INTRODUCTION
Lumbar spinal stenosis (LSS) is a common cause of low back pain and lower extremity pain in older adults. The characteristic clinical manifestations of LSS include periodic exacerbations of low back and leg pain and neurogenic claudication, with resulting compromise in health-related quality of life, mobility, and independence24).
The optimal treatment strategy for LSS has not yet been defined. Non-operative treatments including restriction of activity, posture modification, and epidural steroid injections are useful for LSS symptoms of mild-to-moderate severity. Decompressive surgery is indicated for severe degree stenosis with neurogenic claudication, neural structure compromise, and/or intractable radicular symptoms.
Although conventional laminectomy is the standard option of neural structure decompression, it can cause instability12) and result in a less favorable outcomes at long-term follow-up21). Various technical modifications of the standard laminectomy have been reported in an attempt to adequately treat patients with spinal stenosis while maximizing the structural preservation of the spine4,6,8,11,16,19,22).
The purpose of this study was to present the author's surgical approach for decompression of LSS and to report early surgical results. This technique, which the author named central decompressive laminoplasty (CDL), involves undercutting the facet and upper lamina with maximal neural structure decompression and minimal resection of bony structures related to stability.
MATERIALS AND METHODS
The surgery was performed in 57 patients with LSS between 2006 and 2010. Clinical data were gathered retrospectively via electronic chart review. The surgical indication included LSS due to hypertrophy of the facet joint and ligamentum flavum. Spinal stenosis accompanied by a herniated disc was also included. All patients underwent relevant neurological and radiological examinations and pain was measured separately for the low back/buttock and the legs according to self-assessment on a 10-point visual analogue scale (VAS). Functional disability was assessed using the Oswestry Disability Index (ODI), which has been validated for Korean-language speakers10).
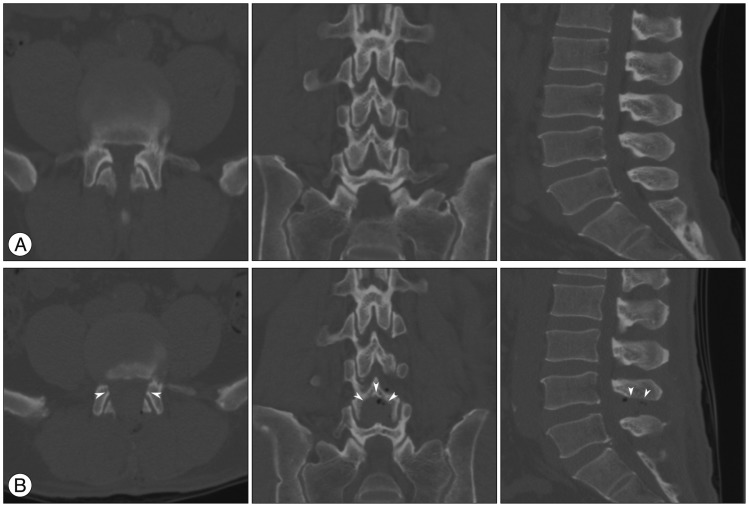
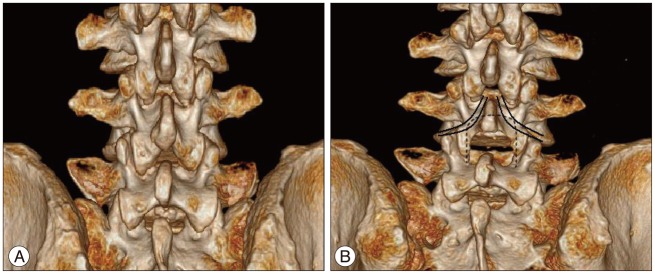
Preoperative lateral lumbar radiographs with flexion and extension views were taken of all patients to identify spondylolisthesis. The degree and level of stenosis were verified using magnetic resonance imaging (MRI) and/or computerized tomography (CT) with three-dimensional reconstruction. In cases with multiple lesions, symptomatic sites were determined by thorough neurological examination and incentive review of radiological findings to minimize surgical sites.
