INTRODUCTION
Low-energy penetrating craniocerebral nail injury is extremely rare, and usually has a better outcome than a gunshot injury because of a more localized primary injury. The main aspects of treatment include detail assessment of vascular injury by imaging studies, followed by careful removal of the nail with hemorrhage control. However, penetrating craniocerebral nail injury accompanying by post-traumatic cerebral infarction (PTCI) can be fatal, and needs to be treated aggressively. Herein, we present the case of a 91-year-old male who had sustained PTCI following a low-energy penetrating craniocerebral injury due to a nail without evidence of hematoma.
CASE REPORT
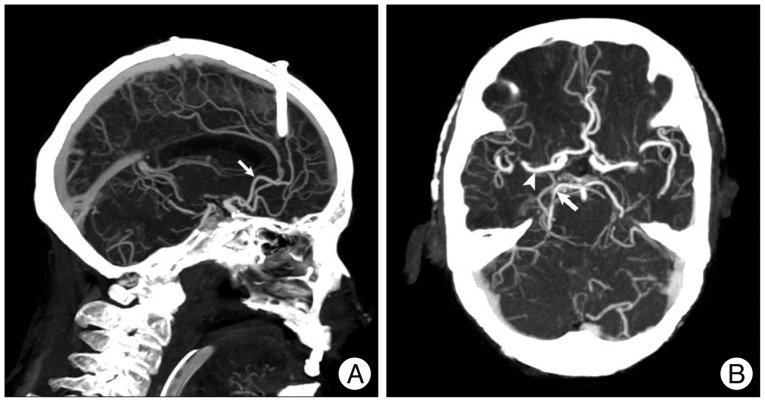
A 91-year-old male was brought to our emergency department because he hammered a nail into his head by himself 4 hours prior to admission. On arrival the patient was found to be unresponsive, with a pulse of 92 beats/min, a blood pressure of 160/95 mm Hg, and a Glasgow Coma Scale (GCS) score of 5. Physical examination disclosed a nail protruding 0.5 cm from the cranium in the right frontal region. The muscle power was grade 1/5 in the right upper and lower limbs with absent deep tendon reflex and grade 4/5 in the left upper and lower limbs. The plantar reflex was present in the left side. He was subsequently intubated. Non-contrast computed tomography (CT) of the brain disclosed an intact metallic nail measuring about 4.5 cm in length in the right frontal region, pneumocranium, and hypo-attenuation involving the right anterior cerebral artery (ACA), middle cerebral artery (MCA) (Fig. 1A, asterisk) and posterior cerebral artery area (PCA) (Fig. 1A, asterisk) without hematoma. The CT scan also revealed cerebral edema with effacement of sulci and homogeneously decreased attenuation with loss of the gray-white matter differentiation (arrows, Fig. 1B). CT angiography revealed intact right ACA (Fig. 2A, arrow), MCA (Fig. 2B, arrowhead), and PCA (Fig. 2B, arrow), without extravasation of contrast material or pseudoaneurysm. A diagnosis of PTCI was made, and a large right frontoparietal decompressive craniectomy close to the nail was done at operation room and followed with removal of the nail along its entry axis under direct vision. Severe brain swelling over the right hemisphere was found during surgery. Postoperatively, the patient was transferred to intensive care unit and received ceftriaxone 2 gm q12h and vancomycin 1 gm q12h intravenously. There was no fever during the hospitalization and the white blood cell count was 8690/uL at the time of discharge. The post-operative course was uneventful, and the patient was discharged on the 11th hospital day with a GCS of 5 and tracheostomy. The bone flap was not replaced at the time of discharge.
DISCUSSION
PTCI is a rare complication of severe traumatic brain injury, and is usually caused by blunt brain injury with intra- or extra-axial hematoma formation associated gross mechanical shift of the brain and herniation across the falx and/or tentorium9,11,15). The patient presented herein developed PTCI after a low-energy frontal penetrating craniocerebral injury caused by a nail without vascular injury or hematoma. He survived after decompressive craniectomy with permanent neurological deficit.
