Kim, Lee, Bang, Kwon, Hwang, and Oh: Epidemiology of Moyamoya Disease in Korea: Based on National Health Insurance Service Data
Abstract
There have been a few studies reporting the epidemiology of moyamoya disease in Korea. Previous studies revealed relatively high prevalence and incidence of moyamoya disease in Korea and Japan. This study was designed to provide the latest epidemiologic information of moyamoya disease in Korea. We analyzed a database comprising of 50 million people covered in Korea by the National Health Insurance Service to calculate the prevalence. The incidence was estimated by eliminating the duplicated records of previous 3 years. We summarized the prevalence and incidence according to age, sex, and local distribution. In addition, the chronological changes were demonstrated with direct standardization using the 2010 population structure information. The standardized prevalence was 6.5 per 100000 persons in 2005, which was increased to 18.1 in 2013. In the same period, standardized incidence was increased from 2.7 to 4.3 per 100000 persons. The prevalence for men was 4.9 and 8.3 for women in 2005. In 2013, the prevalence had increased for men and women to 13.8 and 25.3, respectively. The incidence for men and women was 2.2 and 3.2, respectively, in 2005. It had increased to 3.5 and 5.7, respectively. The mean age of patients was 33.5 in 2005 and increased to 42.5 in 2013. The peak prevalent age group had shifted slightly to the older age groups, with chronologically consistent female predominance. The prevalence was highest in Jeollabuk province and lowest in Ulsan city.
Key Words: Epidemiology · Korea · Moyamoya disease.
INTRODUCTION
Moyamoya disease (MMD) is a rare disease characterized by spontaneous stenosis or occlusion of the distal internal carotid artery 18). Abnormal development of the arterial collateral network is also accompanied with progressive stenosis 16). Moyamoya, meaning "puff of smoke" in Japanese, was coined by Suzuki and depended on the shape of collaterals 19). Several reports have revealed epidemiologic characteristic of MMD. First of all, the most prominent finding was the international difference in incidence and prevalence 8,10). High incidence and prevalence were shown in Asian countries, especially Korea, Japan, Taiwan, and China 1,39,13). The bimodal age distribution and gender difference were consistently reported by several previous studies 3,79,21). On the other hand, there have been a few studies concerning the epidemiology of MMD in Korea 1,46,7). Among them, two studies used institutional data that may not be considered as nationwide statistics. Other two studies utilized data from the National Health Insurance Service (NHIS), which has been run by the Korean government and covers almost the entire Korean population 1,7). To provide up-to-date epidemiologic information of MMD in Korea, we reviewed NHIS data between 2005 and 2013.
MATERIALS AND METHODS
Data source
NHIS data used in this study included approximately 50 million people covered in Korea. These data were based on claims that were sent from healthcare institutions. All patients' data were given unique identification codes that masked their resident registration number. The claims database contained information about the utilization of healthcare system, including the total number of patients, expenditures, and date of visit, admission and discharge. These data could be divided by age, sex, and administrative district. And information regarding medical resources were obtained from the annual report by NHIS, which included the number of health care institutes and human resources.
Patient selection
Using the International Classification of Diseases, 10th Revision (ICD-10) diagnostic code, we collected data from patients with MMD visiting healthcare institutions between 2005 and 2013. This diagnostic code was used in both the main diagnosis and sub-diagnosis for querying. It may be important to identify MMD patients with maximal estimation because the database from NHIS did not contain detailed information regarding symptoms and diagnostic methods.
Data analysis
Prevalent cases were defined as any patients that visited a healthcare institution with MMD, regardless of their symptoms and treatment history. Incident cases were extracted from prevalent cases by subtracting the patients who had any claim record in the previous 3-years. The population size of each group was obtained from the annual reports by Statistics Korea ( www.kostat.go.kr), which could be searched in Korean Open Data Portal ( www.data.go.kr). Prevalence and incidence were calculated as below.
The annual prevalence and incidence were standardized using the population structure data in 2010, which was produced by a population census. The proportions of each age groups and sex were calculated in accordance to the result of census. The standardized prevalence and incidence were calculated by a weighted summation of crude prevalence and incidence for each group using the aforementioned proportional indices.
