Jang, Choi, Nam, Park, and Kwon: Arachnoid Plasty to Prevent and Reduce Chronic Subdural Hematoma after Clipping Surgery for Unruptured Intracranial Aneurysm : A Meta-Analysis
Abstract
Objective
Recent studies have reported that arachnoid plasty (ARP) using gelatin sponges with fibrin glue reduced the occurrence of chronic subdural hematoma (CSDH) following clipping surgery for unruptured intracranial aneurysm (UIA). This meta-analysis was conducted to collate further evidence for the efficacy of ARP in preventing postoperative CSDH.
Methods
Data of patients who underwent clipping surgery were extracted from PubMed, EMBASE, and Cochrane Central Register of Controlled Trials by two independent reviewers. A random effects model was used to investigate the efficacy of ARP by using odd ratios (ORs) and 95% confidence intervals (CIs). A meta-regression analysis for male sex was additionally preformed.
Results
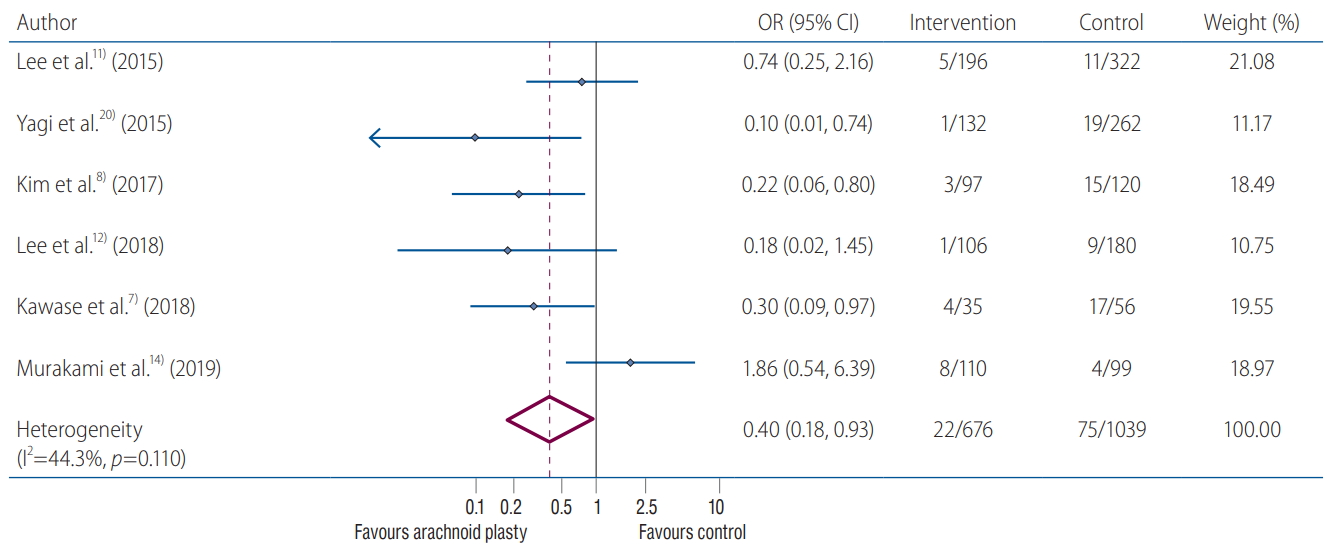
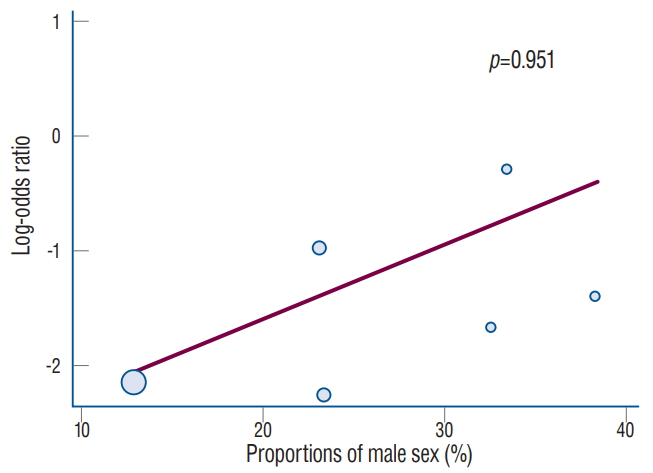
Data from six studies with 1715 patients were consecutively included. Meta-analysis revealed that ARP was significantly associated with lower rates of CSDH development after surgical clipping for UIA (ARP group vs. control group : 3.2% vs. 7.2%; OR, 0.40; 95% CI, 0.18-0.93; I2 =44.3%; p=0.110). Meta-regression analysis did not highlight any modifying effect of the male sex on postoperative CSDH development (p=0.951).