Perioperative clinical survey and X-rays were checked regularly. Follow-up was limited to six months, and the analysis of results was restricted to this early surgical period. Data were analyzed using the PASW Statistics 18.0 (IBM, Armonk, NY, USA). The paired samples t-test was used to test the difference between preoperative and 6-month postoperative values of VAS and ODI.
Surgical technique
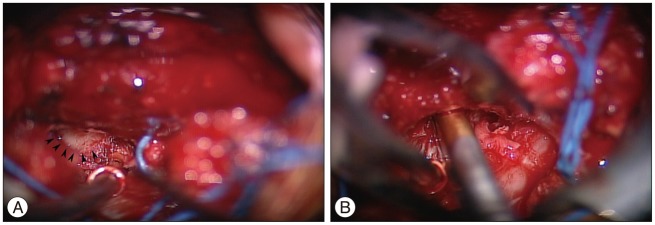
Under general anesthesia, patients were positioned on the Wilson frame, and correct position of the incision was verified using C-arm fluoroscopy. After a 3-cm midline skin incision, a small retractor was applied over the lumbar fascia. Sharp incision with a No. 10 blade was performed over the spinous process and down to the interspinous area. The sharp division and careful dissection of the ligaments from the spinous process enabled the functional closure of the supraspinous and interspinous ligaments when closing the fascia after the operation. Then bilateral dissection of the muscles was performed to expose the vertebral laminae at the stenotic level. Special care was taken when dissecting over the facet joint, so that the capsules were not violated. After retraction of dissected muscle bilaterally using a Caspar retractor, the inferior 1/4 to 1/3 of the spinous process of the cranial vertebra and the superior portion of the lamina in the caudal vertebra were removed with a bone rongeur. The spinolaminar junction of the cranial and caudal vertebrae then was drilled away with a cutting burr. The kyphotic prone positioning on elevated curvature of the frame or occasional use of interlaminar spreader enabled sufficient interlaminar working space for decompression by mobilizing the cranial lamina proximally and the caudal lamina distally (Fig. 1). Distraction was achieved by motion through the facet joints and disc.
A dissector was then used to mobilize the ligamentum flavum insertion from the inner surface of the cranial lamina. Soft tissue, including the ligament, was removed with a rongeur. The capsular portion of the ligamentum flavum was not disturbed to maintain facet joint stability. Dissected ligamentum flavum below the cranial lamina could be completely removed. Using a high-speed drill and spinal punches, undercutting of the inner surface of the cranial lamina was performed. Removal of the internal portion of the lamina extended to the proximal site of the ligamentum flavum insertion.
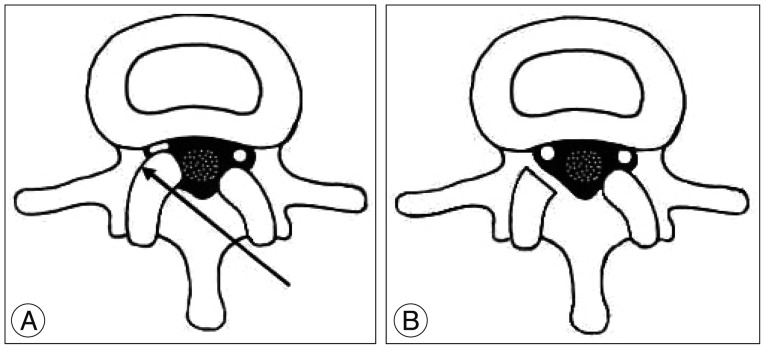
Decompression of nerve roots was performed with an operating microscope, starting from the side contralateral to the operator. The contra-lateral approach allows undercutting of the facet joint while decompressing the distal traversing root. Moreover, tilting the operative table down toward the opposite side provided the surgical view for decompression of proximal exiting root via undercutting of the upper lamina and removal of the tip of the hypertrophic superior articular process (Fig. 2). The medial facet was removed 10% to 20% in a tapered fashion, which allowed complete sparing of the capsule overlying the joint. Special care was taken when decompressing the traversing root. Complete decompression was performed along the pedicle to the lowermost part of the recess, at the turning point of the root into the foramen. Good exposure of the disc space was possible, and discectomy was performed when a soft herniated disc was identified. The divided supraspinous and interspinous ligaments were closed tightly after insertion of a drain onto the lamina. After subcutaneous tissue was stitched, the skin was taped with adhesive strips.