RESULTS
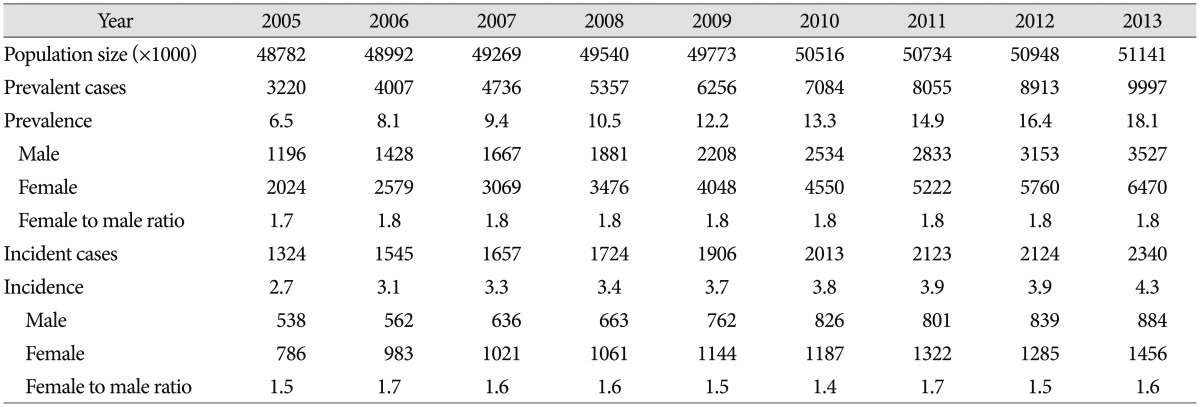
Prevalence and incidence
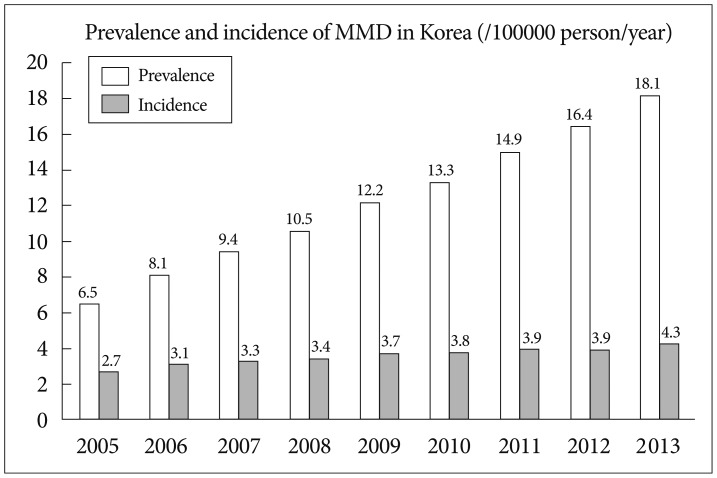
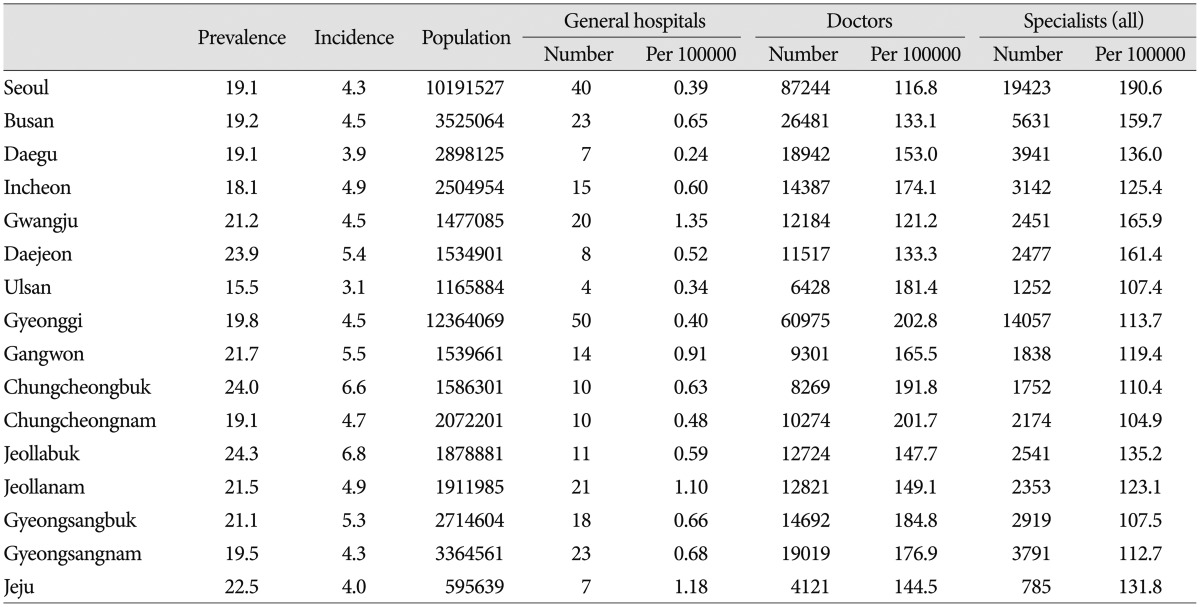
From 2005 to 2013, the number of MMD patients using healthcare services increased by <about> threefold from 3220 to 9997. The crude prevalence was 6.6 in 2005 and gradually increased to 19.5 in 2013. After standardization of sex and age, the prevalence was adjusted to 6.5 and 18.1 in 2005 and 2013, respectively ( Table 1). An average annual increase of standardized prevalence was 22.3% ( Fig. 1). In the same period, an average annual increase of the general population in Korea was estimated to be 0.6%. There had been a total of 1324 incidences in 2005. Because the population size had been about 49 million, crude incidence had been 2.7 per 100000 person/year, which was same after standardization. In accordance to the increases of patients, crude incidence of MMD in Korea was calculated as 4.6 in 2013. The standardized incidence in 2013 was 4.3 ( Table 1). The average annual increase of standardized incidence was 7.4% ( Fig. 1).