Conclusion
This meta-analysis indicated that ARP reduced the incidence rates of CSDH following clipping surgery for UIA. If feasible, ARP would be implemented as an additional surgical technique to prevent postoperative CSDH development during surgical clipping of UIA.
Key Words: Aneurysm · Surgery · Hematoma, Subdural, Chronic · Arachnoid.
INTRODUCTION
Surgical clipping is an effective treatment modality for unruptured intracranial aneurysm (UIA). Overall advancements in microsurgical techniques have markedly reduced postoperative complications. However, chronic subdural hematoma (CSDH) is one of the challenging postoperative complications for UIA clipping [ 13, 15], and the incidence of CSDH development after the surgery ranges from 0.9% to 5.1% [ 3, 11, 15, 16]. Although postoperative CSDH shows a relatively benign clinical course with spontaneous resolution, it sometimes required surgical treatment to relieve mass effect. There are many known risk factors for CSDH after surgical clipping, such as age, brain atrophy, anticoagulant medication, and postoperative subdural air; however, its underlying mechanism remains poorly understood [ 3, 6, 8, 16]. Recent studies reported that increased subdural fluid collection could also be a significant risk factor for postoperative CSDH [ 14, 16]. Previous studies have reported that arachnoid plasty (ARP) with fibrin glue and gelatin sponge has been helpful in the prevention of postoperative CSDH via reducing subdural fluid collection. However, the effectiveness of ARP has not been fully validated [ 7, 8, 11- 14, 20]. Therefore, we aimed to collate the available evidence on the efficacy of ARP in prevention of CSDH after surgical clipping of UIA with a meta-analysis of the relevant clinical studies.
MATERIALS AND METHODS
A study of this type, such as meta-analysis, does not require informed consent or Institutional Review Board’s approval. This study was conducted and documented in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines ( Supplementary Table 1). The supplementary material describes the methods of this study in detail.
Data sources and searches
PubMed, EMBASE, the Cochrane Central Register of Controlled Trials, and relevant web sites were systematically searched for relevant articles including randomized controlled trials and retrospective observational studies. The organized search strategy was established per the Population, Intervention, Comparison and Outcome (PICO) format [ 17] with systematic and concrete terms supplemented with keywords ( Supplementary Table 2). Additional electronic search strategy was complemented by a manual screening of bibliographies of full-text articles such as recent reviews, editorials, and meta-analyses. There were no restrictions on the language of publication, study period, or sample size.
Eligibility criteria and study selection
The articles identified by the search strategy were subjected to the following inclusion criteria : 1) enrolled patients who underwent surgery with clipping for UIA; 2) surgery with craniotomy such as the pterional or supraorbital approach; 3) patients with additional ARP closing the sylvian cistern after aneurysmal repair; 4) studies presenting CSDH development as the outcome regardless of ARP implementation; and 5) articles presenting controls as patients with unexecuted ARP. We excluded studies that : 1) were technical notes, case reports, conference abstracts, study protocols, or editorial letters; 2) enrolled patients who underwent surgery for ruptured intracranial aneurysm (RIA); 3) included participants having non-aneurysmal subarachnoid hemorrhage or intracerebral hemorrhage; and 4) presented not CSDH but subdural effusion as the comparable outcome for ARP. Two different authors (KMJ and HYM) independently screened the abstracts titles, identified duplicates, reviewed full-text articles, and determined their eligibility for inclusion in the meta-analysis. In case of a disagreement between the reviewers, consensus was sought through a discussion with the corresponding author.
