Han, Zhang, Han, and Jin: Intradural Transpetrosectomy for Petrous Apex Meningiomas
Abstract
Objective
This study aimed to assess the surgical results of the intradural transpetrosectomy for petrous apex meningiomas (PAMs). In addition, we describe the methods and techniques used to expose and manage superior petrous vein and greater superficial petrosal nerve.
Methods
The authors conducted a retrospective study of 16 patients with PAMs operated by the senior author via the intradural transpetrosectomy between February 2012 to May 2017. We reviewed patient data regarding the general characteristics, surgical technique and surgery-related outcomes and adopted a combined follow-up strategy of clinic and telephone contacts to evaluate postoperative complications.
Results
Simpson grade I and II resection was performed in 10 out of 16 cases (62.5%), and grade III resection were reported in the remaining six cases (37.5%) with no resultant mortality. The mean Karnofsky Performance Status score was 85.6 preoperatively and improved to 91.9 postoperatively, with a mean follow-up period of 34.4 months (range, 6-66 months). Tumor recurrence was found in two patients and they underwent the second surgical operation.
Conclusion
PAMs could be completely resected by the intradural transpetrosectomy with an improved survival rate and postoperative life quality. Superior petrous vein and greater superficial petrosal nerve should be managed properly in avoidance of postoperative complications. Finally, most meningioma inside cavernous sinus or adhered to brainstem could be totally removed without postoperative complications.
Key Words: Meningioma В· Petrous bone В· Neurosurgical procedures.
INTRODUCTION
Petrous apex meningiomas have puzzled neurosurgeons for decades due to their deep location and surrounding structures, namely carotid canal, Dorello canal, internal acoustic canal, subarcuate canal, and MeckelвҖҷs cave [ 1]. Permanent neural morbidity was reported up to 39.9% after resection of these rare tumors [ 4]. In recent years, extensive surgical approach was introduced to this area, such as transpetrosal, transcochlear, translabyrinthine, and suboccipital retrosigmoid approach [ 12, 15, 18, 19]. Among these surgical approaches mentioned above, the suboccipital retrosigmoid approach is popular and offer a wide range to achieve total removal. However, due to operation space is as narrow as 3 mm and operation distance is as deep as 10 cm, the suboccipital retrosigmoid approach isnвҖҷt suitable to remove meningioma hidden before brainstem. Transpetrosectomy approach which gave neurosurgeons a more anterior view compared to the the suboccipital retrosigmoid approaches and enabled neurosurgeons to operate before cranial nerves VII-XII rather than behind, was first described by Bochenek and Kukwa [ 2] in 1975. In 1991, Kawase et al. [ 9] modified this approach to operate on petroclival meningiomas by extradural drilling of the Kawase triangle. However, Xiao et al. [ 24] proposed that this extradural approach could cause postoperative cerebrospinal fluid leakage. Meanwhile, most tumor bases of petrous apex meningioma are located below trigeminal nerve, therefore neurosurgeons have to remove part of petrous bone to expose the tumor base in a risk of damaging carotid canal [ 3]. With usage of the intradural approach, neurosurgeons could remove less petrous bone than the extradural approach based on the location of the tumor base with a direct view [ 6]. Thus, the authors present the intradural modification of Kawase approach for petrous apex meningioma that have been performed from February 2012 to May 2017, and an analysis of the surgical results.
MATERIALS AND METHODS
General case information
From February 2012 to May 2017, we performed a retrospective analysis of 16 patients with petrous apex meningiomas who underwent the intradural transpetrosectomy practiced by the senior author in the department of neurosurgery at Renji Hospital. All procedures performed in the study involving human participants were in accordance with the ethical standards of Renji Hospital. And Institutional Review Board approval of Renj Hospital was obtained for this study. The case series consisted of six males and 10 females with a mean age of 43.5 years (range, 30-76). A summary of the clinical findings and signs were listed in Table 1. The mean duration of symptoms was 8.2 months (2-120 months). Of the 16 cases, seven were located in the left side and the remaining were located in the right side.