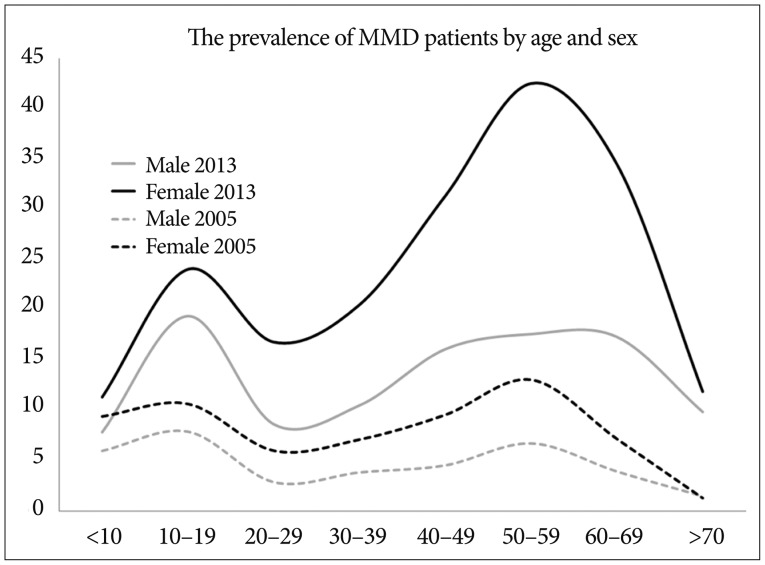
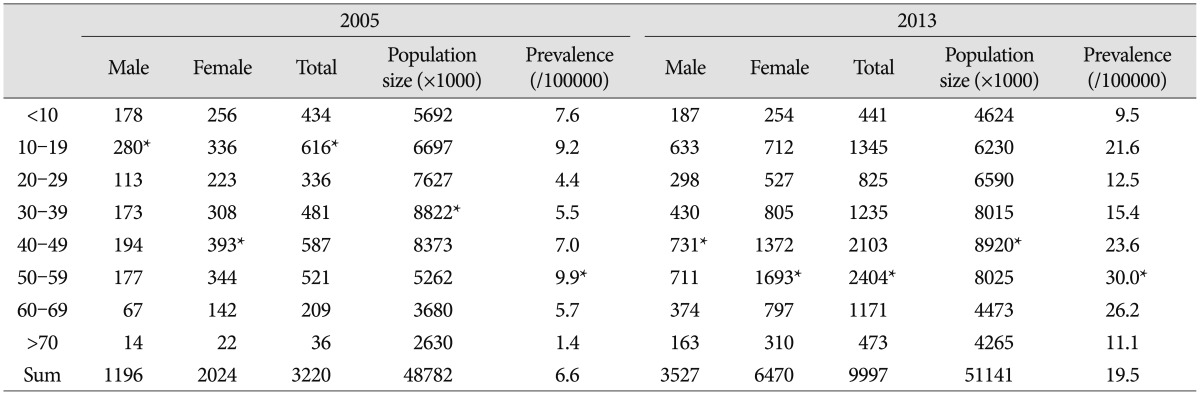
Gender and age
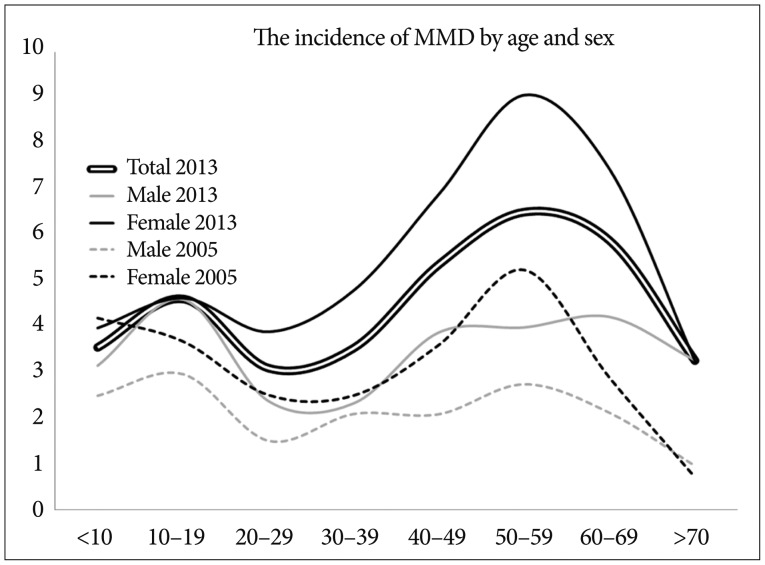
The prevalence for men was 4.9 and 8.3 for women in 2005. In 2013, the prevalence had increased for men and women to 13.8 and 25.3, respectively. The female to male ratio of 1.8 was maintained relatively constant. The age distribution showed a bimodal pattern. Most patients belonged to the age group of 10-19, followed by 40-49 in 2005. In the aspect of prevalence, highest group was age 50-59 and 10-19. However in 2013, the peak prevalent group was more prominent in age group of 50-59 (30.0 per 100000) ( Table 2). As a result, the mean age of patients was 33.5 in 2005 and increased to 42.5 in 2013. In a data comparison between 2005 and 2013, the prevalence of middle-aged patients had increased more than the pediatric group in female ( Fig. 2). The incidence for men and women was 2.2 and 3.2, respectively, in 2005. From 2005 to 2013, male incidence of MMD had increased by 59.1%, from 2.2 to 3.5. On the other hand, female incidence had increased from 3.2 to 5.7 (76.3%) in the same period. The female to male ratio of incidence was observed variously in the range from 1.4 to 1.7 over 9 years. Bimodal age distribution of incidence was confirmed, and it was more prominent in women than in men ( Fig. 3).