Data extraction and quality assessment
Data were obtained independently in duplicate by two authors using a standardized form for extracting study characteristics, design, sample size, age, sex, surgical method, number of patients that underwent surgery with ARP, technique for ARP, and aneurysmal characteristics (e.g., rupture and/or locations). In addition, the authors investigated the prescriptions given before the surgery including antiplatelet and anticoagulant medication.
The authors established that the outcome was postoperative CSDH by referring to new occurrence of symptomatic CSDH after clipping surgery in patients without any history of traumatic brain injury at the latest available follow-up time point. Requiring additional surgery was not considered in establishing the outcome.
The quality of eligible studies was assessed using the Newcastle-Ottawa Scale (NOS) for non-RCTs and retrospective studies. Both authors assessed the study quality on the basis of eight items within three different categories : selection, comparability, and outcome. We did not rule out articles in accordance with the thresholds of NOS checklists.
Data analysis
Statistical analysis was performed using Review Manager and STATA/SE 15.0 (Stata Corp LP, College Station, TX, USA). Postoperative CSDH development according to ARP implement was considered the main outcome, analyzed using the random effects model with generic inverse variance method, and presented with the odds ratio (OR) and 95% confidence interval (CI) as a summary statistic. We excluded data presented as medians with interquartile range and those that did not report the standard deviation values. To homologate the results and make them comparative, an analysis for articles with only UIA was conducted. Sensitivity analysis was carried out with all except one study that showed a high risk of bias. Meta-regression analysis for male sex, a proven risk factor for CSDH, was additionally conducted.
Statistical heterogeneity was estimated using the I2 statistic, to evaluate the degree of inconsistency across studies in the meta-analysis. I2 <25%, <50%, and >75% were considered to indicate low, moderate, and severe heterogeneity, respectively. The authors investigated publication bias by visual asymmetry of funnel plots and Egger’s and Begg’s tests. Two-sided p-values <0.05 were considered to indicate statistical significance.
RESULTS
Search results and risk of bias within studies
From the initial 355 candidate articles (180 in PubMed, 173 in Embase, and two in the Cochrane Central Register) found via the systematic literature search, 128 duplicates were removed. Of the remaining 227 articles, 14 were extracted for full article review by screening the titles and abstracts ( Supplementary Table 3). Finally, six articles fulfilled the eligibility criteria for inclusion ( Fig. 1). Based on the quality of eligible studies per the NOS checklist, the majority of included studies ranged from having low to moderate risk of bias. However, we determined that the risk of bias was high only in one study and performed an additional sensitivity analysis after excluding that study. The NOS data presenting individual judgments for risk of bias are documented in Supplementary Table 4.
Study characteristics
The six studies with a total of 1715 patients that underwent clipping surgery and reported CSDH development as the primary outcome were included in this pooled analysis. All six articles were single-center, retrospective case-control studies. Further, all six studies analyzed patients with UIA. Regarding the surgical methods, the supraorbital and pterional approach were used in one and three studies, respectively. One study used both approaches in accordance with clinical perspectives. The incidence rate of overall postoperative CSDH development was 5.7% (97/1715). The implementation rates of pterional and supraorbital approach were 67.2% (1092/1624) and 32.8% (532/1624), respectively, except for the Kawase trial, which did not provide information on the approach used. Among the five studies with available data for ARP techniques, the procedure was performed using gelatin sponge with fibrin glue in three studies, while oxidized cellulose with glue was used in the remaining two. The gelatin sponge with glue was more frequently applied in the ARP procedure than oxidized cellulose (55.2% vs. 44.8%, respectively) Regarding overall baseline demographics, female patients were included relatively more than males (69.6% vs. 30.4%, respectively). The baseline characteristics of the six individual studies are summarized in Table 1.
CSDH development after clipping for UIA
The ARP implementation rates after clipping surgery for UIA was 39.4% (676/1715). The incidence rate of overall postoperative CSDH development was 5.7% (97/1715). Additionally, the CSDH rates from the pooled analysis were 3.2% (22/676) in the ARP group and 7.2% (75/1039) in the control group. Integrating the results of the six included studies showed that UIA clipping surgery with ARP was significantly associated with a reduced risk of postoperative CSDH development compared to the control (pooled OR, 0.40; 95% CI, 0.18-0.93; I 2=44.3%; p=0.110) ( Fig. 2). Despite visual asymmetry in the funnel plot, noticeable publication bias was not identified with the Egger’s and Begg’s tests ( p=0.225 and p=0.260, respectively) ( Supplementary Fig. 1).
