Midline-Splitting Open Door Laminoplasty Using Hydroxyapatite Spacers : Comparison between Two Different Shaped Spacers
Article information
Abstract
Objective
Although hydroxyapatite (HA) spacer has been used for laminoplasty, there have been no reports on factors associated with fusion and on the effects of HA shape.
Methods
During January 2004 and January 2010, 45 patients with compressive cervical myelopathy underwent midline-splitting open door laminoplasty with winged (33 cases) and wingless (12 cases) HAs by a single surgeon. Minimal and mean follow up times were 12 and 28.1 months, respectively. Japanese Orthopedic Association (JOA) score was used for clinical outcome measurement. Cervical X-rays were taken preoperatively, immediately post-operatively, and after 3, 6, and 12 months and computed tomography scans were performed preoperatively, immediately post-operatively and after 12 months. Cervical lordosis, canal dimension, fusion between lamina and HA, and affecting factors of fusion were analyzed.
Results
All surgeries were performed on 142 levels, 99 in the winged and 43 in the wingless HA groups. JOA scores of the winged group changed from 10.4±2.94 to 13.3±2.35 and scores of the wingless group changed from 10.8±2.87 to 13.8±3.05. There was no significant difference on lordotic and canal dimensional change between two groups. Post-operative 12 month fusion rate between lamina and HA was significantly lower in the winged group (18.2 vs. 48.8% p=0.001). Multivariate analysis showed that ossification of the posterior longitudinal ligament, male gender, and wingless type HA were significantly associated with fusion.
Conclusion
Clinical outcome was similar in patients receiving winged and wingless HA, but the wingless type was associated with a higher rate of fusion between HA and lamina at 12 months post-operatively.
INTRODUCTION
Midline splitting open-door laminoplasty has been considered an effective and safe method for decompressing multisegmental cervical lesions caused by cervical spondylotic myelopathy (CSM), ossification of the posterior longitudinal ligament (OPLL), or intervertebral disc herniation with developmental canal stenosis, as well as for achieving immediate stability of these lesions1,5,9,11,13,16,18). Since the development of an artificial hydroxyapatite (HA) spacer for laminoplasty, several studies have described its biocompatibility, post-operative contact status with lamina, and fusion rate, as well as post-operative canal narrowing and displacement of HA after laminoplasty2,3,6,10,12,15). To our knowledge, however, factors associated with fusion between lamina and HA and the effects of HA shapes on outcomes have not yet been assessed. We therefore analyzed factors significantly affecting fusion between lamina and HA as well as the effects of HA shape on post-operative clinical and radiological outcomes.
MATERIALS AND METHODS
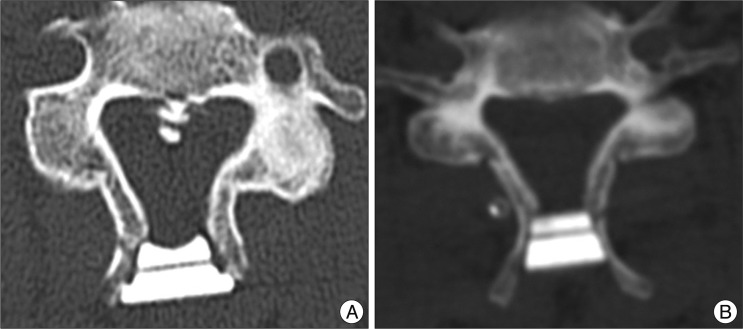
We retrospectively analyzed the outcomes of 45 patients (33 men, 12 women) with myelopathy who underwent midline splitting open door laminoplasty using HA between January 2004 and January 2010. Mean follow up duration was 28.1 months (range, 12-61 months). Of these patients, 23 were diagnosed with CSM and 22 with OPLL. Patients with cervical kyphosis, evidence of cervical instability, serious medical problems, and those who underwent prior anterior cervical surgery were excluded. All laminoplasties were performed by a single surgeon. Gutters were made at the bilateral laminofacet junctions with a 3 mm diameter diamond type burr, and the midline spinous process was split with a 2 mm diameter diamond type burr. We used APACERAM® HA (PENTAX, Tokyo, Japan), with 100-500 µm macropores and 0.5-2.0 µm micropores. A winged or wingless type HA was inserted between the split spinous processes and fixed with black silk (Fig. 1). Patients were classified into two groups based on HA shape; the baseline characteristics of the winged and wingless groups are shown in Table 1. The selection of patients was randomized. Informed consent for all the patients before surgery was done. The primary clinical outcome was change in Japanese Orthopedic Association (JOA) score (0-17). Recovery from myelopathy at 12 months was calculated using the formula : 12 month JOA score-pre operative JOA score)/(17-pre operative JOA score).
