Oh and Hwang: Supraorbital Endoscopic Evacuation for Traumatic Intracerebral Hematomas in the Frontal Lobe
Abstract
Objective
Traumatic intracranial hematomas have been rarely evacuated by endoscopic surgery. The frontal lobe is the usual location for the traumatic intracerebral hematoma (TICH). Endoscopic evacuation for the frontal TICHs via an eyebrow incision is to be presented as minimally invasive surgery.
Methods
Thirteen patients with frontal TICHs were managed with endoscopic hematoma evacuation via eyebrow incision. After making the incision in the lateral eyebrow, a small frontal craniotomy was made, and the hematoma was evacuated under direct visualization of a rigid endoscope. No catheter was placed. Orbital rim resection, hematoma evacuation rate, surgical complications, and outcome at discharge were analyzed.
Results
Men were 11 and the mean age was 54 years old (range, 27-86). Orbitotomy was performed in four patients, and no effect on the hematoma evacuation rate was observed. More than 80% of the hematoma volume was successfully removed in 10 cases. Hematoma configuration was not related to the hematoma evacuation rate. None of the patients underwent revision operation or decompressive craniectomy.
Conclusion
Endoscopic evacuation of the TICHs with the supraorbital approach may be a good method to evacuate the hematoma located in the frontal base.
Key Words: Craniotomy · Endoscopy · Frontal lobe · Traumatic cerebral hemorrhage.
INTRODUCTION
Traumatic intracerebral hematoma (TICH) commonly occurs in the frontal lobe after severe head injury [ 8, 11]. Generally, the traumatic lesions occur in the frontal lobe due to bony ridges on the orbital roof and incidences of indirect injury to the contrecoup [ 3]. The decision to operate a patient with TICH should be made based on considering the radiological findings, the neurological status, and the neurological deterioration in the patient. Large craniectomy with/without hematoma evacuation, craniotomy with hematoma evacuation, or burr hole aspiration should be applied. A conventional frontotemporal scalp incision and craniotomy have been applied for the unilateral frontal TICHs [ 8]. The supraorbital approach was introduced as a way to approach various skull base structures [ 13, 18, 21]. Small frontal craniotomy is performed with or without orbitotomy, followed by operation with microscopic and endoscopic systems, and the surgical incision is made over the eyebrow. The cosmetic benefits and shortening of the operation time have been reported to be superior to conventional craniotomy [ 5, 10]. The supraorbital approach has usually been studied for the vascular and tumorous pathologies in the skull base. The surgical strategy for the management of TICHs using the supraorbital approach has not been discussed. And also endoscopic surgery has been known for providing a panoramic view and reach the remote area through a smaller surgical corridor compared to microscopic surgery. So, we propose a supraorbital approach for the endoscopic evacuation of the frontal TICHs and describe our experiences.
MATERIALs AND METHODS
This study protocol was approved by Instituional Review Board (IRB No. SCHBC 2020-02-017). The patients who underwent surgery for the TICH by a senior author (SCH) were retrieved from the trauma registry in our institution from January 2007 to March 2018. Furthermore, the surgical approach was reviewed, and the cases of endoscopic evacuation for the traumatic frontal ICH via an eyebrow incision were selected. Thirteen patients were enrolled in this study. All the patients and/or relatives signed informed consent for the available treatment and surgical techniques before the operation.
The surgical candidate for the traumatic frontal ICHs was 1) mass effect with midline shifting of >5 mm; 2) growing hematoma in the serial brain computed tomography (CT); and 3) deteriorating consciousness in our institute. The medical records of the patients who underwent endoscopic evacuation for the traumatic frontal ICH via an eyebrow incision were retrospectively reviewed. Hematoma volume was estimated on CT scans using the following equation : volume (mL) = (length × width × thickness) / 2. Hematoma evacuation rate (%) was defined as : (preoperative volume - postoperative volume) / preoperative volume × 100. Hematoma configuration is defined as localized or contused. The localized hematoma signifies homogeneity in the CT density and the contused hematoma is defined as the one with mixed density with hematoma and brain. Rebleeding and surgical complications were analyzed. Operation time, changes in hemoglobin level before and after surgery, and Glasgow outcome scale (GOS) at 3 months after surgery were measured.