Sensitivity analysis
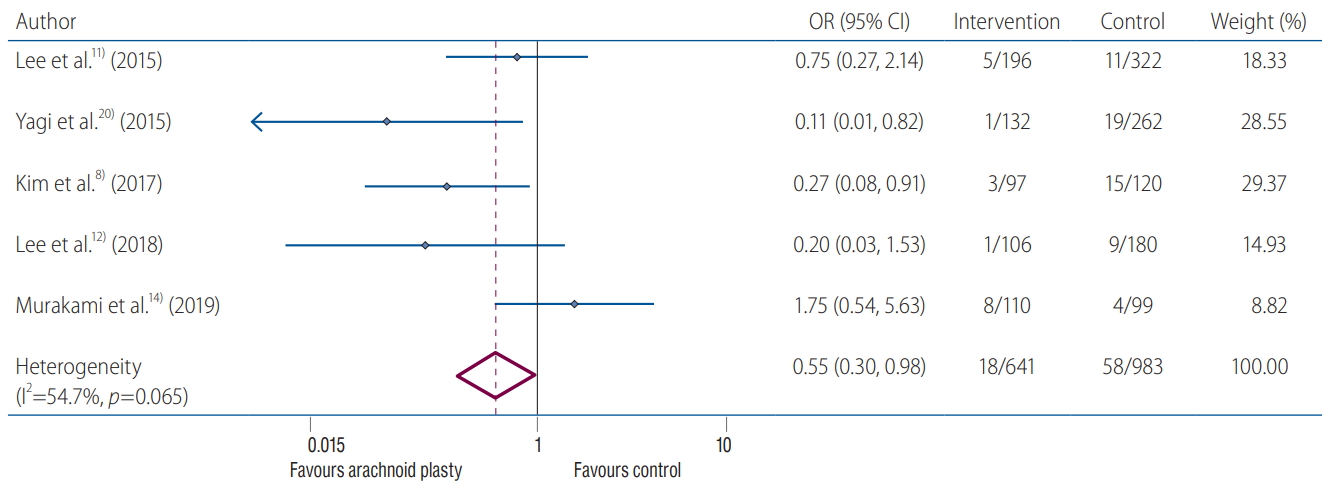
An additional sensitivity analysis was conducted after exclusion of the Kawase 2018 trial that had a high risk of bias according to the NOS checklist. The result was in line with the integrated analysis and indicated that the ARP was significantly associated with lowering CSDH development after surgery (pooled OR, 0.55; 95% CI, 0.30-0.98; I 2=54.7%; p=0.065) ( Fig. 3). In addition, meta-regression analysis did not highlight any modifying effect of male sex on postoperative CSDH development ( p=0.951) ( Fig. 4).
DISCUSSION
This meta-analysis contained integrated data from 1715 patients treated for UIA by clipping surgery, and revealed that implementation of ARP was associated with prevention of postoperative CSDH development. Furthermore, male sex was not a confounding factor between ARP application and CSDH development. There results provided further evidence that ARP following the surgery would be effective in prevention and reduction for postoperative CSDH development.
