Neurotization from Two Medial Pectoral Nerves to Musculocutaneous Nerve in a Pediatric Brachial Plexus Injury
Article information
Abstract
Traumatic brachial plexus injuries can be devastating, causing partial to total denervation of the muscles of the upper extremities. Surgical reconstruction can restore motor and/or sensory function following nerve injuries. Direct nerve-to-nerve transfers can provide a closer nerve source to the target muscle, thereby enhancing the quality and rate of recovery. Restoration of elbow flexion is the primary goal for patients with brachial plexus injuries. A 4-year-old right-hand-dominant male sustained a fracture of the left scapula in a car accident. He was treated conservatively. After the accident, he presented with motor weakness of the left upper extremity. Shoulder abduction was grade 3 and elbow flexor was grade 0. Hand function was intact. Nerve conduction studies and an electromyogram were performed, which revealed left lateral and posterior cord brachial plexopathy with axonotmesis. He was admitted to Rehabilitation Medicine and treated. However, marked neurological dysfunction in the left upper extremity was still observed. Six months after trauma, under general anesthesia with the patient in the supine position, the brachial plexus was explored through infraclavicular and supraclavicular incisions. Each terminal branch was confirmed by electrophysiology. Avulsion of the C5 roots and absence of usable stump proximally were confirmed intraoperatively. Under a microscope, neurotization from the musculocutaneous nerve to two medial pectoral nerves was performed with nylon 8-0. Physical treatment and electrostimulation started 2 weeks postoperatively. At a 3-month postoperative visit, evidence of reinnervation of the elbow flexors was observed. At his last follow-up, 2 years following trauma, the patient had recovered Medical Research Council (MRC) grade 4+ elbow flexors. We propose that neurotization from medial pectoral nerves to musculocutaneous nerve can be used successfully to restore elbow flexion in patients with brachial plexus injuries.
INTRODUCTION
Neurotization involves the repair of a distal denervated nerve element using a proximal foreign nerve as the neuron and axon donor to reinnervate the distal target4). Direct nerve-to-nerve transfers can provide a closer nerve source to the target muscle, thereby enhancing the quality and rate of recovery7). Traumatic brachial plexus palsy is usually caused by traction across long segments of the trunks, divisions, or cords and may be segmental in nature8). Brachial plexus palsy remains one of the most challenging traumatic peripheral nerves injuries to treat. Treatment options including neurolysis, nerve grafting, or neurotization have become important in restoring function in patients with irreparable preganglionic lesions5). Tuttle12) published the first report on neurotization in an attempt to restore injured plexus function and Narakas6) published a review of the historical precedents and the anatomical basis and rationale for nerve transfers in brachial plexus surgery. A variety of donor nerves can be used as sources for neurotization. Some of the more common neurotization sources include the spinal accessory nerve, the phrenic nerve, the medial pectoral nerves, and intercostal nerves. In a C5-C6 injury, Brandt and Mackinnon1) used a closer nerve source to restore musculocutaneous function. Branches of the medial pectoral nerves were transferred directly to the musculocutaneous nerve, promoting good recovery of function7). We describe a 4-year-old patient with a brachial plexus injury who received neurotization from two medial pectoral nerves to the musculocutaneous nerve.