Imaging manifestations
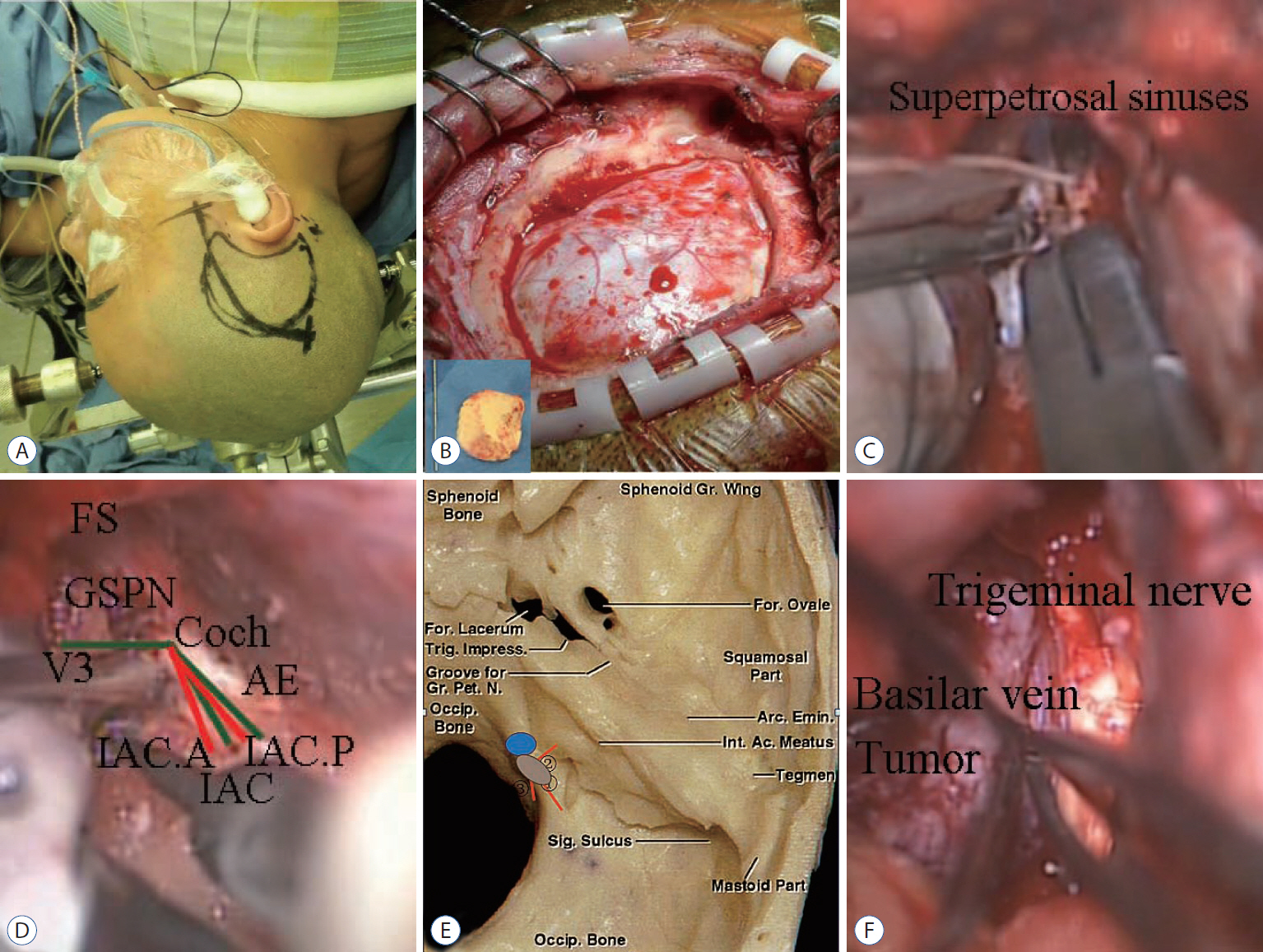
Contrast-enhanced computed tomography (CT) and magnetic resonance imaging (MRI) have been obtained in all patients ( Fig. 1A- C). Contrast-enhanced T1-weighted MRI gave the most accurate information for planning the surgical approach, including the dural attachment zone, maximal dimensions of the tumor, displacement of the brainstem, displacement or engulfment of the basilar arteries and invasion of the cavernous sinus. The maximal tumor dimensions ranged from 21 to 42 mm. Posterior cavernous sinus extension in six cases, displacement of basilar arteries in 10 cases and compression of the brainstem in 13 of the 16 cases were noted. T2-weighted MRI depicted the interface between the tumor and the brainstem, such as hyper-intensive signal within the brain parenchyma indicated disruption of the blood-brain barrier and difficulties in resecting the tumor from the brainstem might be anticipated. Tumor remnant was left in six patients due to these situations.