CSDH after aneurysmal clipping surgery is a relatively common complication, and sometimes requires additional surgical evacuation. The reported incidence rates of CSDH are 2.8% in UIA and 0.9% in RIA [ 15]. Kwon et al. [ 9] also reported higher incidence rates of CSDH in UIA than RIA (10.9% vs. 3.1%, respectively). To explain this difference, the author suggested two possible mechanisms : one entails the potential subdural space obliteration by the residual hematoma with brain edema, and the other is the osmotic gradient theory of the CSDH likely contributing to lower incidence rates [ 2]. The wall of CSDH is composed of two layers with semi-permeable membranes, and the hematoma gradually increases in size because of the difference between the internal and external osmotic pressures [ 1, 18, 21]. Accordingly, increased internal pressure reduces the pressure gradients, ultimately leader to lesser rate of CSDH and effectiveness of ARP in patients with RIA. Therefore, we investigated the effectiveness of ARP in surgical treatment of UIA, but excluded RIA, to homologate the results from this meta-analysis. Increased postoperative subdural fluid collection was a sole predictor for postoperative CSDH [ 14]. Park et al. [ 16] stated that advanced age, male sex, and deep location of the aneurysm were correlated with the occurrence of subdural fluid collection and CSDH after clipping surgery for UIA. The authors suggested that the possible mechanism of correlation was through a one-way valve phenomenon [ 10, 22]. Clipping surgery requires the dissection of the arachnoid membrane covering the sylvian fissures. Therefore, a persistent opening state of the subarachnoid space causes communication between the cerebrospinal fluid (CSF) cistern and subdural space. The healing process of the injured membrane induces the one-way valve from the subarachnoid to the subdural space, and results in persistent CSF leakage, eventually leading to CSDH development. Several additional studies also supported the correlation between subdural fluid collection and CSDH [ 4, 5, 8, 9, 14]. Therefore, ARP implementation can likely be considered to inhibit persistent CSF leakage, to essentially reduce postoperative CSDH development. The current study also observed that patients with ARP showed a lower incidence of CSDH than the controls; hence, we believe our results have provided further evidence to demonstrate the effectiveness of ARP in prevention of postoperative CSDH. The ARP technique using fibrin glue was first introduced by Tsuruno [ 19] in 1995. Since then, it has been developed into a technique that combines gelatin sponge or oxidized cellulose to enhance the sealing effect; more recently, a modified ARP technique using multiple gelatin pieces has also been introduced [ 12]. In this meta-analysis, gelatin sponge with fibrin glue and oxidized cellulose with the glue were applied in 55.2% and 44.8% cases, respectively. Although we were unable to clarify which of the two methods was more effective, we believe that ARP implementation could be an effective prevention method for postoperative CSDH development, and thus helpful to neurosurgeons conducting clipping surgery for UIA. Male sex has been associated with brain atrophy and recognized as presenting a higher risk of postoperative CSDH than females [ 12, 16, 20]. However, Murakami et al. [ 14] recently reported that male sex did not show a significant relationship with CSDH and that only subdural fluid collection was the sole risk factor. According to our results incorporating six studies with 1715 patients, male sex did not highlight any modifying effect between ARP and CSDH. Several limitations should be noted in this meta-analysis. First, our results should be interpreted with caution, given that they were not based on a relatively high level of evidenced studies. In other words, all individual studies were designed retrospectively, with relatively low level evidence of single-institutional study. Although we utilized a concrete search strategy, prospective, randomized-controlled, multi-center studies on ARP could not be identified. Second, this analysis was conducted on studies that had inconsistent protocols, such as those for the ARP techniques. Although there were minor differences in the detailed techniques, there was no significant difference in the method of using space-occupying substances with sealing materials such as fibrin glue gelatin sponges. Therefore, it was not assumed to cause fundamentally confounding errors. Last, patient age that is recognized as the major predictor of CSDH development was excluded in this analysis. Because most of the included studies did not provide overall and baseline patient age [ 6, 16], we tried to reveal the correlation between the age and postoperative CSDH, but could not extract this information. Therefore, prospective, multicenter, and centrally adjudicated studies with completely matched patient characteristics are required to further validate our findings.
CONCLUSION
ARP implementation showed effectiveness in reduction of CSDH development following clipping surgery for UIA. If feasible, ARP implementation would be considered as an additional surgical technique to prevent postoperative CSDH development during surgical clipping of UIA.
Acknowledgements
This research was supported by the Chung-Ang University Research Grants in 2019.
Supplementary Materials
Supplementary Table 1.
Checklist of items to include when reporting a systematic review or meta-analysis (PRISMA guideline)
jkns-2020-0036-supple1.pdf
Supplementary Table 2.
Search strategy in accordance with the Population, Intervention, Comparison and Outcome (PICO) format
jkns-2020-0036-supple2.pdf
Supplementary Fig. 1.