Surgical techniques
The supraorbital approach via an eyebrow incision is one of the well-known techniques in the field of minimally invasive neurosurgery and has been well described [ 13, 21]. In the present study, we briefly describe our method. After making an incision in the eyebrow without injuring the supraorbital nerve, frontal skull, and superior orbital rim get exposed to the maximum extent possible. Frontal craniotomy was accomplished with one burr hole on the keyhole. In some cases, the orbital rim was resected en bloc after the periorbita was dissected. After opening the dura, a cortical incision was made on the frontal cortex. After protecting the cortex with a patty, a rigid endoscope (4 mm diameter, 18 cm working length; Karl Storz, Tuttlingen, Germany) was introduced into the hematoma cavity. The endoscope was held and steered in the surgeon’s lefthand during hematoma removal. On observing closely hematoma wall along the cerebral interface, hematoma was taking out as much as possible. No special irrigation system or clot removing device was not used. Although the active bleeding was rarely met, hemostasis could be sufficiently achieved by bipolar cauterization. And the hematoma adjacent the pia mater on the frontal base was intentionally left to avoiding the further bleeding. After complete hemostasis, dura mater and bone flap were closed in a usual manner.
Statistical analysis
The IBM SPSS version 18.0 software (SPSS Inc., Chicago, IL, USA) was used for data analysis. The chi-square test was used and a p-value <0.05 was considered statistically significant.
RESULTS
Thirteen traumatic frontal ICHs were operated via an eyebrow incision. The demographic and clinical characteristics of 13 patients (11 men and two women) are presented in Table 1. The mean age of the patients was 54 years old (range, 27-86). Most of the accidents were slip-down and falling. For the craniotomy, orbitotomy was performed in four cases. The orbitotomy was performed only in the early days of surgery and the procedure took a longer operation time. The mean volume of the preoperative frontal ICHs was 50.4 mL (range, 20-136). More than 80% of the hematoma volume was successfully removed in 10 cases. Orbitotomy and hematoma configuration exhibited no influence of the hematoma evacuation rate ( Table 2). No catheter for ICHs drainage was not indwelled. The operation lasted for about 1.5 hours. There was no incidence of rebleeding or revision surgery. Transfusion was not required after the operation, and the postoperative hemoglobin drop was usually within 1 g/dL. A woman aged 86 years died of pneumonia on the postoperative 18th day, and most of the patients exhibited good recovery as per the GOS.
Case 1
A 46-year-old man came to the emergency room with semicomatose consciousness. He fell down while driving a motorcycle and experienced severe headaches immediately after the trauma at 6 p.m. He went to sleep and won’t wake up after drove the motorcycle at 11 p.m. In the emergency room, his consciousness was semicomatose with abnormal flexion on the painful stimuli and his right pupil was dilated without direct and indirect light reflex. The left pupil was reactive to light. Brain CT revealed a large amount of epidural hematoma (EDH) on the right temporoparietal area with a linear skull fracture. Also, ICH was identified on the left frontal lobe ( Fig. 1A). Both the lateral ventricles were compressed and a midline shift of about 12 mm was noted towards the right side. Subsequently, the acute EDH was removed by emergency craniotomy and the middle meningeal artery beneath the skull fracture was torn and coagulated. After the evacuation of EDH, improvement in the midline shift was observed. But, the ventricular compression was still noted ( Fig. 1B). The preoperative hemoglobin was 12 mg/dL and it dropped to 7 mg/dL after surgery. The patients’ right pupil became reactive to the light. It was planned to remove the left frontal ICH by minimizing the blood loss because of the low hemoglobin level. Under general anesthesia, a linear incision was made on the left eyebrow. Small supraorbital craniotomy without an orbitotomy was created ( Fig. 1D) and a rigid endoscope was introduced into the hematoma cavity. The ICH was just removed with gentle suction under direct endoscopic visualization. There was no definite offending bleeder. Dura was closed and bone flap was fixed with a CranioFix (Aesculap AG, Tuttlingen, Germany). The ICH was near-totally evacuated and the mass effect was much resolved ( Fig. 1C). The patient recovered consciousness and was completely alert at the time of discharge.