Cervical X-rays were taken preoperatively, immediately post-operatively, and after 3, 6, and 12 months and computed tomography (CT) was performed preoperatively, immediately post-operatively, and after 12 months. Change in overall cervical lordosis, dimension of the spinal canal, and anterior-posterior (AP) distance between the posterior surface of the vertebral body and the anterior surface of HA were assessed on axial CT images.
Bonding status between lamina and HA immediately after surgery, and fusion between lamina and HA at 12 months were assayed as described2,4).
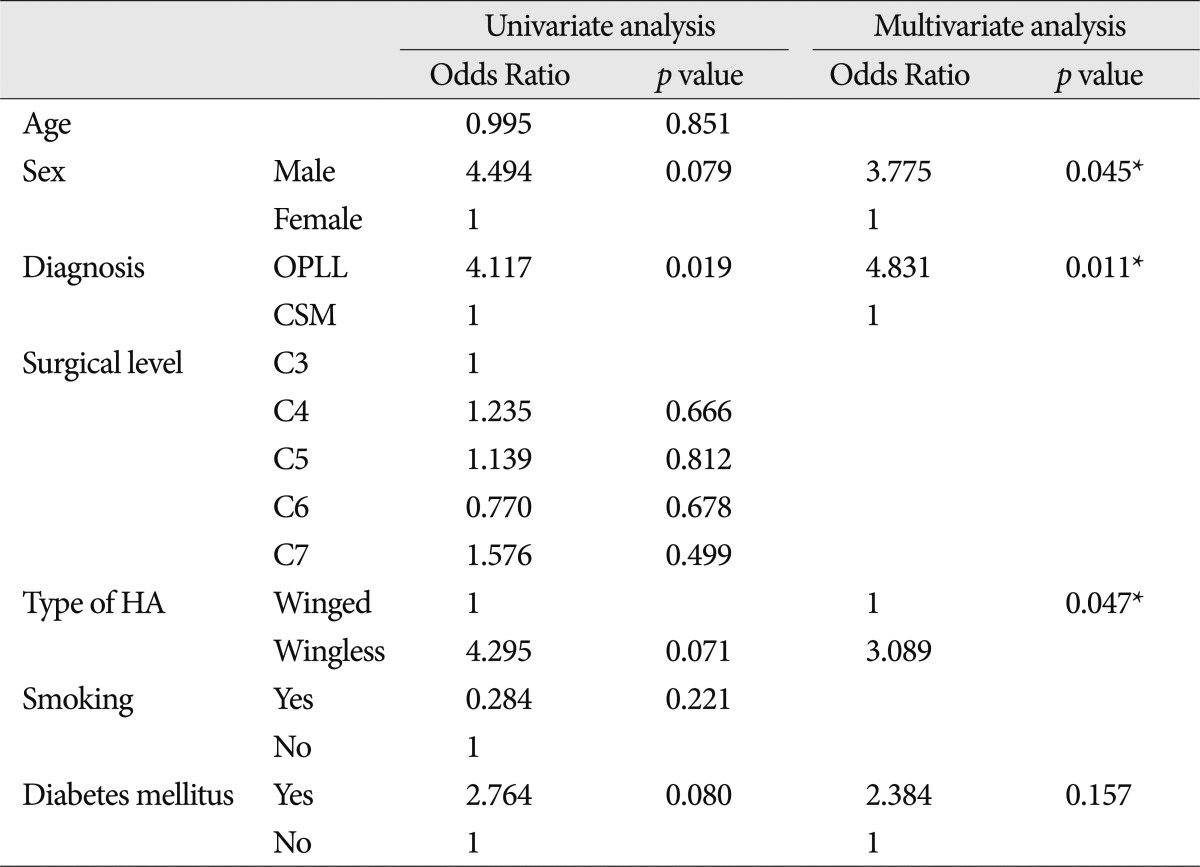
Factors that affected the rate of fusion between laminae and HA (D or E status which were classified as fused status by Iguchi et al.) were analyzed by uni- and multivariate logistic regression4). Age, sex, diagnosis, level of operation, smoking, diabetes mellitus (DM), and type of HA were included in these analyses.