Funnel plots for evaluating publication bias. Funnel plot revealed that there was no evidence for publication bias of across the direct comparisons between arachnoid plasty group and control in patients underwent clipping surgery for unruptured intracranial aneurysm. s.e. : standard error.
jkns-2020-0036-supple5.pdf
Fig. 1.
Flow diagram for the selection of relevant studies. 
Fig. 2.
Efficacy of arachnoid plasty in the chronic subdural hematoma reduction after clipping surgery for unruptured intracranial aneurysm. OR : odds ratio, CI : confidence interval. 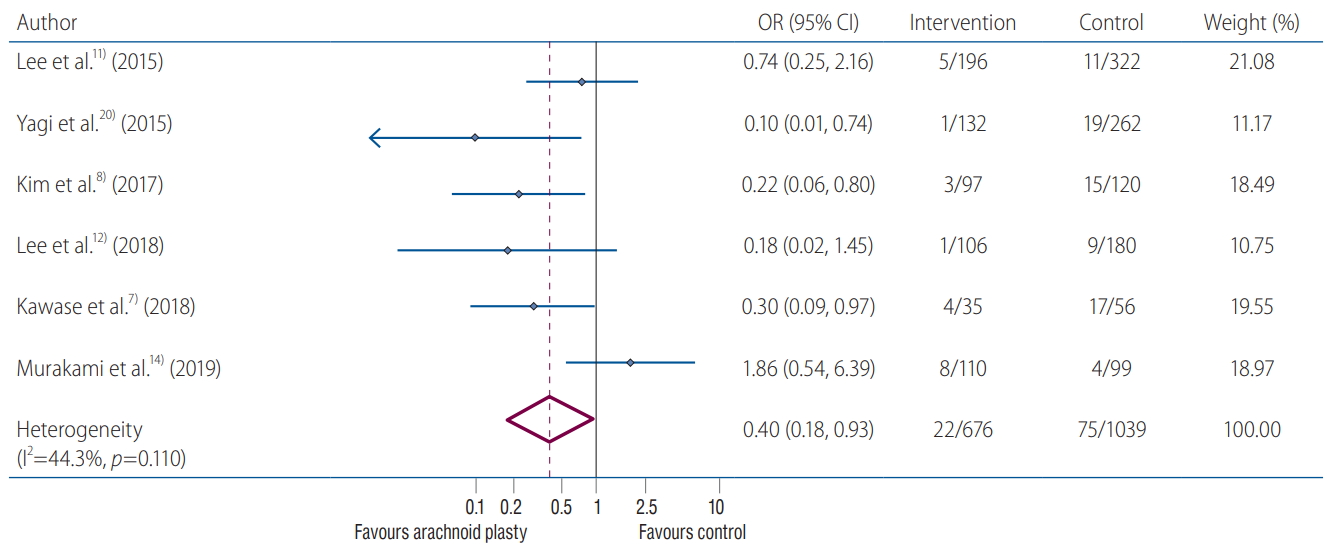
Fig. 3.
