nakamura T : Stand-alone interbody cage versus anterior cervical plate for treatment of cervical disc herniation : sequential changes in cage subsidence. J Clin Neurosci 2008, 15 : 1017-1022,   5. Hauerberg J, Kosteljanetz M, Bøge-Rasmussen T, Dons K, Gideon P, Springborg JB, et al : Anterior cervical discectomy with or without fusion with ray titanium cage : a prospective randomized clinical study. Spine (Phila Pa 1976) 2008, 33 : 458-464,   6. Hermansen A, Hedlund R, Vavruch L, Peolsson A : A comparison between the carbon fiber cage and the cloward procedure in cervical spine surgery : a ten- to thirteen-year follow-up of a prospective randomized study. Spine (Phila Pa 1976) 2011, 36 : 919-925,   7. Hida K, Iwasaki Y, Yano S, Akino M, Seki T : Long-term follow-up results in patients with cervical disk disease treated by cervical anterior fusion using titanium cage implants. Neurol Med Chir (Tokyo) 2008, 48 : 440-446; discussion 446,   8. Joung YI, Oh SH, Ko Y, Yi HJ, Lee SK : Subsidence of cylindrical cage (AMSLUtrade mark Cage) : postoperative 1 year follow-up of the cervical anterior interbody fusion. J Korean Neurosurg Soc 2007, 42 : 367-370,    9. Kao FC, Niu CC, Chen LH, Lai PL, Chen WJ : Maintenance of interbody space in one- and two-level anterior cervical interbody fusion : comparison of the effectiveness of autograft, allograft, and cage. Clin Orthop Relat Res 2005, ( 430):108-116,   10. Kast E, Derakhshani S, Bothmann M, Oberle J : Subsidence after anterior cervical inter-body fusion. A randomized prospective clinical trial. Neurosurg Rev 2009, 32 : 207-214; discussion 214,   11. Kepler CK, Rihn JA, Bennett JD, Anderson DG, Vaccaro AR, Albert TJ, et al : Dysphagia and soft-tissue swelling after anterior cervical surgery : a radiographic analysis. Spine J 2012, 12 : 639-644,   12. Kolstad F, Nygaard ØP, Andresen H, Leivseth G : Anterior cervical arthrodesis using a "stand alone" cylindrical titanium cage : prospective analysis of radiographic parameters. Spine (Phila Pa 1976) 2010, 35 : 1545-1550,   13. Lind BI, Zoega B, Rosén H : Autograft versus interbody fusion cage without plate fixation in the cervical spine : a randomized clinical study using radiostereometry. Eur Spine J 2007, 16 : 1251-1256,    14. Martins AN : Anterior cervical discectomy with and without interbody bone graft. J Neurosurg 1976, 44 : 290-295,   15. Matgé G : Cervical cage fusion with 5 different implants : 250 cases. Acta Neurochir (Wien) 2002, 144 : 539-549; discussion 550,   16. Matsunaga S, Kabayama S, Yamamoto T, Yone K, Sakou T, Nakanishi K : Strain on intervertebral discs after anterior cervical decompression and fusion. Spine (Phila Pa 1976) 1999, 24 : 670-675,   17. Niu CC, Liao JC, Chen WJ, Chen LH : Outcomes of interbody fusion cages used in 1 and 2-levels anterior cervical discectomy and fusion : titanium cages versus polyetheretherketone (PEEK) cages. J Spinal Disord Tech 2010, 23 : 310-316,   18. Profeta G, de Falco R, Ianniciello G, Profeta L, Cigliano A, Raja AI : Preliminary experience with anterior cervical microdiscectomy and interbody titanium cage fusion (Novus CT-Ti) in patients with cervical disc disease. Surg Neurol 2000, 53 : 417-426,   19. Sugawara T, Itoh Y, Hirano Y, Higashiyama N, Mizoi K : Long term outcome and adjacent disc degeneration after anterior cervical discectomy and fusion with titanium cylindrical cages. Acta Neurochir (Wien) 2009, 151 : 303-309; discussion 309,   20. Wang X, Chen Y, Chen D, Yuan W, Chen X, Zhou X, et al : Anterior decompression and interbody fusion with BAK/C for cervical disc degenerative disorders. J Spinal Disord Tech 2009, 22 : 240-245,   21. Whitecloud TS 3rd : Modern alternatives and techniques for one-level discectomy and fusion. Clin Orthop Relat Res 1999, ( 359):67-76,   22. Yang JJ, Yu CH, Chang BS, Yeom JS, Lee JH, Lee CK : Subsidence and nonunion after anterior cervical interbody fusion using a stand-alone polyetheretherketone (PEEK) cage. Clin Orthop Surg 2011, 3 : 16-23,   
Fig. 1
A : Double cylindrical cage (DCC). B : Intraoperative picture after cage placement. C and D : Anteroposterior and lateral radiographs following anterior cervical discectomy and fusion using DCC. 