CASE REPORT
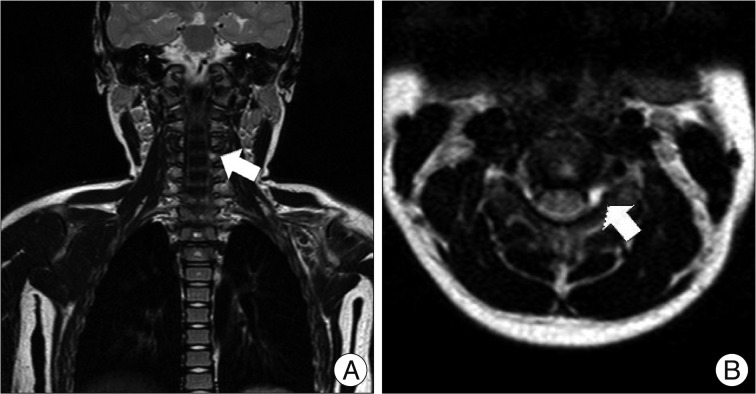
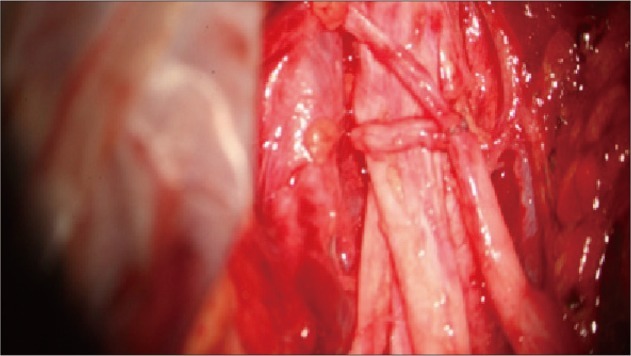
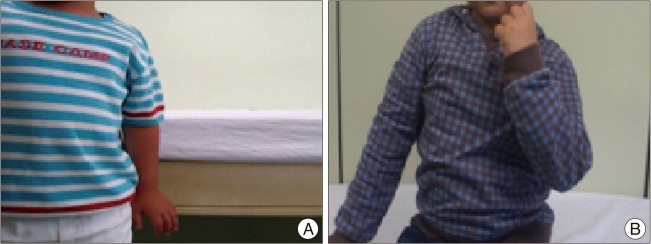
A 4-year-old right-hand-dominant boy sustained a fracture of the left scapula in a car accident. He was treated conservatively. After the accident, he presented with motor weakness of his left upper extremity. Shoulder abduction was grade 3 and elbow flexor was grade 0. Motor assessment was based on the motor classification M0-M5 in the Mallet and Medical Research Council (MRC) Muscle Grading System. Hand function was intact. The patient underwent magnetic resonance imaging (MRI), which revealed a lateral pseudomeningocele arising from the left C4-5 intervertebral foramen (Fig. 1). Nerve conduction studies and an electromyogram (EMG) were performed. Left musculocutaneous nerve and axillary nerve motor conduction studies revealed low compound motor action potential (CMAP) amplitudes. On a needle EMG, positive sharp waves and fibrillation potentials were noted in the left deltoid, biceps brachii, and brachioradialis muscles. Maximal contraction reduced interference patterns were observed in the same muscles. These findings suggested left lateral and posterior cord brachial plexopathy with axonotmesis. The patient was admitted to Rehabilitation Medicine and treated. However, marked neurological dysfunction in the left upper extremity was still noted. Six months after trauma, under general anesthesia with the patient in the supine position, the brachial plexus was explored through infraclavicular and supraclavicular incisions. For supraclavicular exposure the incision extended from the level of the angle of the mandible and followed the posterior border of the sternocleidomastoid muscle to the clavicle. Skin and platysma were retracted, and the sternocleidomastoid muscle exposed. The spinal accessory nerve crosses the sternocleidomastoid muscle and was preserved. The brachial plexus was observed between the scalenus anterior and scalenus medius muscle, and the phrenic nerve was found on the anterior surface of the scalenus anterior muscle. Dissection proceeded medially by cutting both scalenus muscles to fully expose the plexus and the roots. Avulsion of the C5 roots and absence of usable stump proximally were confirmed intraoperatively. The incision for the infraclavicular exposure began at the distal third of the clavicle and moved inferiorly into the deltopectoral groove. Dissection proceeded along the groove between deltoid muscle and pectoralis major muscle from clavicle to axilla. Retractors were placed between the two muscles and the medial pectoral nerves were visualized. The pectoralis major and minor muscles were cut. The biceps fascia was opened and the musculocutaneous nerve identified. Each terminal branch was confirmed by electrophysiology. Under a microscope, neurotization from the musculocutaneous nerve to two medial pectoral nerves was performed with nylon 8-0 (Fig. 2). For 2 weeks, the shoulder was immobilized in adduction and internal rotation and the elbow in flexion. Physical therapy and electrostimulation started 2 weeks postoperatively. At a 3-month postoperative visit, evidence of reinnervation of the elbow flexors was observed. At his last follow-up, 2 years after trauma, the patient had recovered MRC grade 4+ elbow flexion (Fig. 3). A postoperative electrophysiological study illustrated his vast improvement.