Groups were compared using the Wilcoxon signed rank test, paired t-test, χ2 test, Fisher's exact test, Mann-Whitney test, Linear mixed model, and uni- and multivariate logistic regression. If p value is under 0.05, we defined it statistically significant.
RESULTS
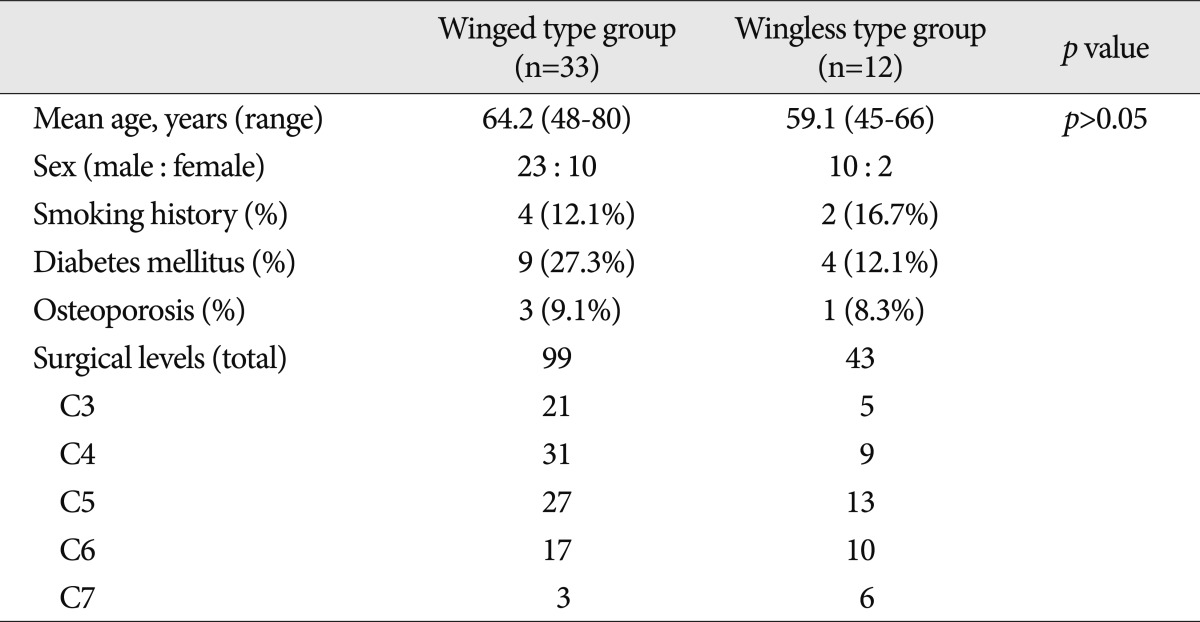
Of the 45 included patients, 33 (23 males, 10 females) received winged type HA and 12 (10 males, 2 females) received the wingless type. Surgeries were performed on 142 levels, 99 in the winged type and 43 in the wingless type group. There was no significant difference between those two groups in baseline characteristics (Table 1).