RESULTS
Operations were performed in 57 patients including 16 men and 41 women. Average age was 64.4 years (range, 46-87 years). All patients had limited functional ability due to back/buttock or leg symptoms despite prolonged conservative treatments including medication, physical therapy, and injection therapy. The symptoms were low back/buttock pain (81%), leg pain (68%), and neurologic claudication (53%). Symptom duration before surgery ranged from two months to 10 years. The L3-4 and L4-5 levels were most commonly involved in 22 (39%) and 45 (79%) cases, respectively. Thirty-seven patients underwent CDL for single level stenosis, 18 for two levels, and 2 for three levels. In 5 patients, discectomy was simultaneously performed at the same level as CDL. All patients responded well to the surgery and none required a revision procedure due to sustained or aggravated symptoms. No significant complications occurred except for a dural tear in six patients. After primary repair of the torn dura during the operation, all patients tolerated the procedure well.
The VAS scores and ODI were improved at six-month follow-up compared to preoperative levels. The mean VAS scores of back/buttock pain decreased significantly after operation (from 5.1±2.0 to 1.3±2.6, p<0.001). The mean VAS scores of leg pain also decreased significantly after operation (from 5.5±2.1 to 1.5±2.2, p<0.001). The mean ODI decreased significantly after operation (from 42.8±18.1 to 19.0±21.6, p<0.001). An excellent outcome, defined as over 75% improvement of initial VAS score of back/buttock pain and leg pain was observed in 75.0% and 76.2% of patients, respectively.
During the six-month follow-up, none of the patients showed significant symptomatic recurrence requiring revision surgery. One patient was treated by caudal epidural block due to leg pain. No patients developed aggravated instability on final plain radiography.
DISCUSSION
Decompressive laminectomy is a common technique for treatment of degenerative LSS. Despite wide variation across studies and little data from long-term follow-up, the outcome of the procedure has generally been reported as deteriorating over time13,14,18). Sufficient dural and root decompression accompanied by minimal resection of the facet joint provided good results in other series6,17). These results suggested that wide decompression with preservation of biomechanical stability, especially in the facet joint area, is required for long-term success of the decompressive procedure.
Unfortunately, under conventional total laminectomy, wide neural canal decompression may remove the pars interarticularis and necessitate significant resection of facet joints that provide spinal stability. Resection of excessive facet joints may also contribute to elevation of intradiscal pressure by establishing an alternate path of axial loading, transferring forces to the disc and longitudinal ligament7). Subsequently, disc degeneration may be accelerated, and further aggravation of disc disease or degenerative spondylolisthesis may occur.
Various technical modifications of lumbar laminectomy have been suggested to minimize the limitations of the procedure. These include bilateral laminotomy4,8) and unilateral laminotomy with bilateral decompression11,16,19). These modifications are intended to safeguard spinal stability by preserving the midline supporting structures, such as spinous processes and interspinous ligaments, while decompressing the central and lateral areas of the surgical level. Adequate decompression and its relation to a good surgical outcome have been reported5,9,20). These approaches do have some technical and theoretical limitations. The surgical corridor for access to the ipsilateral lateral recess and foraminal area is hindered, because the midline structures are not removed during decompression. Therefore, facet capsule violation and greater facet joint resection are needed to decompress the ipsilateral side of the lateral recess and neural foramen. As a result, these approaches may compromise stability and be harmful over the long-term. Additionally, access to the central area is restricted, making decompression difficult. During unilateral laminotomy with bilateral decompression, a narrow corridor to the opposite side of the lateral recess and foramen makes sufficient decompression difficult and requires significant thecal sac compression, which increases the possibility of neural injury and dural tear. To achieve sufficient decompression for the neural structures, this technique necessitates removal of critical bony structures, such as facet joints and capsules, while preserving structures less important to spinal stability (spinous processes and interspinous ligaments).