Sensitivity analysis for arachnoid plasty efficacy, excluding the Kawase trial. OR : odds ratio, CI : confidence interval. 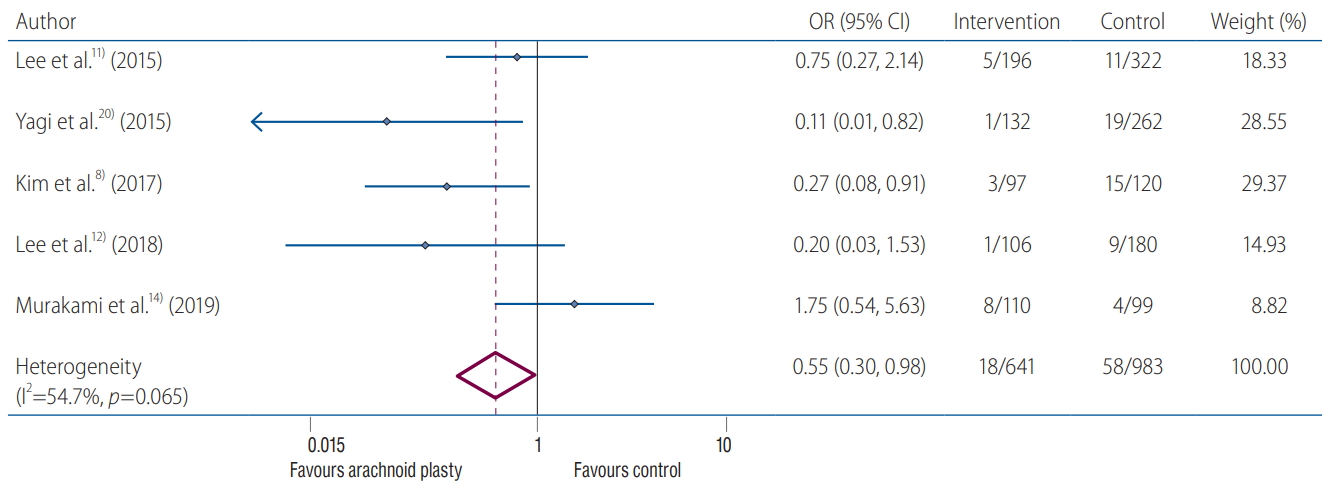
Fig. 4.
Meta-regression analysis for male sex on postoperative chronic subdural hematoma development. 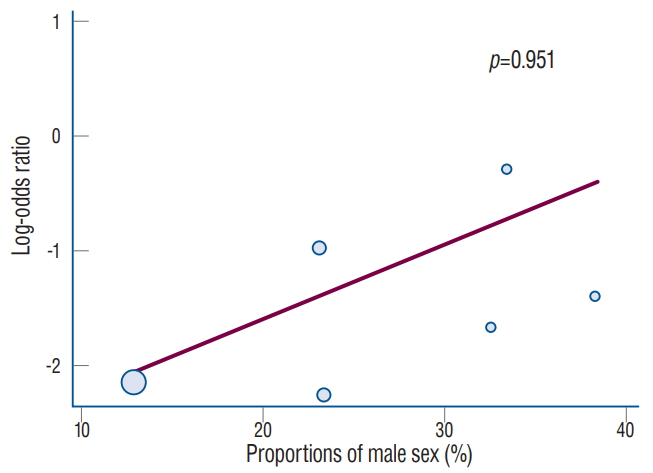
Table 1.
Baseline characteristics of included studies
|
Study |
Design |
Setting |
Aneurysm |
Number of patients
|
Age* (years) |
Male |
Surgical approach |
ARP technique |
|
Total |
ARP |
Control |
|
Lee et al. [11] (2015) |
RO |
Single |
UIA |
518 |
196 (37.8) |
322 (62.2) |
56.6 |
173 (33.4) |
Pterional : 52.5% |
Oxidized cellulosis (SURGICEL® FIBRILLAR™) + Fibrin glue |
|
Lateral supraorbital : 47.5% |
|
Yagi et al. [20] (2015) |
RO |
Single |
UIA |
394 |
132 (33.5) |
262 (66.5) |
62.9 |
92 (23.4) |
Pterional : 100.0% |
Gelatin sponge + Fibrin glue (Gelfoam® + Beriplast®) |
|
Kim et al. [8] (2017) |
RO |
Single |
UIA |
217 |
97 (44.7) |
120 (55.3) |
NR |
83 (38.3) |
Pterional : 100.0% |
Gelatin sponge + Fibrin glue (Cutanplast® + Tisseel®) |
|
Lee et al. [12] (2018) |
RO |
Single |
UIA |
286 |
106 (37.1) |
180 (62.9) |
NR |
93 (32.5) |
Lateral supraorbital : |
Gelatin sponge (SPONGOSTAN™) + Fibrin glue |
|
Kawase et al. [7] (2018) |
RO |
Single |
UIA |
91 |
35 (38.5) |
56 (61.5) |
67.5 |
21 (23.1) |
Pterional : 100.0% |
NR |
|
Murakami et al. [14] (2019) |
RO |
Single |
UIA |
209 |
110 (52.6) |
99 (47.4) |
NR |
55 (26.3) |
NR |
Oxidized cellulosis (SURGICEL®) + Fibrin glue |
References
1. Desai VR, Scranton RA, Britz GW : Management of recurrent subdural hematomas. Neurosurg Clin N Am 28 : 279-286, 2017   2. Gazzeri R, Galarza M, Neroni M, Alfieri A, Giordano M : Hemostatic matrix sealant in neurosurgery: a clinical and imaging study. Acta Neurochir (Wien) 153 : 148-155, 2011    3. Inamasu J, Watabe T, Ganaha T, Yamada Y, Nakae S, Ohmi T, et al : Clinical characteristics and risk factors of chronic subdural haematoma associated with clipping of unruptured cerebral aneurysms. J Clin Neurosci 20 : 1095-1098, 2013   5. Kang JH, Huh SK, Kim J, Park KY, Chung J : Subdural fluid collection after the clipping of unruptured intracranial aneurysms: its clinical course and significance. World Neurosurg 116 : e266-e272, 2018   6. Kawabata S, Tani S, Imamura H, Adachi H, Sakai N : Postoperative subdural air collection is a risk factor for chronic subdural hematoma after surgical clipping of cerebral aneurysms. Neurol Med Chir (Tokyo) 58 : 247-253, 2018    7. Kawase T, Bishnoi I, Tanaka R, Dash