Case 2
A 74-year-old man was found in an unconscious mental state in the hallway of his apartment. He suffered from laryngeal cancer and hepatocellular carcinoma. He had a tracheostomy after laryngeal surgery. He was stuporous with reactive pupils. Huge ICH in the right lobe was found in the brain CT with compression of the lateral ventricle ( Fig. 2A). Platelet count in the blood was decreased to 83000/mcL and prothrombin time was normal as 12.5 seconds. He was planned for emergency hematoma evacuation. Under general anesthesia, a linear incision was made on the right eyebrow. A supraorbital craniotomy was made in a usual manner and dura was found to be moderately tense. After dural opening, a small cortical incision was made under rigid endoscopic visualization ( Fig. 2C). While removing the hematoma, we closely observed the hematoma-brain border to save the brain and remove the hematoma to the maximum extent possible. After confirming the hemostasis ( Fig. 2D), dura was closed in a water-tight manner, and bone flap was fixed with a miniplate. The frontal hematoma was nearly evacuated and the ventricle compression was relieved ( Fig. 2B). The patient recovered and turned to his normal activities at the time of discharge.
DISCUSSION
Brain trauma surgery focuses on the control of increased intracranial pressure (ICP). Traumatic intracranial hematoma does not generally occur as a single lesion. Also, the choice of operative technique is influenced by the surgeon’s expertise, training, and evaluation of a particular situation [ 14, 15]. But, for TICHs, early surgery within 12 hours may be a valuable tool in the treatment of TICH compared with initial conservative treatment with delayed evacuation [ 9]. Patients with TICHs could get benefits by removing the hematoma without a large craniectomy under certain circumstances. Our results suggest that evacuation of acute frontal TICHs can be achieved via a small supraorbital craniotomy in a less invasive manner by using the endoscope. TICHs in the parietal lobe or temporal lobe have relatively obvious neurological symptoms, whereas the initial neurological status in frontal lobe shows 13% to 17% of abnormal pupillary reaction and hemiplegia, which is more silent than other lesions [ 11]. The surgical guidelines in 2006 recommended that for the frontal TICHs was that in the patient with Glasgow comas scale of 6 to 8 with frontal or temporal contusions ≥20 cm 3 in volume with midline shift of at least 5 mm and/or cisternal compression on CT scan or patients with any lesion ≥50 cm 3 in volume, neurosurgical interventions are warranted [ 4]. The hematoma volume was more than 20 cm 3 in all our cases. After surgery, a craniectomy was not required. The hematoma was removed to the extent that the patient did not deteriorate neurologically in the postoperative course. More than 20 cm 3 of TICH, located in the frontal base, would be a good candidate for the supraorbital approach and endoscopic evacuation of the hematoma. If increased ICP is the main concern after hematoma evacuation, a decompressive craniectomy is mandatory. The neurosurgeon should be confident about the fact that sufficient removal of the hematoma will provide enough control of ICP after completion of surgery. Surgical evacuation of a hematoma can be accomplished by craniotomy/craniectomy or stereotactic-guided aspiration via the burr-hole craniotomy [ 1, 4]. Decompressive craniectomy in traumatic brain injury (TBI) can effectively reduce ICP and secondary brain damage and lower the risk of brain herniation caused by extensive cerebral edema. Decompressive craniectomy is not considered as essential in cases where control of ICP can be achieved simply after the hematoma evacuation. In this situation, minimally invasive surgery is regarded as a good alternative to large craniotomy. Endoscopic surgery has been reported as a safe and effective way to manage the deep-seated hypertensive ICH [ 12, 17]. But, reports on the endoscopic surgery for the TICHs are limited. Surgeries for a brain tumor and aneurysms via supraorbital craniotomy have been performed under both microscope and endoscope [ 13, 18, 21]. The cosmetic result with an eyebrow incision is excellent after the surgery. This surgery has become a popular approach under certain circumstances