Surgical technique
The patient was placed in the lateral decubitus position with the ipsilateral shoulder slightly elevated ( Fig. 2A). The skin incision began 0.5 cm below the zygomatic arch, 1 cm anterior to superficial temporal artery, and extended 9 to 11 cm superoposteriorly based on the location of tumor. Then superficial and deep temporalis fascia and temporalis muscle was incised and elevated with a self-retaining retractor. Root of zygoma and suprameatal ridge were drilled separately. Next, bone flap was removed with rongeurs as needed to middle point of zygomatic arch anteriorly, intersection point of suprameatal ridge and extended line of zygomatic arch posteriorly, superior temporal line superiorly and zygomatic arch inferiorly, until bony opening was nearly flush with the floor of the middle cranial fossa ( Fig. 2B). Then, dura was open curvely and bottom of temporal lobe was elevated to expose tentorium. Dissected the arachnoid membranes of cistern ambiens and released cerebrospinal fluid. Incised tentorium behind the entrance of trochlear nerve. Freed superior petrosal sinus from superior petrosal sinus groove to clip it with titanium clips and ligated it later ( Fig. 2C). During surgery, we utilized technique of Garcia-Ibanez with the bisection of the angle between the GSPN and arcuate eminence to identify the direction of the internal acoustic canal ( Fig. 2D). To expose the tumor base, we have to removal part of petrous bone from the trigeminal nerve pressure trace to the internal auditory canal, not exceeding 1.5 cm laterally, from the petrous edge to the petrous section of internal carotid artery, not exceeding 2 cm anteriorly, and from the petrous tip to the petrosal sinus, not exceeding 1 cm inferiorly ( Fig. 2E). Tumor base of petrous apex meningioma was often found at the bottom dura of MeckelвҖҷs cave near superior petrous sinus, which should be coagulated before internal decompression was performed. Incised MeckelвҖҷs cave to resect residue tumor inside. Oculomoter nerve, trochlear nerve, abducens nerve, trigeminal nerve and facial nerve were often adhered to tumor ( Fig. 2F). Tumor was debulked with microscissor and aspirator by a piecemeal technique. After meticulous bleeding control, closure was performed in layers.
RESULTS
The intradural transpetrosectomy was performed in all 16 cases with brainstem auditory evoked potentials monitoring. In all patients, tumor removal was classified based on postoperative contrast-enhanced MRI ( Fig. 1D- F), and gross total resection was considered to be achieved if there was no enhancement present. According to Simpson grading system, grade I resection (tumor, dura, and bone) was achieved in four cases (25%). Grade II resection (tumor and dura) was achieved in six cases (37.5%) and there was no recurrence in this two group. Grade III resection (tumor) was achieved in six cases (37.5%) due to firm consistency and carvernous sinus invasion or brainstem adherence. Among this group, two patients experienced regrowth of the tumor which have been confirmed by the pathological results ( Fig. 3) and underwent a second operation. The postoperative complications improved during a mean follow-up period of 34.4 months (range, 6-66). The mean KPS improved from 85.6 preoperatively to 91.9 postoperatively, and all data was handled by SPSS version 20.0 for stastical analysis (SPSS Inc., Chicago, IL, USA). Using Wilcoxon rank testing indicated, the difference between preoperative and postoperative KPS score was statistically significant ( p=0.039).
DISCUSSION
The advantages of intradural transpetrosectomy approach compared to conventional Kawase approach are 1) an arc incision begins from 1 cm anterior to superficial temporal artery and stops above the auricle in intradural transpetrosectomy with a nicer appearance and shorter operation time, compared with a rectilinear incision around the ear in conventional Kawase approach. 2) Temporalis muscle is retracted bilaterally in intradural transpetrosectomy approach which can better neurosurgeonвҖҷs vision of middle fossa, compared with temporalis muscle reflected inferiorly in conventional Kawase approach. And 3) middle meningeal artery and dorsal meningeal artery are exposed better and earlier. After obstructing the blood supply of petrous apex meningiomas, tumor will be easily resectable and surrounding structures can be protected during the process.
