INTRODUCTION
The etiologies of intracranial artery dissection are various, the exogenous triggers like trauma, infection as well as inherited connective tissue disorders like moyamoya disease, fibromuscular dysplasia, and Marfan's syndrome. Alpha 1 antitrypsin deficiency and hyperhomocysteinemia are also distributing factors of carotid artery dissection19,25). The internal carotid artery dissection is responsible for less than 2% of all stroke and for 10-20% of stroke of young adults22). The dissection tends to occur in proximal internal carotid artery (ICA) and rare in distal ICA except when the cause is exogenous such as infection. Dissecting aneurysms of the intracranial posterior circulation are also rare that produce acute brain stem infarction or hemorrhage in young, healthy patients13,28,29). We report a case of multiple dissecting aneurysms of left superior cerebellar artery (SCA), left posterior inferior cerebellar artery (PICA) and right pericallosal artery in patient who presented with subarachnoid hemorrhage. We will also discuss of the relevance between dissecting aneurysm with the patient's medical history, thrombocythemia.
CASE REPORT
A 42-year-old man was admitted to emergency room with a history of decrease in the level of consciousness. The patient was in drowsy mentality, localizing to painful stimuli. His pupil reflexes were equal and symmetric. Yet, his motor response was reduced to grade three on the right. He had no previous event of motor weakness or dizziness before the onset of mental change. He had past medical history of hereditary spherocytosis and underwent splenectomy. During the follow up, his blood test showed thrombocytosis. His bone marrow biopsy reported megakaryocytic hyperplasia and he was diagnosed to essential thrombocythemia (ET). After a year, he was diagnosed to cerebral infarction and had been taking oral anti-platelet agent, since then. His chest X-ray, electrocardiogram, and echocardiogram showed normal findings. The routine laboratory tests were normal except the platelet count, 660 K/uL. Serum elastase was also within normal limit.
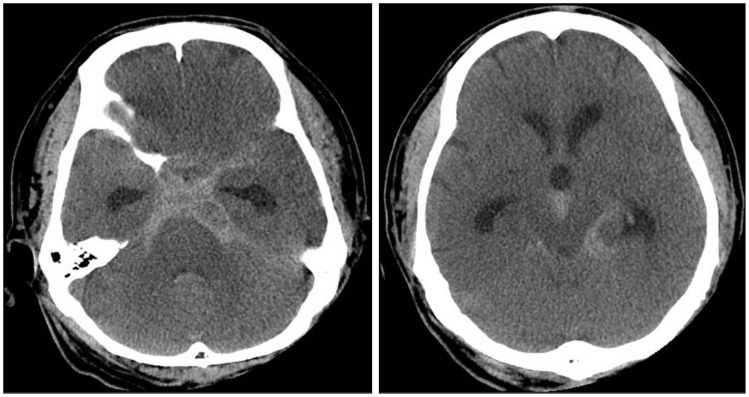
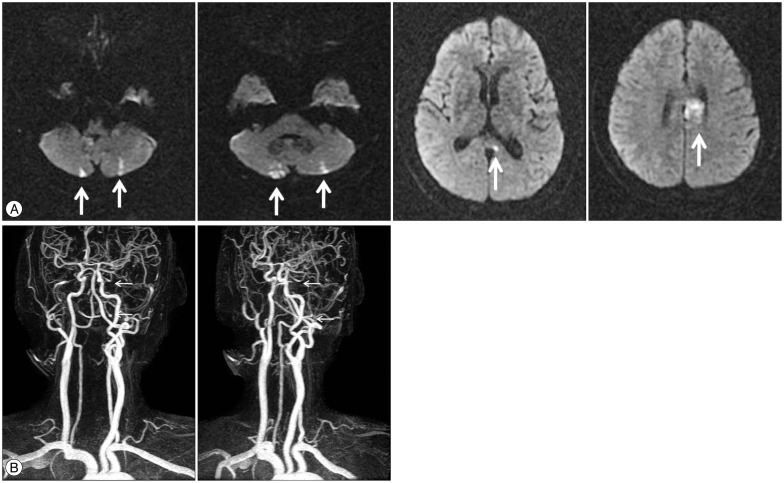
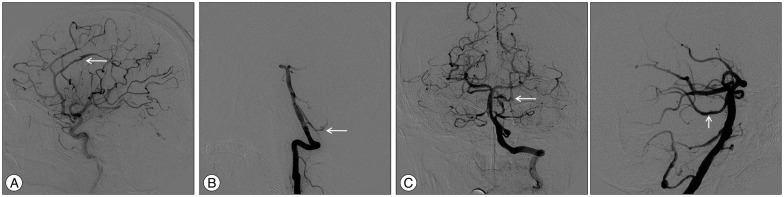
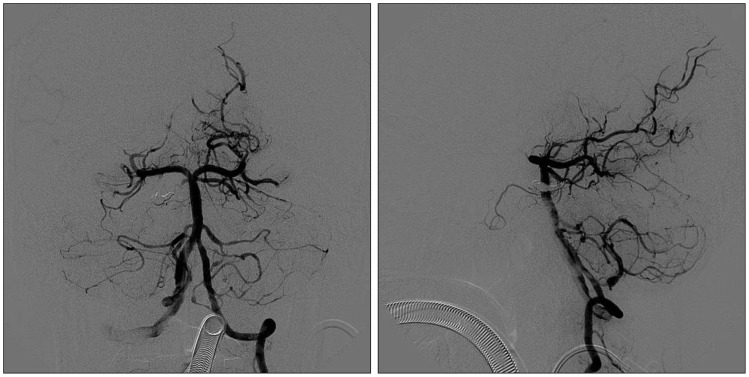
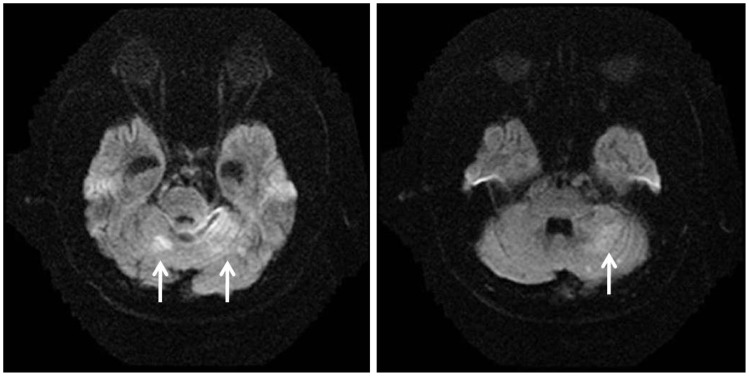
Emergent brain CT showed diffuse subarachnoid hemorrhage (SAH) in the basal cistern and acute hydrocephalus (Fig. 1). The hematoma was located in posterior fossa, especially in interpeduncular cistern and prepontine cistern. The diffusion MRI, which was done one year prior to the time of stroke, showed multiple cerebral infarctions on both cerebellum and body of corpus callosum (Fig. 2A). With MR angiography, we could identify the fusiform aneurysms on the left SCA and the left PICA. Each size was 3.2×3.7×7.0 mm and 3.9×4.0×7.2 mm (Fig. 2B). The conventional angiography revealed multiple dissecting aneurysms in left SCA, left PICA and right pericallosal artery (Fig. 3). There was no proximal carotid artery dissection. Considering hematoma distribution, we concluded that the SCA aneurysm was responsible for SAH. Since collateral circulation to midbrain, pons and cerebellum was abundant, we decided to occlude left SCA with coil embolization (Fig. 4). During the procedure, there was no event of vessel occlusion or thrombus formation. Postoperative diffusion MRI revealed cerebellar infarction; however, the patient showed no clinical symptom and was able to discharge with alert mentality, recovered from hemiparesis after rehabilitation (Fig. 5).
