INTRODUCTION
Among the osteoporotic skeletal fractures, osteoporotic vertebral fracture (OVF) is the common type of osteoporotic fractures in older adults2). The musculoskeletal disorders including osteoporosis and bone fragility fractures rank as the second common cause of disability estimated by the years lost due to disability worldwide16). Therefore, preventive strategy for osteoporotic fracture may be important to reduce the burden of OVF in population. Bone mineral density (BMD) has been widely used as a predictor of the osteoporotic fractures13). Although measurement of BMD by dual-energy X-ray absorptiometry (DXA) is routinely performed to predict the risk of osteoporotic fracture, most fractures occur in the patient population with a BMD T-score above the WHO recommended threshold for osteoporosis3). The absolute risk of osteoporotic fracture increases with age at any given BMD5,18). Therefore, discrepancy between BMD and the risk of osteoporotic fracture may exist because of paradoxical error that improves BMD such as osteoarthritis9). Recently, the incorporation of clinical risk factors including age, sex and body mass index, use of glucocorticoids, secondary osteoporosis, rheumatoid arthritis and parental history of hip fracture, current smoking, and alcohol intake, the incorporating clinical risk factors with BMD has been shown to enhance fracture risk prediction4). Therefore, the World Health Organization (WHO) Collaborating Centre for Metabolic Bone Diseases developed the Fracture Risk Assessment (FRAX¬ģ), a computerbased algorithm (http://www.shef.ac.uk/FRAX) that provides a tool of assessing 10-year probability of osteoporotic hip fracture and major fractures including vertebral fracture by calculating the probability from clinical risk factors including BMD11). The major osteoporotic fracture includes other skeleton as distal forearm, proximal humerus and spine12). The FRAX is available in 50 models for 45 countries and the website has been translated into diffent19 languages (FRAX version 3.6)15). The current National Osteoporosis Foundation (NOF) Guide recommends treating patients with 3% and over FRAX 10-year risk scores for hip fracture or 20% and over for major osteoporotic fracture17). However, the WHO selected not the lumbar spine T-score but the femoral neck T-score as the reference site for BMD in the FRAX tool. Therefore, there is controversy over the feasibility of FRAX for the risk prediction of OVF using femur neck BMD and not lumbar spine BMD19). The aim of this study was to investigate the usefulness of femur neck bone mineral density (BMD) and lumbar BMD by comparing with prediction of osteoporotic vertebral fracture (OVF) using Fracture risk assessment (FRAX) tool. We investigated the significance of difference of other factors as activities of osteoblast and osteoclast between OVF and non-OVF groups.
MATERIALS AND METHODS
Study population
This was a cross-sectional study conducted from 2013 to 2014 on all patients 60 years old and over who were admitted to our hospital for treatment of degenerative spine disease or osteoporotic vertebral fracture. We enrolled patients with degenerative spine disease or osteoporotic spine fracture. Exclusion criteria were infectious spondylodiscitis, primary or metastatic spine tumor or spinal cord injury, previous history of non-osteoporotic vertebral fracture, and spine operation. Therefore, 110 consecutive patients were enrolled in the present study. The institutional database of the 110 patients was reviewed according to the sex, age, past and current medical history and cause of current admission, in order to calculate the fracture risk within 10 years using FRAX tool. The BMD, blood level of osteocalcin and C-terminal telopeptide (CTX) as markers of activities of osteoblast and osteoclast, respectively were analyzed using the institutional database. The retrospective study was approved by our Institutional Review Board.
The BMD of the lumbar spine and the femur neck was available in all patients of our study at the time of admission. BMD was measured by anteroposterior projection at L1-4 for the lumbar spine and at the femoral neck, trochanter, or the total hip for the femurs. The World Health Organization (WHO) classification system was applied to define osteoporosis as T-score ‚ȧ-2.5 and osteopenia as -2.5<T-score<-1. The blood levels of osteocalcin and CTX were available in 79 of 110 patients at the time of admission. We compared the blood levels of osteocalcin and CTX between non-OVF and OVF groups to identify significance in OVF using statistical difference. The value was compared between the non-OVF and OVF groups.
Osteoporotic fracture risk
The 10-year risk of hip and major osteoporotic fracture was calculated by FRAX algorithm of Korean model, which is available free of charge at www.shef.ac.uk/FRAX based on the patients' clinical characteristics including BMD. BMD of the femur neck and lumbar spine was used to calculate the risk of osteoporotic fracture by FRAX10,11).