and based on the preference of the surgeon. The pathologies located parallel to or below the orbital roof could be handled under both microscope and endoscope through the surgical window between the orbital roof and the frontal lobe. However, microscopic surgery does not reach the pathology inside the frontal lobe because of straight light projection and a narrow surgical corridor in the small supraorbital craniotomy. The rigid endoscope can be placed directly in the frontal hematoma and the panoramic view enables the surgeon to have a wide surgical view for evacuating the hematoma. Even though we resected orbital rim in four cases during the early surgeries, it was not necessary as the endoscope was steerable and provided a wide surgical view. Based on our small experiences, it is hypothesized that additional orbitotomy is not essential during eyebrow incision and endoscopic evacuation of frontal TICHs. A minimally invasive cranial surgery may be considered in patients who cannot tolerate a larger craniotomy because of blood loss or other comorbidities. Intraoperative hypotension and patient comorbidity are significant independent predictors of increased mortality [ 16]. Furthermore, older age is a significant predictor of surgical mortality [ 20]. Less time-consuming and blood-losing surgical approaches help to reduce mortality in comorbid elderly patients. In most of our cases, hemoglobin loss was postoperatively less than 1 g/dL. Supraorbital craniotomy and endoscopic hematoma evacuation for the frontal TICHs are proposed as good surgical strategies, especially in elderly patients with deteriorating neurological conditions. The functions of the frontal lobes are divisible into four distinct anatomically discrete categories : executive functions, speed of processing, personality changes, and problems with empathy and social cognition. TBI predominantly causes damage to the frontal/temporal regions, regardless of the pathophysiology [ 19]. Even though the clinical presentation after TBI is heterogenous, damage to the frontal lobe leads to cognitive, emotional, and social-behavioral sequelae that negatively affect the quality of life. In the field of animal research, unilateral frontal lobe contusion in mice has been reported to produce long-term impairments to social recognition and reversal learning [ 6]. No comprehensive published research indicates whether evacuation of TICHs and decompressive craniectomy are better for the functional outcomes [ 7]. Cerebral contusion and necrotic core are the primal source of contusion edema. And neuro-endoscopic aspiration of the necrotic core promptly ameliorates brain edema [ 15]. The accomplishment of appropriate removal of TICH and cerebral contusion might be helpful to obtain better outcomes by preventing further progression of brain edema. Further research is necessary to elucidate it in the future. Moreover, it is important to recognize the heterogeneity of TBI and that the “one-size-fits-all approach” may not always be appropriate for all the TBI patients [ 2]. This study has some limitations. The cases of the study were small and retrospectively analyzed. Furthermore, a comparison of different surgical approaches for the frontal TICHs was not the major aim of the study. So, the surgical indication and techniques could not be applied for most of the TICHs in the frontal lobe. We believe that surgical candidates will be limited in the frontal TICHs located mainly at the base of the frontal lobe. Also, we intended to provide the feasibility of the supraorbital approach for the frontal TICHs, and not to analyze the functional outcomes. It could not be argued that surgical evacuation for the frontal TICHs has a better prognosis.
CONCLUSION
Endoscopic evacuation of the TICHs with the supraorbital approach may be a good alternative surgical method to evacuate the hematoma located in the frontal base, especially in the elderly. It could be sufficiently achieved without orbitotomy and with minimal blood loss.
Acknowledgements
This work was supported by the Soonchunhyang University Research Fund and the National Research Foundation of Korea (NRF) grant funded by the Korean government (Ministry of Science and ICT) (grant number : NRF-2019R1G1A1109991313).
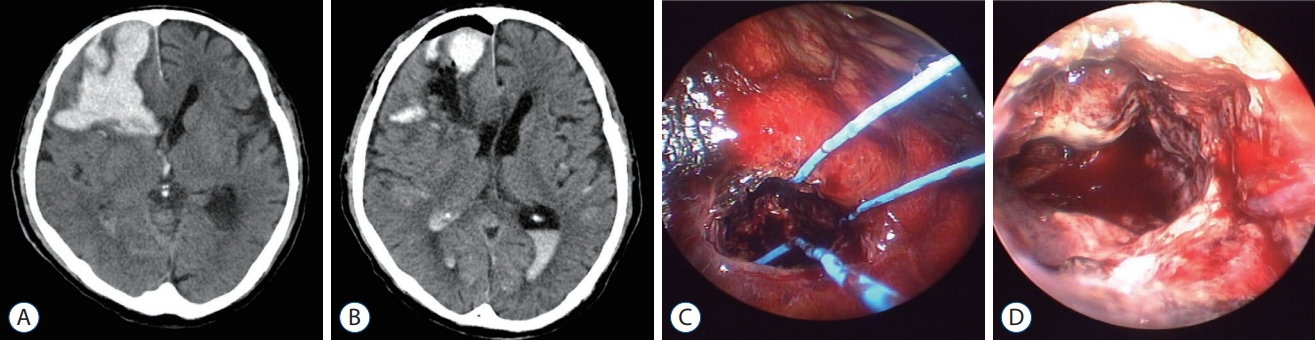
Fig. 1.