In this intradural transpetrosectomy, there is still debates regarding several steps and willed be discussed as followed. First, could superior petrous vein (SPV) be sacrificed? Superior petrous vein normally works as the drainage route from anterior cerebellar and brainstem venous system, which has four tribulates including anterior pontomesencephalic group, posterior mesencephalic group, tentorial group and petrosal group. If there is not enough space for operation, neurosurgeons should sacrifice veins after assessing the size of the veins [ 4]. Zhong et al. [ 26] claimed that veins with a diameter less than 2 mm could be coagulated and cut without risk. The vein of the cerebellopontine fissure, which has a diameter of 2.6 cm as the largest common stem of SPVs in the petrosal group, is often found coursing along the posterior surface of petrous apex meningiomas and should not be sacrificed. Conversely, the tributaries of the tentorial group or the posterior mesencephalic group could be sacrificed [ 13]. Besides, the superior petrosal vein is either displaced or compressed by meningioma, resulting in the formation of collateral veins, and therefore superior petrosal vein can be safely sacrificed in such cases [ 17, 20]. No patient in this study developed a severe ipsilateral cerebellar edema or brainstem shift due to occlusion of the superior petrous vein. Second, how to dissect greater superficial petrosal nerve? Back-to-front or front-to-back? Greater superficial petrosal nerve (GSPN) is an important landmark for identifying internal acoustics canal and drilling petrous bone. GSPN are prone to injuries during drilling as it courses to the geniculate ganglion, which could cause facial nerve palsy. Traditional surgical literature recommends to dissect GSPN from back-to-front, but it is infeasible to control traction forces on the proximal portion of the GSPN, including the geniculate ganglion [ 23, 25]. On the other hand, front-to-back dissection has some advantages. At foramen ovale which is easily identified, it is simple to dissect the cleavage plane between the meningeal dura and the outer dura. Following trigeminal nerve from foramen ovale, the dura portion of the GSPN is located 7.5 mm medially and outer dural layer can be readily elevated from GSPN. Neural tissue is protected because front-to-back dissection leaves a defined endosteum coving the GSPN [ 8]. Third, should meningioma inside cavernous sinus or adhered to brainstem be totally removed? Most neurosurgeons worried that removing tumors in these places would cause paralysis of cranial nerves, especially glossopharyngeal nerve and vagus nerve [ 16]. Besides, neurosurgeons even like Sammi believed few patients with a efficacious subtotal removel had clinical progression and death [ 19]. However, a study lasting more than 4 years indicated that overal growth rates of petroclival menigiomas in patients managed conservatively were 0.81 mm/year in diameter [ 14]. In addition, meningioma in cavernous sinus and brainstem isnвҖҷt often adhered tightly to the surrounding tissues and solid in consistency, so the preferred choice is complete resection of meningioma. Meanwhile, radiotherapy for meningioma could induce intratumoral necrosis, peritumoral edema and second malignancy, so the preferred choice is complete resection of meningioma [ 10, 11]. Intradural transpetrosectomy is ideal for petrous apex meningioma, especially for those with a predominant middle fossa extension, which can save much time to expose tumors and provide more surgical freedom when dealing with trigeminal nerve as compared with standard retrosigmoid approach [ 21]. But this approach is not ideal for tumors at the posterior fossa, because bone window is relatively small to provide space as a corridor to the posterior fossa [ 7, 22]. Furthermore, it is not ideal for tumors at sella region and cerebellopontine angle due to the vein of Labbe on the dominant side being at high risk of injury, which is the main reason for temporal edema and postsurgical bleeding.
CONCLUSION
The intradural transpetrosectomy is an intradural modification of the conventional Kawase approach with less complications and better visions compared with the conventional Kawase approach, which is ideal for petrous apex meningioma. During this approach, superior petrous vein could be sacrificed except the vein of the cerebellopontine fissure and the common stem. Dissecting greater superficial petrosal nerve by front-to-back is recommended with less traction injuries. Meanwhile, most meningioma inside cavernous sinus or adhered to brainstem could be totally removed.
Acknowledgements
The work has been funded by Chinese National Natural Science Foundation (81471333).
Fig.В 1.