Statistical analysis
The results were presented as mean¬Īstandard deviation. OVF and non-OVF groups comparison using FRAX with lumbar BMD and femur neck BMD was assessed by Student t-test and chi-square analysis. In subgroup analysis, vertebral fracture risk was compared using one-way analysis of variance. We assessed the overall discriminative value of the different risk scores by calculating the areas under the receiver operator characteristic (ROC) curve (AUC). Higher AUC values represent better prediction with the models. SPSS 22.0 was used for statistical analysis and the level of significance was set as p‚ȧ0.05.
RESULTS
Patient demographics
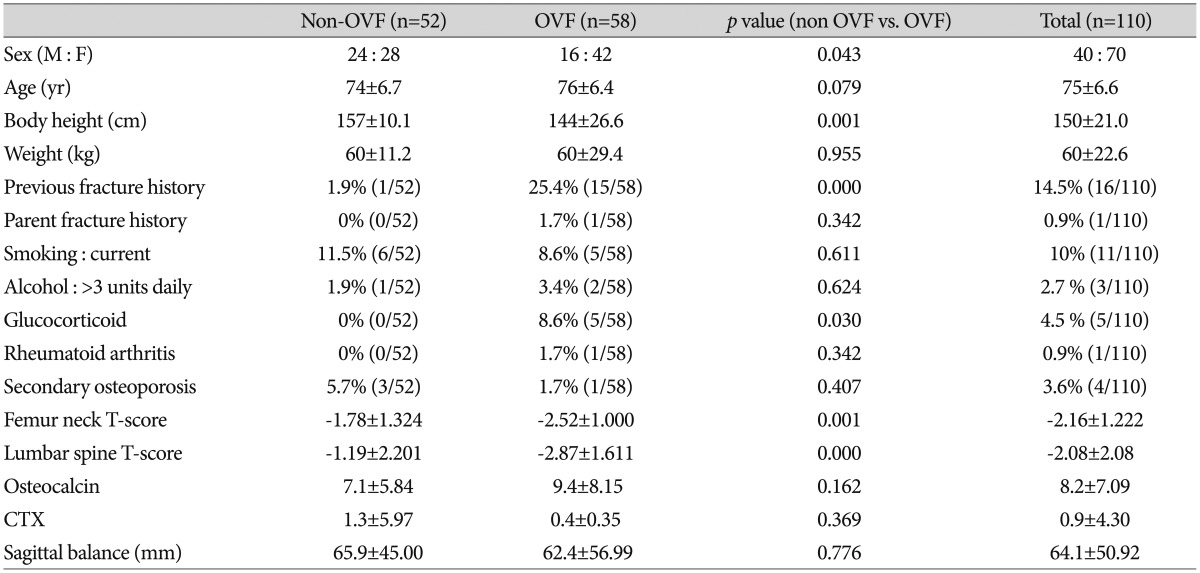
Of the 110 patients, 70 patients were women and 40 patients were men. Mean age of the patients was 75.6¬Ī6.65 years (range, 49 to 89 years). The number of patients with non-OVF and OVF were 52 and 58, respectively. The ratio of female in OVF group was superior to that in non-OVF (p=0.043). The body height in OVF group was significantly less than that in non-OVF group (p=0.001). In OVF group, the ratio of patients with previous fracture history or use of glucocorticoid was higher than those in non-OVF group (p=0.000 and 0.030, respectively). The levels of T-score of femur neck and lumbar spine in OVF group were significantly lower than those in non-OVF group (p=0.001 and 0.000, respectively). Demographics of the patients were listed in Table 1.
Risk of OVF using femur neck and lumbar spine BMD
The major fracture risk in FRAX using femur BMD in non-OVF and OVF groups was 6.7¬Ī6.13 and 11.4¬Ī10.06, respectively (p=0.007). The risk using lumbar BMD in the 2 groups was 6.9¬Ī8.91 and 15.1¬Ī15.08, respectively (p=0.002). In the comparison between non-OVF and recurrent OVF (n=13) groups, the risk using femur neck BMD was 6.7¬Ī6.13 and 16.4¬Ī20.87, respectively (p=0.122). Furthermore, the risk using lumbar BMD was 6.9¬Ī8.91 and 22.9¬Ī22.5, respectively (p=0.027).