Mean JOA scores changed from 10.4±2.94 to 13.3±2.35 in the winged type group and from 10.8±2.87 to 13.8±3.05 in the wingless type group, with mean calculated recovery rates of 48±35.5% and 53±45.2%, respectively (p=0.706) (Table 2).
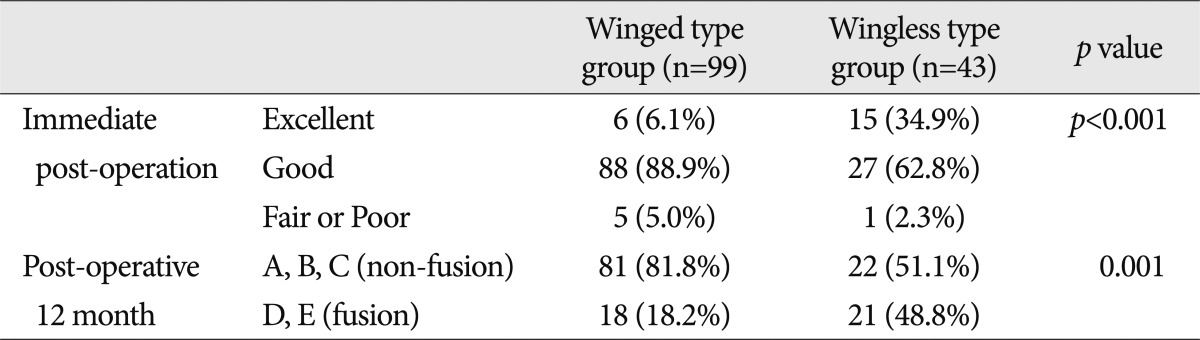
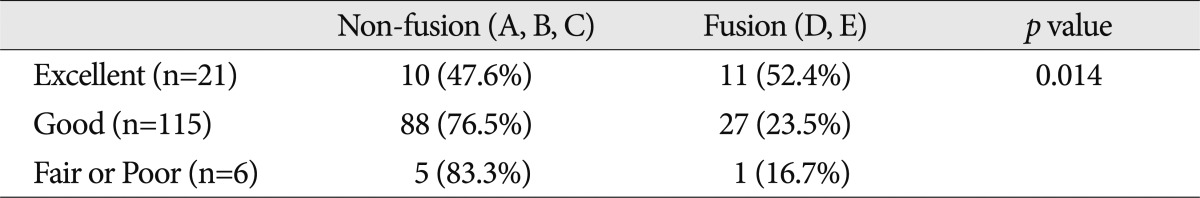
Immediate post-operative bonding status of the winged and wingless groups were excellent at 6 and 15 levels, respectively; good at 88 and 27 levels, respectively; fair at 4 and 1 levels, respectively; and poor at 1 and 0 levels, respectively (p<0.001) (Table 3).
The overall post-operative 12 month fusion rate between lamina and HA, classified as D or E status was 27.46%, 18.2% in the winged and 48.8% in the wingless group (p=0.001) (Table 3).
Better immediate post-operative bonding between lamina and HA was associated with a significantly higher probability of fusion (p=0.014) (Table 4).
Uni- and multivariate logistic regression analyses showed that male gender, diagnosis of OPLL, and wingless type of HA were statistically significant factors affecting 12-month post-operative fusion (Table 5).
Mean cervical lordosis, defined as the angle between C2 and C7 inferior end plates, changed from 11.73 to 10.95 degrees in the winged type group and from 12.27 to 18.11 degrees in the wingless type group (p=0.135) (Fig. 2).

A : Cervical lordosis, defined as the angle between C2 and C7 inferior end plates. B : Changes in cervical lordosis in the winged and wingless groups. Lordosis changed from 11.73 to 10.95 degrees in the winged type group and from 12.27 to 18.11 degrees in the wingless type group (p=0.135).