A : Preoperative MRI, axial view : an enhanced petrous apex meningioma was seen around the right MeckelвҖҷs cave and extend into the supratentorial region. B : Preoperative CT : relationship between bone and tumor. C : Preoperative 3D-CT angiography : right posterior cerebral artery was compressed and replaced superior to the tumor. D : Postoperative MRI : no residual tumor. E : Postoperative CT : the drilling extent of petrous bone. F : Postoperative 3D-CT reconstruction : bone flap was placed back. MRI : magnetic resonance imaging, CT : computed tomography. 
Fig.В 2.
A : PatientвҖҷs position and skin incision. B : The size of bone flap. C : Superior petrosal sinus groove was clipped with titanium clips. D : Identified the internal auditory canal by Garcia-Ibanz method [ 5]. E : Drilling extent. в‘ 1.5 cm : from the trigeminal nerve pressure trace to the internal auditory canal; в‘Ў 1.0 cm : from the petrous edge to the petrous section of internal carotid artery; в‘ў 1.0 cm : from the petrous tip to the petrosal sinus. F : Separated neurovascular structures from tumor. FS : foramen spinosum, GSPN : greater superficial petrosal nerve, AE : arcuate eminence, IAC : internal auditory canal, Gr. : great, For. : foramen, Trig. : trigminal, Pet. : petrosal, N. : nerve, Occip. : occipital, Arc. : arcuate, Emin. : eminece, Int. : internal, Ac. : arcuate, Sig. : sigmoid. 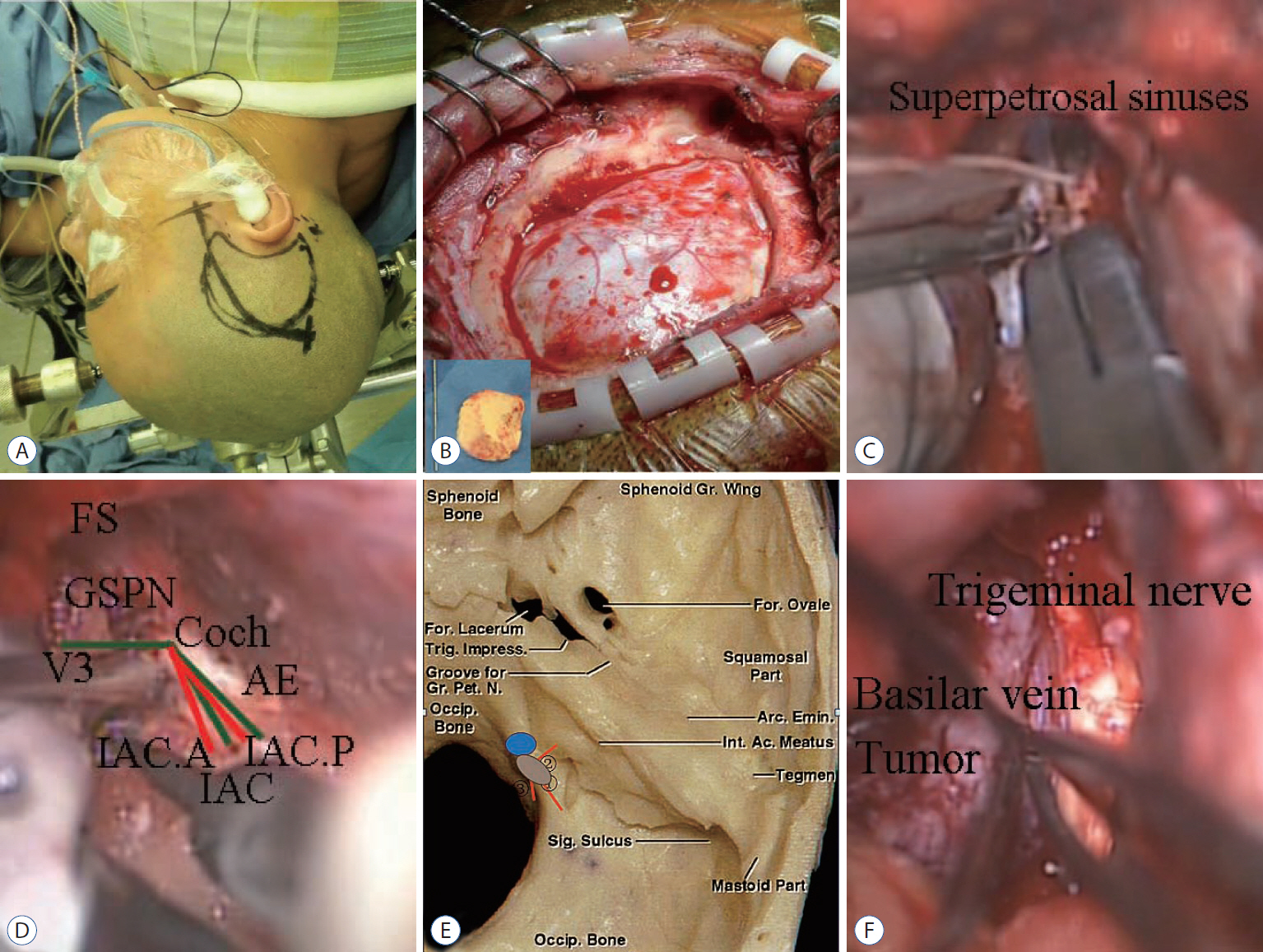
Fig.В 3.