Illustrations of case 1. A : Computed tomography (CT) scan of a semicomatose conscious 46-year-old man taken immediately after the motorcycle accident. A large amount of epidural hematoma (EDH) in the right parietal and intracerebral hematoma (ICH) in the left frontal lobe can be seen. B : Postoperative CT scan after craniotomy and evacuation of EDH on the right parietal. Frontal ICH slightly grows and compresses the lateral ventricle. Supraorbital endoscopic evacuation of frontal ICH was attempted and ICH was sufficiently removed (C). Small craniotomy on the left supraorbital skull (arrow) was visualized (D). 
Fig. 2.
Illustrations of case 2. A 74-year-old man was found with semicomatose consciousness. Huge intracerebral hematoma (ICH) in the right frontal lobe can be seen (A). After endoscopic evacuation for ICH, nearly total removal was achieved (B). Endoscopic views of the cortical incision (C) and final stage with hemostasis (D). 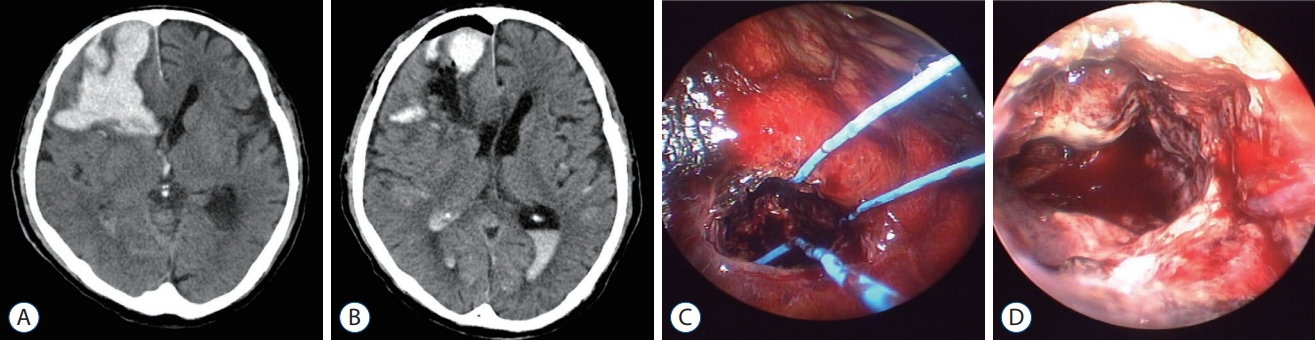
Table 1.
Characteristics of 13 patients of endoscopic evacuation for the traumatic frontal hematomas
|
Characteristic |
Value |
|
Men : women |
11 : 2 |
|
Age (years) |
54 (27-86) |
|
Trauma mechanisms |
|
|
Slip down |
5 |
|
Falling |
2 |
|
Traffic accident |
2 |
|
Direct impact |
1 |
|
Unknown |
3 |
|
Orbitotomy |
|
|
Yes |
4 |
|
No |
9 |
|
Hematoma configuration |
|
|
Localized |
7 |
|
Contused |
6 |
|
Hematoma volume (mL) |
|
|
Preoperative |
50.4 (20-126) |
|
Postoperative |
8.7 (2-31) |
|
Revision surgery |
None |
|
Hemoglobin changes |
|
|
≤1 |
11 |
|
>1 |
2 |
Table 2.