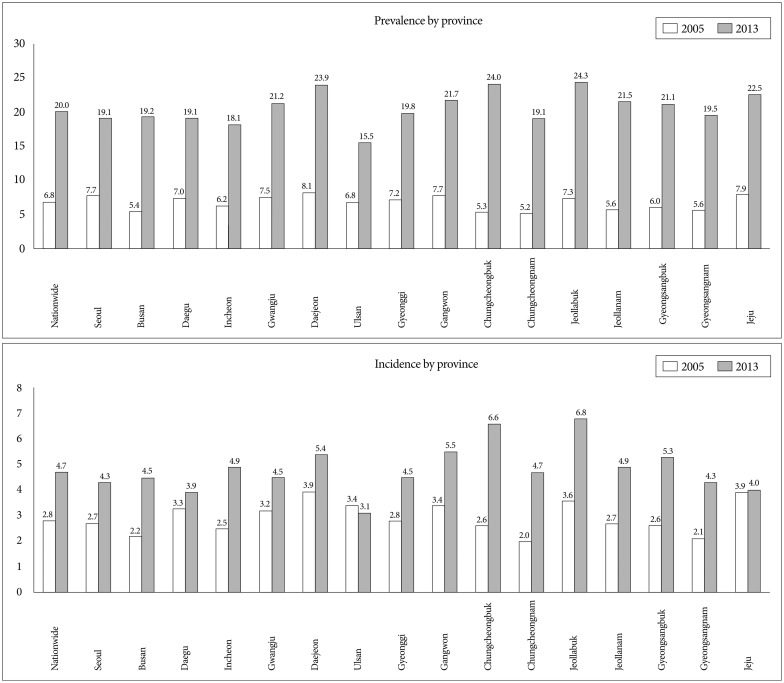
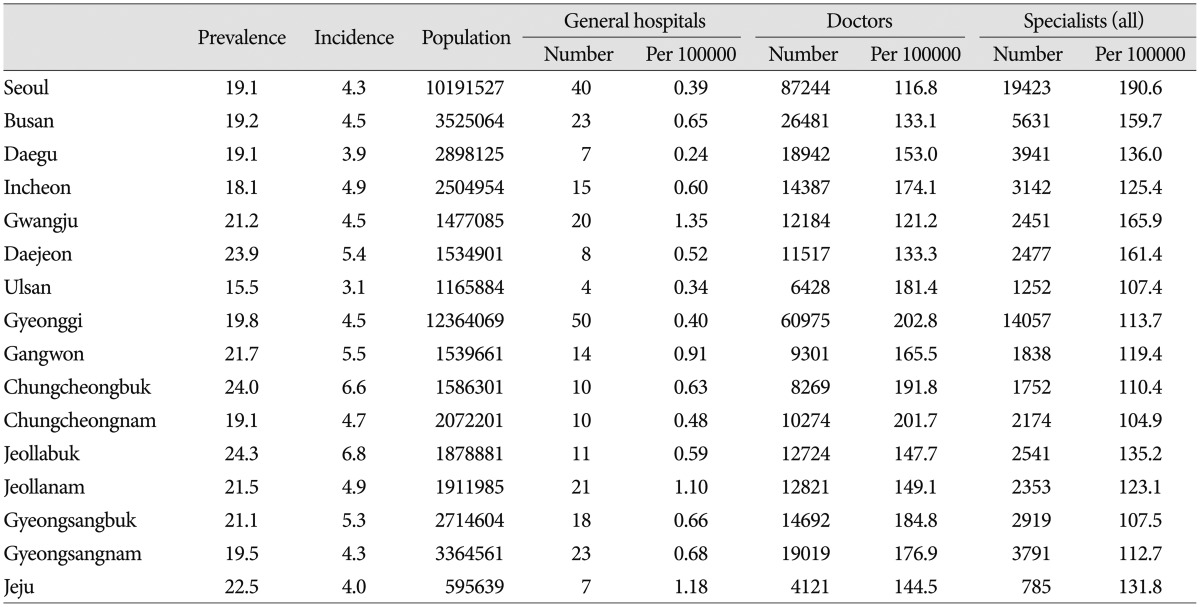
Regional distributions
With respect to local distribution of MMD in Korea, the crude prevalence had been highest in Jeollabuk province and lowest in Ulsan city as of 2013 ( Table 3). The prevalence of MMD in Jeollabuk province was about 50% higher than in Ulsan city. From 2005 to 2013, all provinces experienced similar trends of increment in MMD prevalence. On the other hand, among the 16 provinces, 15 experienced an increase in incidence. The highest incidence was observed in Jeollabuk province ( Fig. 4). The regional distribution of medical resources was inspected and analyzed. In provinces with lesser general hospital per 100000 population (<0.5), both the crude prevalence (18.5±1.7 vs. 21.5±2.0, p=0.013) and crude incidence (4.1±0.6 vs. 5.2±0.9, p=0.027) were lower. However human resources, including the number of general practitioners and board certificated doctors (specialists), were not correlated.