Histological examination of meningioma following hematoxylin and eosin staining (Г—200). 
TableВ 1.
Characteristics of patients who underwent intradural transpetrosectomy for petrous apex meningiomas
|
Case |
Age/sex |
Tumor size (mm) |
Chief complaint |
Preopscore |
Scale by Simpson |
Complications |
Postop score |
Progression-free survival (months) |
|
1 |
40/F |
21 |
Headache |
100 |
I |
|
100 |
Censored obsevations |
|
2 |
36/M |
24 |
Headache |
100 |
I |
|
100 |
Censored obsevations |
|
3 |
50/M |
28 |
Headache |
100 |
II |
Facial numbness |
90 |
Censored obsevations |
|
4 |
38/M |
25 |
Diplopia |
90 |
II |
|
100 |
Censored obsevations |
|
5 |
34/F |
31 |
Facial numbness |
90 |
II |
|
100 |
Censored obsevations |
|
6 |
41/F |
31 |
Headache, facial numbness |
90 |
II |
|
100 |
61 |
|
7 |
30/F |
24 |
Facial numbness |
90 |
I |
|
100 |
Censored obsevations |
|
8 |
33/M |
27 |
Headache, facial numbness |
90 |
II |
Facial numbness |
90 |
48 |
|
9 |
45/F |
30 |
Headache, facial numbness |
90 |
II |
Facial numbness |
90 |
Censored obsevations |
|
10 |
43/F |
35 |
Headache, facial numbness |
90 |
III |
Facial numbness |
90 |
Censored obsevations |
|
11 |
38/M |
30 |
Facial numbness |
90 |
I |
Hydrocephalus |
80 |
Censored obsevations |
|
12 |
38/F |
28 |
Hearing disturbance |
80 |
III |
|
100 |
35 |
|
13 |
43/M |
35 |
Hearing disturbance |
80 |
III |
Facial numbness |
90 |
23 |
|
14 |
62/F |
35 |
Headache, diplopia |
80 |
III |
Diplopia |
80 |
43 |
|
15 |
49/F |
38 |
Headache, vision |
70 |
III |
|
100 |
11 |
|
16 |
76/F |
42 |
Headache, ision fading, ataxia |
40 |
III |
Hemiparesis, cerebrospinal fluid leak |
60 |
Censored obsevations |
References
1. Altieri R, Sameshima T, Pacca P, Crobeddu E, Garbossa D, Ducati A, et al : Detailed anatomy knowledge: first step to approach petroclival meningiomas through the petrous apex. Anatomy lab experience and surgical series. Neurosurg Rev 40 : 231-239, 2017    2. Bochenek Z, Kukwa A : An extended approach through the middle cranial fossa to the internal auditory meatus and the cerebello-pontine angle. Acta Otolaryngol 80 : 410-414, 1975   3. Borghei-Razavi H, Tomio R, Fereshtehnejad SM, Shibao S, Schick U, Toda M, et al : Anterior petrosal approach: The safety of Kawase triangle as an anatomical landmark for anterior petrosectomy in petroclival meningiomas. Clin Neurol Neurosurg 139 : 282-287, 2015   4. Cui H, Zhou CF, Bao YH, Wang MS, Wang Y : Extended suboccipital retrosigmoid surgical approach is effective for resection of petrous apex meningioma. J Craniofac Surg 27 : e429-e433, 2016  5. Garcia-Ibanez E, Garcia-Ibanez JL : Middle fossa vestibular neurectomy: a report of 373 cases. Otolaryngol Head Neck Surg 88 : 486-490, 1980   6. Ichimura S, Hori S, Hecht N, Czabanka M, Vajkoczy P : Intradural anterior transpetrosal approach. Neurosurg Rev 39 : 625-631, 2016   7. Janjua MB, Caruso JP, Greenfield JP, Souweidane MM, Schwartz TH : The combined transpetrosal approach: Anatomic study and literature review. J Clin Neurosci 41 : 36-40, 2017   8. Jittapiromsak P, Sabuncuoglu H, Deshmukh P, Nakaji P, Spetzler