Fig. 2
A : The construct length was measured as the distance between the middle margin of the upper end plate of the upper vertebra and the middle margin of the lower end plate of the lower vertebra. B : The lordotic curvature was measured by Profeta's method. C : The thickness of the prevertebral soft tissue was measured as the distance between the soft tissue shadow and the anterior margin of the lower endplate of the caudal vertebra. D : Segmental instability was measured as the difference of the interspinous distance on the flexion and extension radiographs. 
Table 1
The demographic and clinical data of the two groups 
Table 2

Table 3
Comparisons of the radiologic results between the plate group and the DCC group 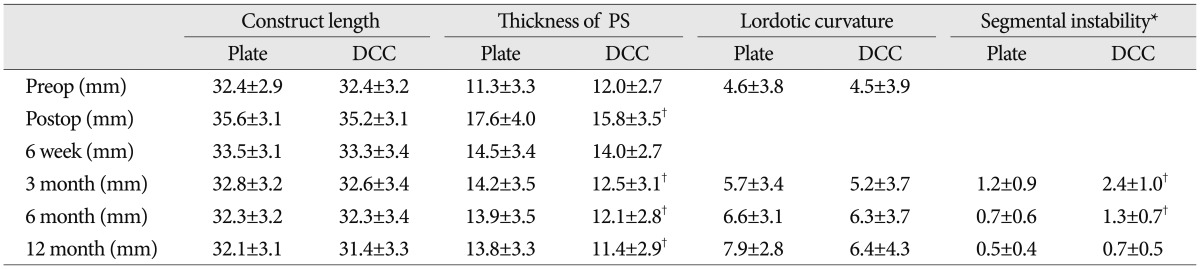
Table 4
Comparisons of clinical outcomes between the plate group and DCC group 
Table 5
Comparisons of the incidence of subsidence between plate group and DCC group 
Table 6
Comparisons of clinical outcomes between the subsidence group and non-subsidence group 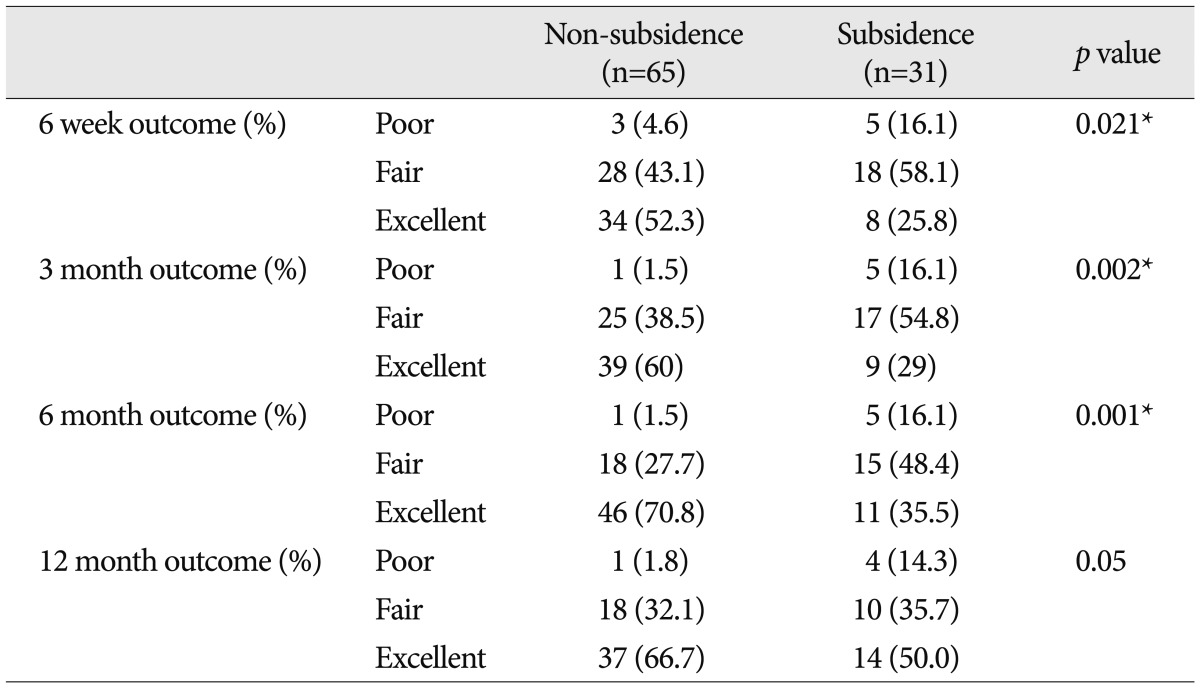
|
|