DISCUSSION
In this study, we calculated the prevalence and incidence of MMD using a nationwide database. In 2013, the standardized prevalence and incidence of MMD was 18.1 and 4.3 per 100000, respectively. In Japan, the nationwide incidence of MMD was estimated to be 0.54 in 2003 9). However, they used questionnaires, and the response rate was only 57%. Baba et al. 2) reported the incidence of MMD as 0.94 in the Hokkaido province of Japan. Although it was not a nationwide study, the investigators performed an all-inclusive survey. Recently, Chen et al. 3) reported a nationwide epidemiology of Taiwan. They used the national database covering most of the population in Taiwan. The prevalence and incidence of MMD was 1.61 and 0.20, respectively, in 2011. Although these results were relatively low compared to ours, they revealed that the incidence had increased since 2000 in Taiwan. Moreover, the increment of incidence was largely due to an increase in the number of adult patients. Such phenomenon resembles our results. Recently, RNF213 was found to be a susceptible gene with MMD 12). Liu et at. 11) presented a difference of genetic background between China and Korea/Japan. They found that p.R4810K was detected 0.43% in China, whereas 1.36% in Korea/Japan. Although it has not been fully elucidated, the difference of genetic background may play an important role in these regional differences of MMD in East Asia. Female predominance has been a consistent trend reported by many articles 2,35,913,1520,2122,23). Among these, relatively weak female predominance (<1.5) was reported in China and Taiwan 3,513). Conversely, investigators from Korea and Japan, including this study, reported relatively strong female predominance (≥1.8) 2,79,21). As it had been well known, bimodal age distribution of MMD was confirmed in Korea. The important change from 2005 was that the prevalence and incidence of MMD has increased much more for middle-aged patients than pediatric populations. Furthermore, this increment was more pronounced in women ( Fig. 2, 3). This change should be interpreted carefully. Because patients who were diagnosed with MMD are entitled to economic benefit from NHIS in Korea, the diagnostic code for MMD could be over-issued for other atherosclerotic intracranial stenosis, which affect the older population. Nevertheless, similar trends of change were reported by foreign investigation, already. Baba et al. 2) reported that the highest peak of incidence shifted from children to adults, especially in women. Chen et al. 3) announced similar results, and they explained that increased prevalence of comorbid ischemic stroke was associated with this trend. Although there had been a few reports regarding the epidemiology of MMD in Korea using national database, the knowledge of regional distribution had been minimal 1,7). In this study, the prevalence and incidence of MMD were measured variously by region. And they were associated with the supply rate of general hospitals. This relationship could not be investigated with an international comparison due to different genetic background 11). Further studies using data about distribution of diagnostic tools, including magnetic resonance image and digital subtraction angiography, would be helpful for understanding the relationship between the epidemiology of MMD and medical resources. Although this study confirmed high prevalence and incidence of MMD in Korea based on a nationwide database, there were some limitations. First limitation of this study was its diagnostic accuracy. The database we used was comprised solely on the claims of healthcare institutes. Therefore, a validation of diagnostic criteria was impossible. Moreover, the data from NHIS were subject to change according to the diagnostic tool and pattern of patient follow-up. Because there was no clinical guideline for the follow-up of MMD patients, some doctors recommended frequent visits, while others did not. Secondly, because we applied the diagnostic code to both the main diagnosis and sub-diagnosis, the calculated prevalence and incidence of MMD seemed to be the maximal estimation. The proportion of MMD as sub-diagnosis had been about 7% thoroughout the investigation period. The prevalence and incidence of MMD were reported in two previous studies using national database 1,7). According to Ahn et al. 1), estimated prevalence and incidence were 10.0 and 1.9, respectively in 2008; Im et al. 7) reported that they were 9.1 and 1.0, respectively. The prevalence of previous studies was similar with our result, which was 10.5 in 2008. However, the incidence of MMD was relatively higher in this study (3.4 in 2008). Because Ahn et al. 1) used rare intractable disease (RID) registry, which was considered to have more tight inclusion criteria for identifying incident case, the estimated incidence could be lower. Also, we could not distinguish between MMD presented with hemorrhage and MMD presented with ischemia. These two types of presentation were well-known as they differ in age distribution and prognosis 10,1417). Furthermore, it was difficult to differentiate symptomatic from asymptomatic or stable from progressive states of the disease in this study. For improving the accuracy of estimation, a comparative and analytic study with a database of RID from the national registration system for intractable diseases, including MMD, could provide more delicate epidemiologic information.