The spinal canal dimension was increased immediately after surgery, from 190.76 to 291.46 in the winged group and from 189.25 to 290.60 in the wingless group, but decreased to 276.77 and 276.93, respectively, after 12 months (p=0.970) (Fig. 3).
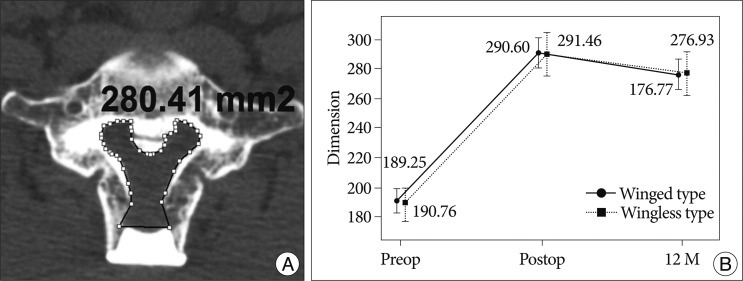
A : Spinal canal dimension measurements. B : The spinal canal dimensions increased immediately post-operatively in both groups, from 190.76 to 291.46 in the winged group and from 189.25 to 290.60 in the winged group, but decreased to 276.77 and 276.93, respectively, after 12 months (p=0.970).
The AP distance of the spinal canal on axial CT images was increased immediately after surgery from 11.52 mm to 19.22 mm in the wingless group and from 11.59 mm to 18.18 mm in the winged group, decreasing to 18.67 mm in the wingless group at 12 months, but remaining stationary, at 17.93 mm, in the winged group (p=0.021) (Fig. 4).
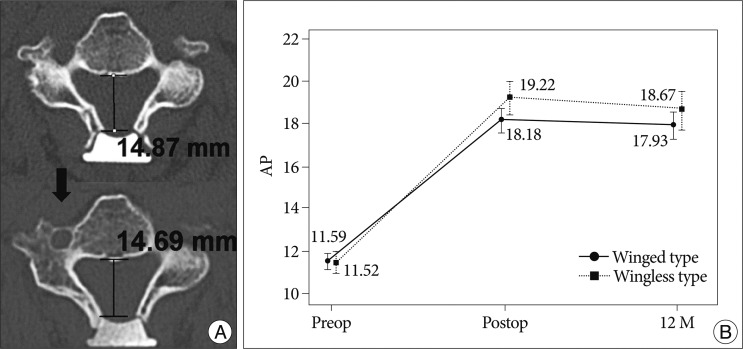
A : AP distance, as measured on CT axial image. (Upper image) immediate post-operative AP distance; (lower image) AP distance after 12 months. B : The AP distance of the spinal canal increased immediately after surgery from 11.52 mm to 19.22 mm in the wingless group and from 11.59 mm to 18.18 mm in the winged type group. After 12 months, the AP distances were 18.67 mm and 17.93 mm in the wingless and winged groups, respectively (p=0.021). AP : anterior-posterior, CT : computed tomography.
DISCUSSION
HA have several advantages compared with autologous bone grafts for expansive midline splitting laminoplasty, including good biomechanical stability and reductions in operation time, blood loss, and donor site morbidity8,12,14,15). Although HAs have been shown to be biocompatible and to fuse with lamina2-4,6,10), no previous study had analyzed the relationship between HA shape and outcomes. We therefore assessed the effects of HA shape (winged versus wingless) on clinical and radiological outcomes. As assessed by JOA scores, there were no significant between group differences in clinical outcomes, primarily because this clinical outcome was affected by decompression of the spinal cord. Moreover, there was no between group difference in post-operative expansion of spinal canal dimensions and subsequent dimensional reduction, suggesting that similar cord decompression resulted in similar clinical outcomes.