Hematoma evacuation rate according to the orbitotomy and the hematoma configuration
|
Hematoma evacuation rate
|
p-value |
|
≥80% |
<80% |
|
Orbitotomy |
|
|
0.91 |
|
Yes |
3 |
1 |
|
|
No |
7 |
2 |
|
|
Hematoma configuration |
|
|
0.61 |
|
Localized |
5 |
2 |
|
|
Contused |
5 |
1 |
|
References
1. Abdu E, Hanley DF, Newell DW : Minimally invasive treatment for intracerebral hemorrhage. Neurosurg Focus 32 : E3, 2012   2. Adams H, Kolias AG, Hutchinson PJ : The role of surgical intervention in traumatic brain injury. Neurosurg Clin N Am 27 : 519-528, 2016   3. Al-Sarraj S : The pathology of traumatic brain injury (TBI): a practical approach. Diagn Histopathol 22 : 318-326, 2016  4. Bullock MR, Chesnut R, Ghajar J, Gordon D, Hartl R, Newell DW, et al : Surgical management of traumatic parenchymal lesions. Neurosurgery 58 : S25-S46, 2006    5. Chalouhi N, Jabbour P, Ibrahim I, Starke RM, Younes P, El Hage G, et al : Surgical treatment of ruptured anterior circulation aneurysms: comparison of pterional and supraorbital keyhole approaches. Neurosurgery 72 : 437-441, 2013  6. Chou A, Morganti JM, Rosi S : Frontal lobe contusion in mice chronically impairs prefrontal-dependent behavior. PLoS One 11 : e01514182016    7. Cooper DJ, Rosenfeld JV, Murray L, Arabi YM, Davies AR, Ponsford J, et al : Patient outcomes at twelve months after early decompressive craniectomy for diffuse traumatic brain injury in the randomized DECRA clinical trial. J Neurotrauma 37 : 810-816, 2020   8. Gao L, Wu X, Hu J, Jin Y, Han X, Wu X, et al : Intensive management and prognosis of 127 cases with traumatic bilateral frontal contusions. World Neurosurg 80 : 879-888, 2013   10. Hernesniemi J, Ishii K, Niemelä M, Smrcka M, Kivipelto L, Fujiki M, et al : Lateral supraorbital approach as an alternative to the classical pterional approach. Acta Neurochir Suppl 94 : 17-21, 2005   11. Hung KS, Liang CL, Wang CH, Chang HW, Park N, Juo SH : Outcome after traumatic frontal intracerebral haemorrhage: a comparison of unilateral and bilateral haematomas. J Clin Neurosci 11 : 849-853, 2004   12. Hwang SC, Yeo DG, Shin DS, Kim BT : Soft membrane sheath for endoscopic surgery of intracerebral hematomas. World Neurosurg 90 : 268-272, 2016   13. Jane JA, Park TS, Pobereskin LH, Winn HR, Butler AB : The supraorbital approach: technical note. Neurosurgery 11 : 537-542, 1982    15. Mino M, Fujimura M, Yoshida M, Sonobe S, Tominaga T : Application of neuro-endoscopic target aspiration of the necrotic core for cerebral contusion with delayed progression: technical note. Acta Neurochir (Wien) 161 : 225-230, 2019    16. Monk TG, Saini V, Weldon BC, Sigl JC : Anesthetic management and one-year mortality after noncardiac surgery. Anesth Analg 100 : 4-10, 2005   17. Nagasaka T, Tsugeno M, Ikeda H, Okamoto T, Inao S, Wakabayashi T : A novel monoshaft bipolar cautery for use in endoscopic intracranial surgery. A short technical note. Clin Neurol Neurosurg 113 : 607-611, 2011   18. Reisch R, Perneczky A : Ten-year experience with the supraorbital subfrontal approach through an eyebrow skin incision. Neurosurgery 57 : 242-255, 2005    19. Stuss DT : Traumatic brain injury: relation to executive dysfunction and the frontal lobes. Curr Opin Neurol 24 : 584-589, 2011  20. Turrentine FE, Wang H, Simpson VB, Jones RS : Surgical risk factors, morbidity, and mortality in elderly patients. J Am Coll Surg 203 : 865-877, 2006   21. Wilson DA, Duong H, Teo C, Kelly DF : The supraorbital endoscopic approach for tumors. World Neurosurg 82 : e243-e256, 2014  
|
|