To overcome this limitation, a series of authors have performed specific modifications, which provide wide decompression while preserving facet stability by minimal bony resection. Two representative techniques were published as modifications of laminectomy. In 1981, Getty et al.6) performed a prototype of partial undercutting facetectomy for LSS to provide stability during nerve root decompression. A long-term, retrospective study of 57 patients who underwent the facet-sparing surgery was performed17). During a minimum five-year follow-up, 88% of patients maintained symptomatic improvement, and 72% had an excellent outcome with no leg pain at all at the final visit. In contrast, a prospective five-year follow-up study with conventional total laminectomy reported that the outcome was less favorable, showing 52% excellent outcome at final13). For a wider view during decompression, facet-undercutting methods have been modified with the additional lumbar spinous process splitting technique15,22,23). This technique provides sufficient working space for decompressive laminectomy by retracting the split spinous process. Because the paraspinal muscle is not detached from the spinous process, the muscle damage can be minimized. A randomized controlled study demonstrated that the splitting technique lessened postoperative back pain and prevented muscle atrophy compared with conventional laminectomy23).
In the present study, a modified laminectomy with facet joint preservation and wider decompression of neural structures was used to treat lumbar canal stenosis. The author named the procedure, "central decompressive laminoplasty" because decompression occurs in the central interspinous area and because the posterior arch of the lamina is spared while decompressing the internal hypertrophied area of the lamina and facet joint.
CDL offers two major technical strengths. One is near-total facet joint preservation including the capsule overlying the joint. The other is excellent surgical view and unhindered access to the central canal, lateral recess, and upper/lower foraminal area, providing thorough decompression of the neural element.
The facet joint and its capsule are key structures for spinal stability. Major structures that resist shear forces are the facet joints (33%) and discs (67%)2). While loaded in full flexion, simulated by combined bending and compression, approximately 70% of the bending moment is resisted by facet joint capsules and only 30% by discs3). Spine range of motion was not affected by the division of the supraspinous and interspinous ligaments1). During decompression with CDL, the lesion is approached from the contralateral side. Thus, inclined undercutting of hypertrophic inferior and superior articular processes without any major disruption of facet joints and overlying capsules is possible (Fig. 3). Mobilizing the ligamentum flavum from the inner surface of the cranial lamina and intermittent use of a laminar spreader provide a wide interlaminar surgical window in the prone position on elevated frame. Domed undercutting of the internal portion of the hypertrophied lamina, which compresses central canal or proximal exiting roots is possible using a table or microscope tilting in the coronal and axial plane (Fig. 4, 5). This internal laminoplasty technique can preserve the posterior arch of the lamina and spinous process overlying the spinal thecal sac during decompression of neural tissue, and may prevent epidural fibrosis and help physiologic healing in detached muscle and ligaments as seen in laminoplasty of the cervical spine. In addition, sharp dividing with blade and retraction of the supraspinous and interspinous ligaments with paraspinal muscle bulk could minimize damage to the muscles. Tight closing of the ligaments onto the spinous processes can restore the integrity of the ligaments and may provide additional stability. Using this technique, an excellent outcome showing improvement in back/buttock pain and leg pain (>75% of their initial VAS score) was observed in 75.0% and 76.2% of cases, respectively. These results are comparable to early surgical results showing an excellent outcome using other modified laminectomy technique (ranging from 61% to 79%)15,17).
This is the first study to explain CDL procedure and early surgical results. A long-term follow-up study is underway investigating surgical outcomes of LSS using this procedure. Future research is being planned to do a randomized controlled study comparing this procedure and spinal fusion for treatment of LSS.
CONCLUSION
This technique makes possible the inclined undercutting of hypertrophied lamina and superior articular processes in the lateral recess area without violating overlying inferior articular processes and joint capsules to maintain facet stability. This means that CDL provides an ideal technique to combine maximal central and lateral decompression with minimal resection of critical bony structures. The wide decompression of neural components while maintaining stability may guarantee good long-term results.