CONCLUSION
The prevalence and incidence of MMD in Korea had gradually increased, and they were 18.1 and 4.3 per 100000 annually with age and sex standardization, respectively, in 2013. The peak prevalent age group had slightly shifted to the older age groups, with higher female predominance. The local difference of prevalence and incidence was also found.
Acknowledgements
This study was supported by a grant of the Korea Healthcare Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (HI10C2020).
References
1. Ahn IM, Park DH, Hann HJ, Kim KH, Kim HJ, Ahn HS : Incidence, prevalence, and survival of moyamoya disease in Korea : a nationwide, population-based study. Stroke 2014, 45 : 1090-1095,   2. Baba T, Houkin K, Kuroda S : Novel epidemiological features of moyamoya disease. J Neurol Neurosurg Psychiatry 2008, 79 : 900-904,   3. Chen PC, Yang SH, Chien KL, Tsai IJ, Kuo MF : Epidemiology of moyamoya disease in Taiwan : a nationwide population-based study. Stroke 2014, 45 : 1258-1263,   4. Choi KS : Moyamoya disease in Korea. Edited by Suzuki J : In: Advances in Surgery for Cerebral Stroke. Tokyo : Springer-Verlag, 1988, pp107-109
5. Hung CC, Tu YK, Su CF, Lin LS, Shih CJ : Epidemiological study of moyamoya disease in Taiwan. Clin Neurol Neurosurg 1997, 99( Suppl 2):S23-S25,   6. Ikezaki K, Han DH, Kawano T, Inamura T, Fukui M : Epidemiological survey of moyamoya disease in Korea. Clin Neurol Neurosurg 1997, 99( Suppl 2):S6-S10,   7. Im SH, Cho CB, Joo WI, Chough CK, Park HK, Lee KJ, et al : Prevalence and epidemiological features of moyamoya disease in Korea. J Cerebrovasc Endovasc Neurosurg 2012, 14 : 75-78,    8. Kleinloog R, Regli L, Rinkel GJ, Klijn CJ : Regional differences in incidence and patient characteristics of moyamoya disease : a systematic review. J Neurol Neurosurg Psychiatry 2012, 83 : 531-536,   9. Kuriyama S, Kusaka Y, Fujimura M, Wakai K, Tamakoshi A, Hashimoto S, et al : Prevalence and clinicoepidemiological features of moyamoya disease in Japan : findings from a nationwide epidemiological survey. Stroke 2008, 39 : 42-47,   10. Kuroda S, Houkin K : Moyamoya disease : current concepts and future perspectives. Lancet Neurol 2008, 7 : 1056-1066,   11. Liu W, Hitomi T, Kobayashi H, Harada KH, Koizumi A : Distribution of moyamoya disease susceptibility polymorphism p.R4810K in RNF213 in East and Southeast Asian populations. Neurol Med Chir (Tokyo) 2012, 52 : 299-303,   12. Liu W, Morito D, Takashima S, Mineharu Y, Kobayashi H, Hitomi T, et al : Identification of RNF213 as a susceptibility gene for moyamoya disease and its possible role in vascular development. PLoS One 2011, 6 : e22542,    13. Miao W, Zhao PL, Zhang YS, Liu HY, Chang Y, Ma J, et al : Epidemiological and clinical features of Moyamoya disease in Nanjing, China. Clin Neurol Neurosurg 2010, 112 : 199-203,   14. Miyamoto S, Yoshimoto T, Hashimoto N, Okada Y, Tsuji I, Tominaga T, et al : Effects of extracranial-intracranial bypass for patients with hemorrhagic moyamoya disease : results of the Japan Adult Moyamoya Trial. Stroke 2014, 45 : 1415-1421,   15. Nam DH, Oh CW, Wang KC, Paek SH, Hwang YS, Kim IO, et al : Moyamoya disease : the differences between age groups in clinical presentation and hemodynamic characteristics. J Korean Neurosurg Soc 1997, 26 : 1357-1362,
16. Natori Y, Ikezaki K, Matsushima T, Fukui M : 'Angiographic moyamoya' its definition, classification, and therapy. Clin Neurol Neurosurg 1997, 99( Suppl 2):S168-S172,   17. Saeki N, Nakazaki S, Kubota M, Yamaura A, Hoshi S, Sunada S, et al : Hemorrhagic type moyamoya disease. Clin Neurol Neurosurg 1997, 99( Suppl 2):S196-S201,   18. Suzuki J, Kodama N : Moyamoya disease--a review. Stroke 1983, 14 : 104-109,   19. Suzuki J, Takaku A : Cerebrovascular "moyamoya" disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol 1969, 20 : 288-299,   20. Uchino K, Johnston SC, Becker KJ, Tirschwell DL : Moyamoya disease in Washington State and California. Neurology 2005, 65 : 956-958,   21. Wakai K, Tamakoshi A, Ikezaki K, Fukui M, Kawamura T, Aoki R, et al : Epidemiological features of moyamoya disease in Japan : findings from a nationwide survey. Clin Neurol Neurosurg 1997, 99( Suppl 2):S1-S5,  22. Wetjen NM, Garell PC, Stence NV, Loftus CM : Moyamoya disease in the midwestern United States. Neurosurg Focus 1998, 5 : e1,  23. Yonekawa Y, Ogata N, Kaku Y, Taub E, Imhof HG : Moyamoya disease in Europe, past and present status. Clin Neurol Neurosurg 1997, 99( Suppl 2):S58-S60,  
Fig. 1
The prevalence and incidence of moyamoya disease in Korea from 2005 to 2013.