DISCUSSION
Intracranial dissection is rare event comparing to extracranial dissection, and is usually demonstrate ischemic event of young adults when it's symptomatic5,22). It usually relates to exogenous triggers like trauma, infection as well as inherited connective tissue disorders. Our case was very rare one because it was a case of multiple intracranial dissecting aneurysms that resulted in SAH as well as acute cerebral infarction which was related to no other risk factors except ET.
Essential thrombocythemia is characterized by a high platelet count, originating from a pluripotent stem cell and usually affects middle aged to elderly. Nearly half of the patients are asymptomatic while the other half has vascular occlusive or hemorrhagic event14). It is known to cause a prothrombic state10,17), and there are reports that describe the relationship between ET with cerebral ischemic event. Arboix et al.3) has reported several cases of large-vessel occlusion which resulted in ischemic stroke due to ET. Bogousslavsky et al.6) has reported that the ischemic stroke attributed to ET was found in 0.4% of cases in the Lausanne Stroke registry. There have been reports of intrapetrous ICA dissection of the patient with ET9,12), yet multiple intracrnial dissecting aneurysms of the patient with ET has been rarely reported. Piepgras et al.20) has reported the case of distal middle cerebral artery dissecting aneurysm secondary to proximal artery dissection, however, in our case, we could not find any dissection or occlusion in proximal arteries.
There are explanations that ET increases the incidence of intracranial dissection. ET, by changing prothrombotic state, causes a disturbance of microcirculation of vasa vasorum and as a result, increases the vulnerability of the vessel walls10). However, this theory only explains the dissection of extracranial arteries that the vasa vasorum is usually distributed to and does not fit in our case7). ET can induce endothelial damage by activating leukocyte and releasing the elastase and alkaline phosphatase that play a role of the pathogenesis of the prothrombic state8).
There are anatomical differences between extracranial artery and intracranial artery. The most characteristic structure of intracranial artery is internal elastic lamina. Instead of lack of external elastic membrane, thinner adventitia, and fewer elastic fibers of media, internal elastic lamina is thicker than extracranial artery23). In addition, the media and internal layer of intracranial artery is lack of vasa vasorum7). These changes occurs at the level of skull base in the carotid artery and at the 1 cm proximal to the dural perforation in vertebral artery27).
With the anatomical differences, there are pathological differences between dissecting aneurysm of extracranial and intracranial arteries. In the extracranial artery, dissection usually occurs between the media and adventitia or outer layer of the media11,13,23,28). In extracranial artery dissection, for example, cystic medial necrosis and degeneration of elastic tissue in the media is observed4,18). In the intracranial artery, on the other hand, intramural hematoma is usually formed between internal elastic lamina and media1,15,16,28,29). Thus, the clinical manifestation of the intracranial dissection is usually an ischemic stroke. When the dissection involves the subadventitia and rupture into the subarachnoid space, SAH is presented2,21,24,26,29).