INTRODUCTION
Myofibroblasts are spindle mesenchymal cells sharing features of both muscular and fibroblastic cells6) and represent a connective tissue cell characterized by morphologic and functional properties intermediate between fibroblasts and smooth muscle cells3). Low-grade myofibroblastic sarcoma (LGMS) represents a distinct atypical myofibroblastic tumor with fibromatosis like features and has a predilection for the head and neck, particularly the tongue and oral cavity2,8). More than 80% of malignant tumors of the head-and-neck region originate from squamous epithelium. Therefore, the incidence of mesenchymal tumors is low. Among them, myofibroblastic sarcomas are extremely rare7,12). Jay et al.5) reviewed in the literature that reported 22 cases (including their cases) myofibroblastic sarcomas in the oral cavity and maxillofacial region. Among them, 6 cases occur in tongue. Five (24%) cases showed local recurrence and one case distant metastases during follow up period.
We describe a case of LGMS occurring in the scalp of a 26-year-old man and review this rare entity tumor in the literatures.
CASE REPORT
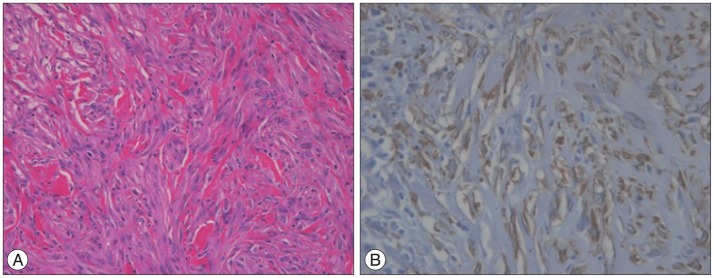
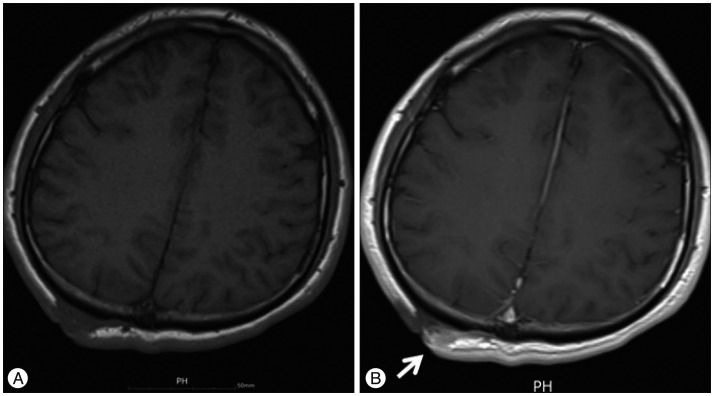
A 26-year-old man presented with a 12-month history of a slow growing palpable hard mass in the right parietal scalp. He had no past history of scalp trauma or neoplasm. On physical examination, there was a 3Г—4 cm hard mass that was mild tenderness. Enhanced computed tomography (CT) scanning of head showed a well-defined and heterogeneously enhancing scalp mass (Fig. 1). The patient underwent excision of the tumor with macroscopically clear margins. The mass was relatively well-circumscribed, firm, and grayish with fibrous. Histological examination revealed a spindle cell tumor with interspersed collagen bundles. The spindle cells show moderate degree of nuclear pleomorphism (Fig. 2A). A mitotic count was 1 to 2 per 10 high power fields (HPFs). There was no necrosis or multinucleated giant cells in the numerous sections. The spindle cells were found to be positive for s Оұ-smooth muscle actin (Fig. 2B) and negative for desmin, S-100 protein, epithelial membrane antigen and CD34 on immunohistochemistry. Ki-67 labeling index was at 10%. Ultrathin section shows oval and spindle cells having scant cytoplasm. The tumor cells showing scant organelles except dilated rough endoplasmic reticulum. There are primitive intercellular junctions with cytoplasmic dense bodies (Fig. 3). All of features were consistent with a LGMS. After confirmed a diagnosis, we performed a brain magnetic resonance image (MRI) for finding a possible remnant tumor. T1 weighted image (T1WI) axial brain MRI showed iso-signal intensity remnant mass in right parietal scalp (Fig. 4A). Gadolinium enhancement T1WI axial brain MRI showed the heterogeneously enhancing mass, which was measured 0.3Г—1 cm (Fig. 4B). We performed re-operation for remnant tumor removal. Postoperative course was uneventful. No adjuvant radiotherapy and chemotherapy should be applied. Regular follow-up showed no sign of recurrence. After 14 months of surgery, follow up brain MRI showed no evidence of recurred lesion in scalp (Fig. 5). 18FDG-PET CT scan demonstrated no abnormal hot uptake in the body. The patient was well-being state.
DISCUSSION
LGMS is a recently defined tumor that can be considered a part of the spectrum of malignant mesenchymal tumors, showing features of myofibroblastic differentiation11). Myofibroblasts have been recognized for over three decades, but the existence of sarcomas composed of myofibroblasts has become generally accepted recently8). Myofibroblastic sarcoma must be distinguished from other neoplasms, which including nodular fasciitis, proliferative myositis and fibromatosis, and also other types of low-grade spindle-cell sarcomas, leiomyosarcoma and fibrosarcoma10). Mentzel et al.7) characterized myofibrosarcoma or myofibroblastic sarcoma as a spindle cell sarcoma composed of myofibroblasts. They summarized clinical findings of LGMS patients, which data show that the age of the patients ranged between 19 and 72 years (median : 42 years). Male to female ratio is 1.57. In most cases, patient complained of a painless swelling or an enlarging mass7).
The diagnosis of LGMS is made on the basis of ultrastructual findings as determined by light microscopy and immunocytochemistry.
LGMS is composed of slender spindle cells arranged in interlacing fascicles. LGMS have a mild to moderate amount of eosinophilic or amphophilic cytoplasm and fusiform nuclei, and usually characterized with mild nuclear pleomorphism and low mitotic rate (1-6/10 HPFs)12). Our case shows 1 to 2 per 10 HPFs of mitotic rate and moderate pleomorphism of spindle cells.
LGMS tumors cells express strong positive immunoreactivity for at least one of following myogenic markers that muscle-specific actin (HHF35), Оұ-smooth muscle actin, rarely desmin1,78,1112). LGMS may also express focal expression of CD34 and CD998). The tumors do not stain for S-100 protein, epithelial markers such as laminin and h-caldesmon4,812). Our case is negative for CD34 and desmin but positive for Оұ-smooth muscle actin.
LGMS usually affects deep soft tissue sites and is more often poorly circumscribed with fascicles and individual cells infiltrating between muscle fibers, although focal circumscription is not unusual4,5).
The treatment of this rare tumor should include a simple local excision with wide surgical margins and adjuvant therapies such as chemotherapy or radiotherapy have also been used in some cases9,1112).
Local recurrences are common in LGMS, but metastases occur only rarely7,8). Follow-up information is limited in the literature, but multiple soft tissues, bone, and pulmonary metastases from a chest wall mass were reported5). Therefore, LGMS are needed years of clinical follow-up evaluation including scans11).