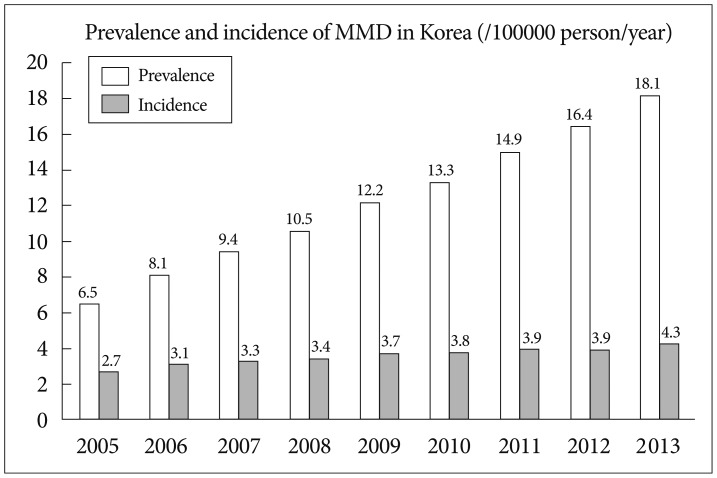
Fig. 2
The prevalence of moyamoya disease by age and sex in 2005 and 2013. The prevalence of moyamoya disease increased during this period. The largest increment of patients was seen in middle aged women.
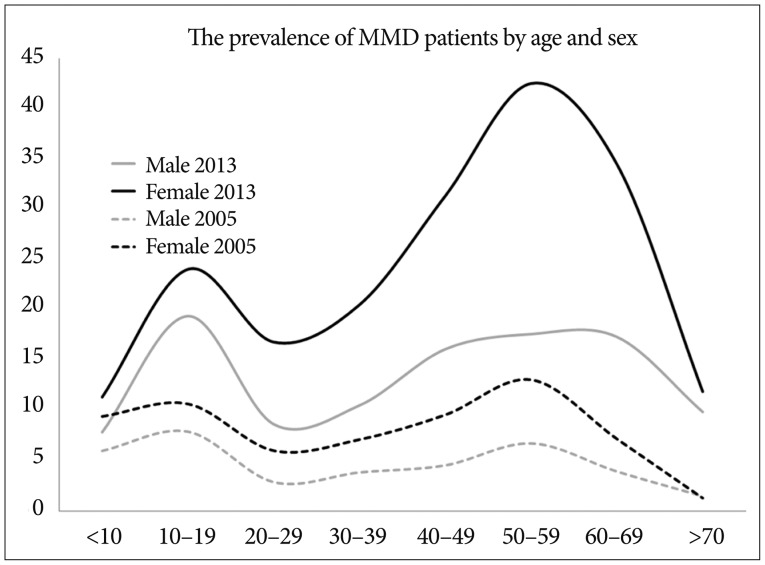
Fig. 3
The incidence of moyamoya disease by age and sex. In populations over 40 years old, the incidence change was prominent in women than in men. In 2013, the peak incidence was shown in ages 10-19 and 50-59.
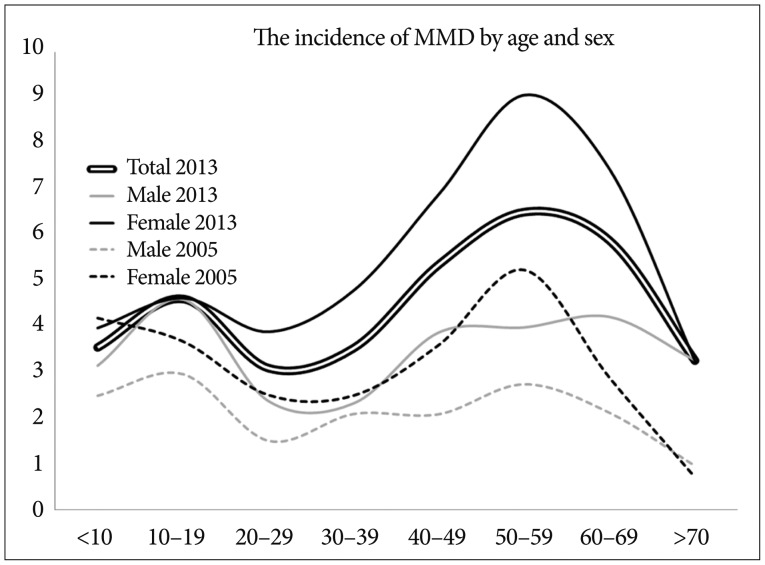
Fig. 4
The local distribution of prevalence and incidence of moyamoya disease. Jeollabuk was the province with highest prevalence and incidence in 2013.