RF, Preul MC : Greater superficial petrosal nerve dissection: back to front or front to back? Neurosurgery 64( 5 Suppl 2):253-258; discussion 258-259, 2009    9. Kawase T, Shiobara R, Toya S : Anterior transpetrosal-transtentorial approach for sphenopetroclival meningiomas: surgical method and results in 10 patients. Neurosurgery 28 : 869-875; discussion 875-876, 1991   12. Li D, Tang J, Ren C, Wu Z, Zhang LW, Zhang JT : Surgical management of medium and large petroclival meningiomas: a single institutionвҖҷs experience of 199 cases with long-term follow-up. Acta neurochir (Wien) 158 : 409-425; discussion 425, 2016    13. Matsushima T, Kawashima M, Inoue K, Matsushima K : Anatomy of the superior petrosal veins and their exposure and management during petrous apex meningioma surgery using the lateral suboccipital retrosigmoid approach. Neurosurg Rev 37 : 535-456, 2014    15. Miller ME, Mastrodimos B, Cueva RA : Facial nerve function after the extended translabyrinthine approach. J Neurol Surg B Skull Base 76 : 1-6, 2015   16. Morisako H, Goto T, Ohata K : Petroclival meningiomas resected via a combined transpetrosal approach: surgical outcomes in 60 cases and a new scoring system for clinical evaluation. J Neurosurg 122 : 373-380, 2015  18. Ohata K, Haque M, Morino M, Nagai K, Nishio A, Nishijima Y, et al : Occlusion of the sigmoid sinus after surgery via the presigmoidal-transpetrosal approach. J Neurosurg 89 : 575-584, 1998   19. Samii M, Ammirati M, Mahran A, Bini W, Sepehrnia A : Surgery of petroclival meningiomas: report of 24 cases. Neurosurgery 24 : 12-17, 1989  20. Sharma M, Ambekar S, Guthikonda B, Nanda A : A Comparison between the Kawase and extended retrosigmoid approaches (Retrosigmoid transtentorial and retrosigmoid intradural suprameatal approaches) for accessing the petroclival tumors. A cadaveric study. J Neurol Surg B Skull Base 75 : 171-176, 2014   21. Shibao S, Borghei-Razavi H, Orii M, Yoshida K : Anterior transpetrosal approach combined with partial posterior petrosectomy for petroclival meningiomas with posterior extension. World neurosurg 84 : 574-579, 2015   22. Tripathi M, Deo RC, Suri A, Srivastav V, Baby B, Kumar S, et al : Quantitative analysis of the Kawase versus the modified Dolenc-Kawase approach for middle cranial fossa lesions with variable anteroposterior extension. J Neurosurg 123 : 14-22, 2015  23. Tummala RP, Coscarella E, Morcos JJ : Transpetrosal approaches to the posterior fossa. Neurosurg Focus 19 : E6, 2005  24. Xiao X, Zhang L, Wu Z, Zhang J, Jia G, Tang J, et al : Surgical resection of large and giant petroclival meningiomas via a modified anterior transpetrous approach. Neurosurg Rev 36 : 587-593; discussion 593-594, 2013   25. Youssef S, Kim EY, Aziz KM, Hemida S, Keller JT, van Loveren HR : The subtemporal interdural approach to dumbbell-shaped trigeminal schwannomas: cadaveric prosection. Neurosurgery 59( 4 Suppl 2):ONS270-ONS277, 2006   26. Zhong J, Li ST, Xu SQ, Wan L, Wang X : Management of petrosal veins during microvascular decompression for trigeminal neuralgia. Neurol Res 30 : 697-700, 2008 
|
|