C, Kato Y, Yamada Y : Study of incidence and factors: risk and preventive, of chronic subdural hematoma/hygroma in clipped patients of unruptured intracranial aneurysms - an institutional experience. Asian J Neurosurg 13 : 707-713, 2018    8. Kim JH, Kim CH, Lee CY : Efficacy of arachnoid-plasty on chronic subdural hematoma following surgical clipping of unruptured intracranial aneurysms. World neurosurgery 104 : 303-310, 2017   10. Lee KS : The pathogenesis and clinical significance of traumatic subdural hygroma. Brain Inj 12 : 595-603, 1998   13. Mino Y, Hirashima Y, Hamada H, Masuoka T, Yamatani K, Takeda S, et al : Effect of arachnoid plasty using fibrin glue membrane after clipping of ruptured aneurysm on the occurrence of complications and outcome in the elderly patients. Acta neurochirurgica (Wien) 148 : 627-631; discussion 631, 2006   14. Murakami T, Nakagawa I, Park HS, Kotsugi M, Takamura Y, Takeshima Y, et al : Extensive postoperative subdural fluid volume affects the onset of chronic subdural hematoma after unruptured aneurysmal clipping surgery. Clin Neurol Neurosurg 187 : 105533, 2019   15. Ohno T, Iihara K, Takahashi JC, Nakajima N, Satow T, Hishikawa T, et al : Incidence and risk factors of chronic subdural hematoma after aneurysmal clipping. World Neurosurg 80 : 534-537, 2013   16. Park J, Cho JH, Goh DH, Kang DH, Shin IH, Hamm IS : Postoperative subdural hygroma and chronic subdural hematoma after unruptured aneurysm surgery: age, sex, and aneurysm location as independent risk factors. J Neurosurg 124 : 310-317, 2016   18. Sundstrøm T, Helland CA, Aarhus M, Wester K : What is the pressure in chronic subdural hematomas? A prospective, population-based study. J Neurotrauma 29 : 137-142, 2012   19. Tsuruno T : An arachnoid plasty technique using a collagen seat and fibrin glue. Jpn J Neurosurg (Tokyo) 4 : 193-195, 1995  20. Yagi K, Irie S, Inagaki T, Ishii Y, Saito O, Lee T, et al : Intraoperative arachnoid plasty has possibility to prevent chronic subdural hematoma after surgery for unruptured cerebral aneurysms. Neurol Med Chir (Tokyo) 55 : 493-497, 2015    21. Yamamoto H, Hirashima Y, Hamada H, Hayashi N, Origasa H, Endo S : Independent predictors of recurrence of chronic subdural hematoma: results of multivariate analysis performed using a logistic regression model. J Neurosurg 98 : 1217-1221, 2003   22. Yoshimoto Y, Wakai S, Hamano M : External hydrocephalus after aneurysm surgery: paradoxical response to ventricular shunting. J Neurosurg 88 : 485-489, 1998  
|
|