DISCUSSION
The incidence and severity of brachial plexus injury have been increasing worldwide mainly due to an escalating number of motorcycle accidents. Most of these injuries are high velocity injuries resulting in root avulsions. These injuries are often devastating, and can lead to significant long-term functional disability13). Patients with traction brachial plexus lesions are generally observed for spontaneous recovery for several months. Those who do not demonstrate clinical or electrical recovery by 3 to 6 months after trauma should undergo operative intervention5). Nerve transfer by reinnervating the most functionally important nerves using intact neighboring nerves has become widely accepted since the 1963 study by Sedden10). Muscle reinnervation following nerve injury is essential for the successful recovery of motor function. A critical number of motor axons must regenerate and reinnervate the motor end plate to provide adequate muscle power2).
Surgical management of patients with severe brachial plexus injuries involves first determining preoperatively whether most or all the nerve roots are truly avulsed3). The second goal is to perform nerve repair, which in severe cases (i.e., those with avulsion) involves appropriate nerve transfers to reanimate the extremity11). Intraoperative electrical tests and operative findings are used in concert with the preoperative clinical, electromyography, and imaging findings to determine the extent of the injury and the presence of nerve root avulsion and to guide determination of the most suitable nerve reconstructive procedure4). Our patient experienced left upper extremity motor weakness, especially in elbow flexion. Left brachial plexopathy was confirmed through neurophysiological tests, including (electromyography and nerve conduction velocity tests). In C5 root avulsion injuries, loss of abduction and external rotation at the shoulder and flexion in the elbow are the main functional deficits. The goal in the management of upper (C5-6) nerve root paralysis is complete repair. When the upper roots are avulsed from the spinal cord, the only repair option is neurotization using a nerve transfer4).
The musculocutaneous nerve, one of the terminal branches of the brachial plexus, arises principally from the fifth and sixth cervical nerves. The pectoralis major muscle has dual input from the medial and lateral pectoral nerves, arising from the medial and lateral cords, respectively4). Brandt and Mackinnon1) directed the medial pectorals to the musculocutaneous nerve, with the additional innovation of turning the lateral antebrachial cutaneous nerve (the cutaneous derivative of the musculocutaneous nerve) into the biceps muscle to avoid loss of motor axons in the cutaneous distribution. The results of the different series vary. However, Samardzic9) noted that medial pectoral nerve transfers were associated with significantly improved outcomes in elbow flexion as compared with intercostal and accessory nerve transfers. The proximity of a normal medial pectoral motor nerve to the musculocutaneous recipient provides a theoretical advantage for early recovery; Brandt1) confirmed that biceps reinnervation occurs between 6 and 8 months postoperatively. The present case demonstrated that after total avulsion injury of the brachial plexus, an upper limb could be restored through neurotization from the musculocutaneous nerve to the medial pectoral nerves. One must isolate the function of the biceps and pectoralis major muscle to allow an object to be held within the arm and thorax without concomitant elbow flexion.
Postoperative rehabilitation is an essential final step and usually requires 2 to 3 years. To maximize function following neurotization, the rehabilitation program must include motor re-education to initiate recruitment of the weak reinnervated muscles and establish new motor patterns and cortical mapping. Patient education and a home program are essential for obtaining optimal functioning.
CONCLUSION
Neurotization is an effective treatment option for the restoration of elbow and shoulder function in brachial plexus injuries. Early intervention and postoperative rehabilitation allow for the recovery of shoulder and elbow function in most patients. We have shown that neurotization from the medial pectoral nerves to musculocutaneous nerve can be used successfully to restore elbow flexion in patients with brachial plexus injuries.