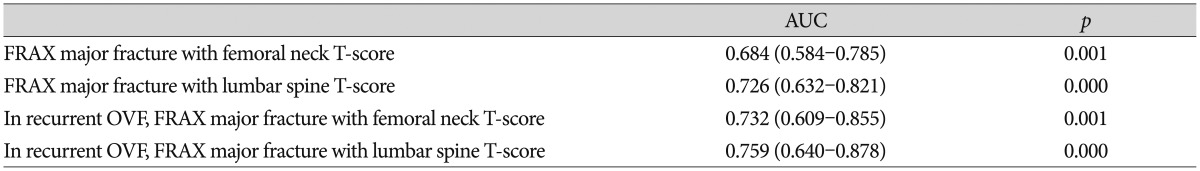
A model with no utility in predicting fracture would have an AUC of 0.50 (i.e., no better than flipping a coin or chance alone). The AUCs in the FRAX risk with lumbar and femur neck BMD were 0.726 and 0.684, respectively. In the recurrent OVF, the AUCs in the FRAX with lumbar and femur neck BMD were 0.759 and 0.732, respectively (Table 2). The AUC in FRAX using lumbar BMD was higher than the AUC with femur neck BMD (Fig. 1).
DISCUSSION
In the present study, we evaluated the 10-year probability of OVF using FRAX model with femur neck and lumbar spine BMD. Among the risk factors in FRAX model, sex, body height, previous fracture history, femur neck T-score and lumbar spine T-score were different factors between non-OVF and OVF groups. In addition, the AUC in the FRAX model with lumbar spine BMD was higher than the AUC with femur neck BMD.
Osteoporosis is a worldwide socioeconomic problem with an increasing severity and frequency, due to the progressive aging of the world's population1,2). The lifetime risk at 50 years of age for any osteoporotic fracture ranges between 40-50% in women and 13-22% in men, which is considered very high8). The prediction of patients with osteoporotic skeletal fracture and medical intervention are important to decrease the incidence of new onset osteoporotic skeletal fracture and the socioeconomic burden. Therefore, many countries have used the FRAX model following the guidelines of NOF for osteoporosis medication. The NOF guidelines recommended that anti-osteoporotic therapy should be considered in postmenopausal women and men aged 50 years and above, who met any of the following criteria: 1) a femoral neck or spine BMD T-score ‚ȧ -2.5; 2) a femoral neck T-score between -1 and -2.5 SD, with a 10-year hip fracture probability ‚Č•3% or major fracture (humerus, forearm, hip or vertebral fracture) probability ‚Č•20%14). The NOF guidelines are based on cost-effectiveness that estimate 35% prevention rate for 5 years to morbidity and mortality in the USA18). In the present study, the major fracture risk in FRAX in OVF group using femur neck BMD and lumbar BMD was 11.4¬Ī10.06 and 16.4¬Ī20.87, respectively; and the 2 values were below 20%. These results indicated that the recommended criteria for treatment osteoporosis using FRAX might be decreased. Also, in the oriental population, the femur neck size may be smaller than that of western people. Therefore, the reproducibility of measurements at the femur neck BMD could be poorer than that at lumbar spine. These concerns have caused controversy over the use of femur neck BMD or lumbar spine BMD in FRAX tool7). Several studies showed that the ability of risk prediction for the spinal fractures was similar between femoral neck BMD and lumbar spine BMD6,7). However, another study showed that lumbar spine BMD was more suitable for prediction of OVF using FRAX than that of femur neck BMD20). In these studies, morphological spinal fracture with or without back pain were enrolled. There was no study on symptomatic patients with OVF. In the present study, authors enrolled the symptomatic patients with OVF. The ability to predict the risk of symptomatic OVF was superior to that of femur neck BMD. In risk factors used in FRAX tool, sex, body height, previous fracture history and the use of glucocorticoid were more significant factors, as compared with patients without OVF.
There were several limitations in the present study. First, the data was obtained retrospectively from a small patient population who were admitted to our neurosurgical department for treatment of OVF or degenerative disease. Analysis of the small sized and unmatched patients groups can provide the bias and decrease the confidence of the results. Well-designed prospective study is needed in the future. Second, because asymptomatic patients were not enrolled in the present study, the result in the present study will be adjusted in the symptomatic patients with OVF. In addition, the contributing factors such as diabetes mellitus, kidney disease and thyroid disease were not considered. These factors could cause bias in the analysis of result. Future study should consider the large number of patients with or without OVF, other diseases related with bone quality and the differentiated study design to provide strong insistence of the importance of lumbar BMD in FRAX.