Regardless of HA shapes, our overall fusion rate (27.46%) between HA and lamina was similar to previous reports4,8). Although post-operative bonding between HA and lamina has been classified, its effect on final union was not assessed2). In contrast, we found that initial contact status between lamina and HA significantly affected fusion status. In addition, HA shape was significantly associated with initial contact status of HA with lamina. HA wings may limit the wide contact between HA and lamina, whereas the wingless type of HA can be inserted deeply into the split spinous process and form a wider contact with bone, resulting in a higher fusion rate 12 months later.
Multivariate analysis showed that male sex, OPLL, and wingless type of HA were significantly associated with higher HA fusion rate. Range of motion (ROM) is significantly lower with OPLL than with CSM, suggesting that the decreased ROM of OPLL provided the stabilization needed for fusion between the HA and lamina8). We also believe that better initial bonding status of wingless type HA seems to be contributing factor of higher fusion rate. However, the reason that fusion rates are higher in male than in female patients remains unclear.
In agreement with previous findings, we observed dimensional reduction of the spinal canal after immediate post-operative widening8). Our CT results showed that, when we used both type HAs, the tip of the spinous process tended to be resorbed and move inward slightly, resulting in canal narrowing (Fig. 5). We also believe that the dimensional reduction well correlate with reduction of AP distance in this study. Post-operative displacement of HA and resorption of the spinous process has been reported previously3,6). We observed a statistically significant difference in HA displacement between the two groups. HA wings may prevent its subsidence, while also preventing wider contact with bone and increase resorption of contacted bone, resulting in a lower fusion rate. Nevertheless, this structural difference was not associated with clinical outcomes.
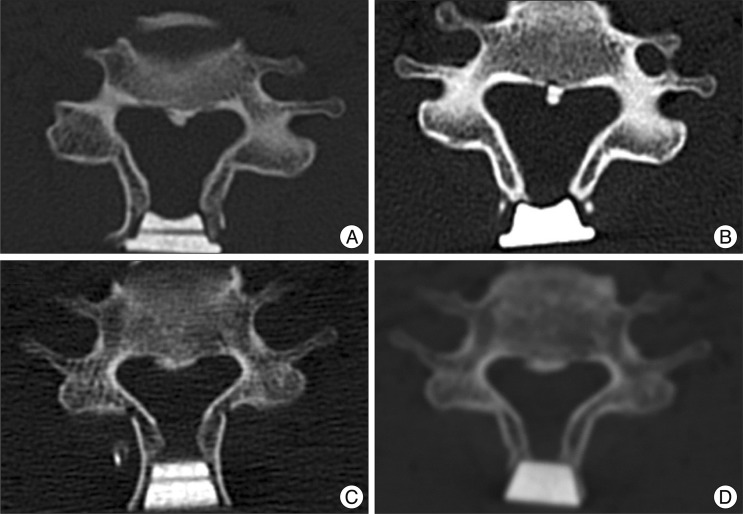
A : Immediate post-operative axial CT image in the winged type group showing good touch status. B : Post-operative 12 month axial CT in the same patient showing non-fusion and spinous process resorption. C : Immediate post-operative axial CT image in the wingless type group showing good touch status. D : Post-operative 12 month axial CT in the same patient showing fusion, but spinous process resorption. CT : computed tomography.
Although kyphotic deformities have been observed after laminoplasty in previous many studies, we observed maintenance of lordosis over 12 months in both groups, but additional follow up is needed5,7,17,19,20).
CONCLUSION
Although the two types of HA yielded similar clinical outcomes, their radiological outcomes differed. The changes of cervical lordosis and, canal dimension were not significantly different between winged and wingless typed HA. The AP distance change of wingless type showed bigger subsidence that of winged type. The wingless typed HA also showed significantly better fusion rate between lamina and HA after 12 months. Multivariate analysis showed that OPLL, male gender, and wingless type HA were significantly associated with fusion rate.
Acknowledgements
This research was supported by the Pioneer Research Center Program through the National Research Foundation of Korea funded by the Ministry of Education, Science and Technology (2012-0000447).