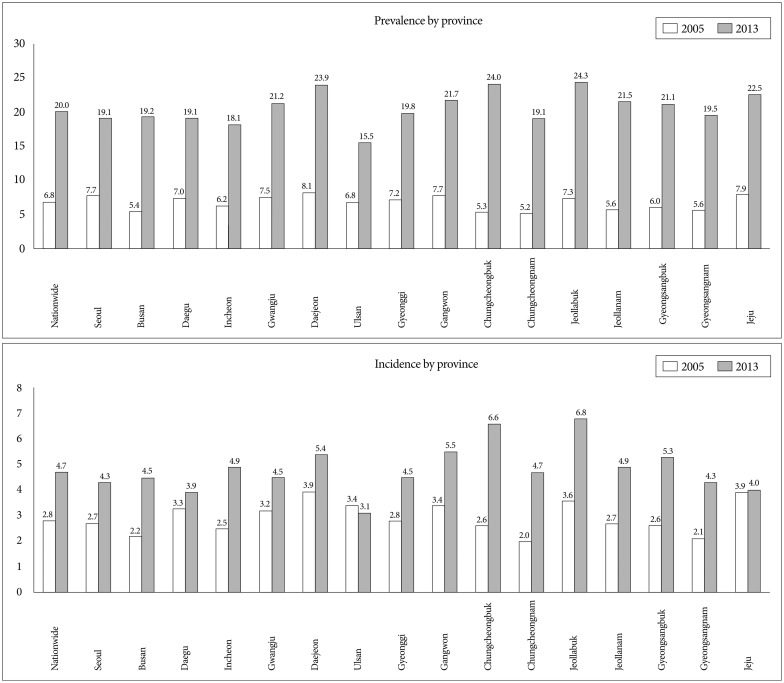
Table 1
Prevalence and incidence of moyamoya disease in Korea from 2005 to 2013
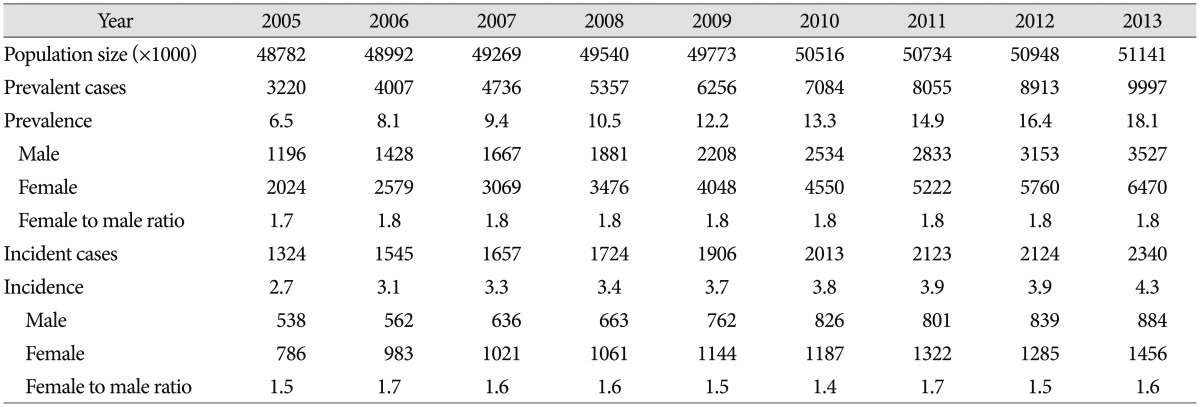
Table 2
Age distribution of moyamoya disease in 2005 and 2013
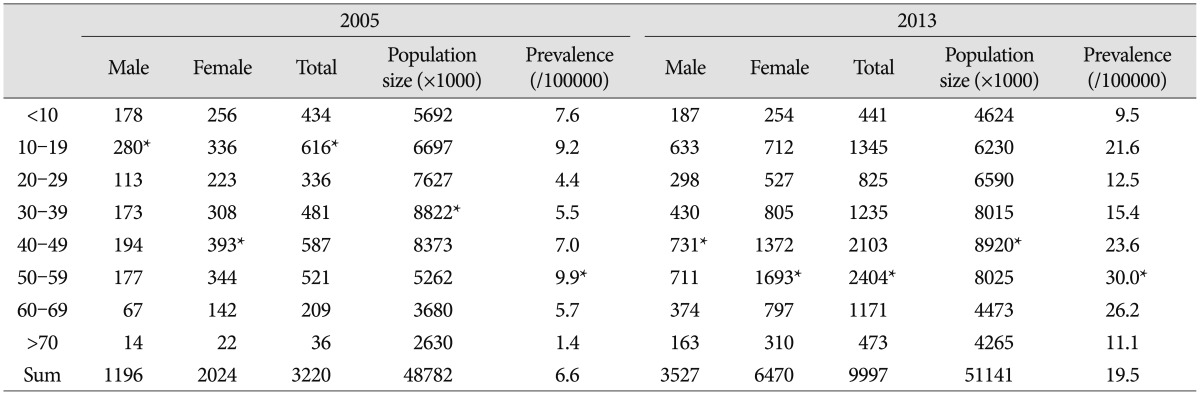
Table 3
Regional distribution of moyamoya disease and medical resources in 2013
|
|