Low-energy penetrating craniocerebral nail injury is rare, and only a few cases that have been due to suicide attempts have been reported7,12,13,14). Unlike gunshot injuries in which skull fracture fragments can cause intra-cranial hemorrhage; intra-cranial hemorrhage is uncommon in the low-energy penetrating craniocerebral nail injuries. CT angiography can help to exclude vascular injury and pseudoaneurysm formation that would result in serious bleeding after removal of the nail. In most cases, extraction of the nail can be safely done by gentle traction with or without craniotomy, and serious hemorrhage is unusual7,10,13). Antibiotic treatment is generally recommended for preventing brain abscess in patients sustaining penetrating brain injuries. The prognosis of a penetrating craniocerebral nail injury is relative good in most of the cases reported in the literature because of the relative low damage caused by the small diameter of the nails7,12,13). However, the outcome may be catastrophic if the penetrating craniocerebral nail injury is complicated by PTCI, as in our case.
PTCI occurs as a complication of severe traumatic brain injury with an incidence ranging from 1.9 to 8%9,15). A variety of mechanism may account for PTCI, including direct vascular compression due to a focal mass effect from brain herniation and intra- or extra-axial hematoma, cerebral vasospasm, brain edema, thromboembolism, cerebrovascular injury, and systemic hypoperfusion9). Among these mechanisms, mechanical shift of the brain and herniation across the falx leading to compression of the cerebral artery account for the majority of PTCI cases9,11). Although penetrating brain injury is usually associated with vascular damage, no vascular injury was noted in the present case. We propose the mechanism of the PTCI in our patient that may be related to multiple factors. First, short-term distal artery spasm with decreased cerebral flow might have been induced by mechanical stimulation of the penetrating nail injury1) and undetected by angiography in the ER. Second, traumatic brain injury could have induced cerebral hypoperfusion which might have been mediated by endothelin-1 and its receptors as early as 2-4 hours after injury3). Third, global hypoxia could have been further exacerbated by increased diffusion barriers8) and respiratory depression with hypoxia. Fourth, previous study has demonstrated that cytotoxic brain edema is caused by metabolic disturbances and occurs rapidly following traumatic brain injury2). Although the brain edema in our patient clearly did not compress ipsilateral cerebral arteries but brain edema resulted in elevated intracranial pressure leading to vascular hypoperfusion and subsequent ischemic cerebral damage.
The overall mortality rate of PTCI is high, ranging from 21 to 75%, and reaches close to 100% if the territory of the MCA is involved5,11,15). The territories of the PCA and MCA are the most commonly involved, and in 55% of patients with PTCI more than one vascular territory is involved9,11,15). The infarction areas in the present case involved the right-side territories of the ACA, MCA, and PCA, and this was expected to carry a grave prognosis. This case revealed that early decompressive craniectomy may relieve devastating brain edema.
Decompressive craniectomy has been considered a "rescue" therapy for traumatic brain injury with unilateral hemispheric edema4), which can immediately reduce increased intracranial pressure and decrease the subsequent cumulative ischemic burden16). Although the optimal time to perform decompressive craniectomy for traumatic brain edema is still in debate, previous studies have shown that early decompressive craniectomy improved functional outcome and survival rate4,6). Because PTCI with large infarctions is associated with a poor clinical outcome, we believe that decompressive craniectomy, not only simple extraction of the penetrating nail, should be performed as soon as possible to alleviate the profound brain edema10,13).
CONCLUSION
We reported the first case of hemi-cranial cerebral infarction due to a low-energy frontal penetrating craniocerebral nail injury. Clinicians should have a high index of suspicion for this catastrophic complication in cases of penetrating craniocerebral nail injuries. Decompressive craniectomy should be considered, rather than simple nail extraction, to relieve intracranial hypertension and cerebral hypoperfusion in case of extensive PTCI.