Intradural Extramedullary and Subcutaneous Tumors in Neonate : Atypical Myxoid Spindle Cell Neoplasm
Article information
Abstract
Tumors of the central nervous system are common in the pediatric population and constitute the second most prevalent tumor type in children. Within this group, spinal cord tumors are relatively rare and account for 1 to 10% of all pediatric central nervous system tumors. We describe a very rare case of an intradural extramedullary spinal cord tumor with a subcutaneous mass and discuss its clinical presentation, pathogenesis, and treatment. A male infant was delivered normally, with uneventful development. At 16 days post-delivery, his family took him to a pediatrician because of a mass on his upper back. Magnetic resonance imaging of the thoracic spine revealed a well-demarcated soft-tissue mass with central cystic change or necrosis at the subcutaneous layer of the posterior back (T2-7 level). Another mass was found with a fat component at the spinal canal of the T1-3 level, which was intradural extramedullary space. After six weeks, the spinal cord tumor and subcutaneous mass were grossly total resected; pathologic findings indicated an atypical myxoid spindle cell neoplasm, possibly nerve sheath in type. The final diagnosis of the mass was an atypical myxoid spindle cell neoplasm. The postoperative course was uneventful, and the patient was discharged after nine days without any neurological deficit. We report a rare case of an intradural extramedullary spinal tumor with subcutaneous mass in a neonate. It is necessary to monitor the patient's status by examining consecutive radiologic images, and the symptoms and neurological changes should be observed strictly during long-term follow-up.
INTRODUCTION
Tumors of the central nervous system are common in the pediatric population and constitute the second most prevalent tumor type in children. Within this group, spinal cord tumors are a relatively rare diagnosis and account for 1% to 10% of all pediatric central nervous system tumors8,10,15). Primary spinal cord tumors occur at a frequency of 0.19 per 100000 person-years, according to the Central Brain Tumor Registry of the United States4). Spinal cord tumors can occur at all levels of the spinal cord, but occur most frequently in the thoracic vertebra. These tumors are classified into three groups according to location : epidural, intradural extramedullary, and intradural intramedullary. The most common spinal cord tumors are intradural intramedullary2). Intradural extramedullary tumors are very rare. Intradural extramedullary tumors can be meningeal in origin or from distant sites, and include meningiomas and schwannomas. Of this group, most tend to be benign17). We describe a rare case of an intradural extramedullary spinal cord tumor with subcutaneous mass and discuss its clinical presentation, pathogenesis, and treatment.
CASE REPORT
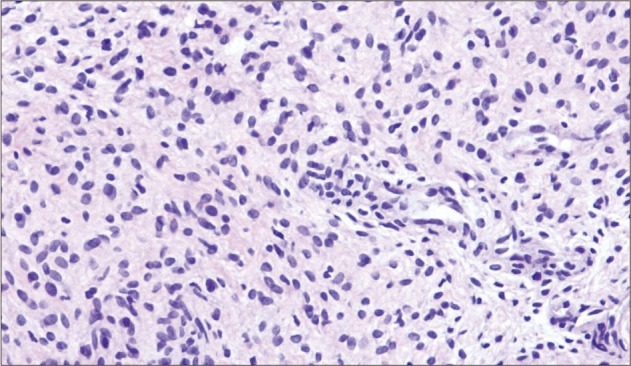
A male infant was delivered normally, with uneventful development. At 16 days post-delivery, his family took him to a pediatrician because of an upper back mass. He moved his extremities well and showed normal sensation and strength as well as deep tendon reflexs. Magnetic resonance imaging (MRI) of the thoracic spine revealed a well-demarcated soft-tissue mass with central cystic change or necrosis at the subcutaneous layer of the posterior back (T2-7 level). Another mass with a fat component at the spinal canal of the T1-3 level, the intradural extramedullary space, was also revealed (Fig. 1). An ultrasonography-guided needle biopsy was done at the subcutaneous mass. The histopathological diagnosis was a round and spindle cell neoplasm. After six weeks, another MRI was done (Fig. 1). The intradural extramedullary mass was increased, and the spinal cord was markedly compromised by the tumor mass. Thus, we decided to perform an operation. The operation was performed in the prone position. A midline vertical skin incision was made from about the C7 spinous process to the T7 spinous process, and the subcutaneous mass was noted. We removed the subcutaneous mass (Fig. 2), and a bilateral T1-4 laminectomy was performed. Upon opening, the exposed dura mater was tense. After opening the dura mater, a yellowish tumor was visualized. There was no firm attachment of the intradural extramedullary component of the lesion. Separation of the capsule and grossly total removal of the tumor was possible. The histopathological diagnosis was an atypical myxoid spindle cell neoplasm, possibly nerve sheath in type. Microscopic findings revealed that most of the lesional cells had ovoid, tapering, or wavy nuclei with rather neural-like morphology distributed in the myxoid or collagenous stroma (Fig. 3). In these areas, there was very striking perivascular whirling. Immunostaining was positive only for CD34, while S-100 protein, GFAP, and desmin were negative. The final diagnosis of the mass was an atypical myxoid spindle cell neoplasm. The postoperative course was uneventful, and the patient was discharged on day nine without any neurological deficit.
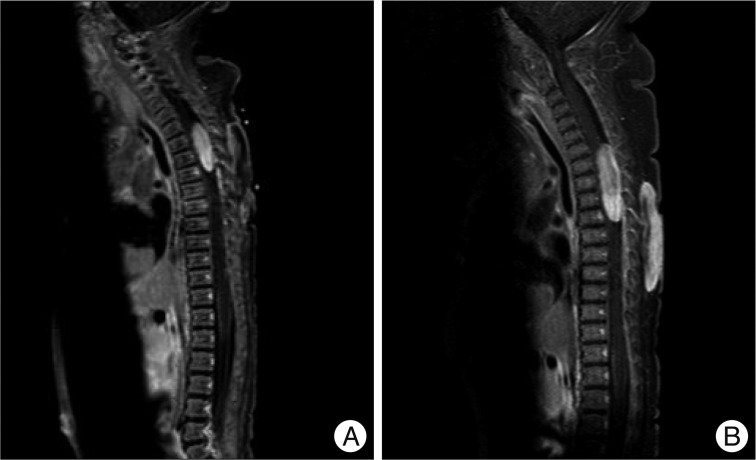
Preoperative sagittal T1-weighted gadolinium enhanced MRI of the thoracic spine showing the presence of an inhomogeneous high signal intradural mass between the T1 to T3 level, and another mass in the subcutaneous layer of the posterior back (T2-7 level). A : Initial MRI at 16 days post delivery. B : Follow up MRI at 58 days post delivery. Intradural extramedullary mass was increased, and the spinal cord was markedly compromised by the tumor mass. MRI : magnetic resonance imaging.
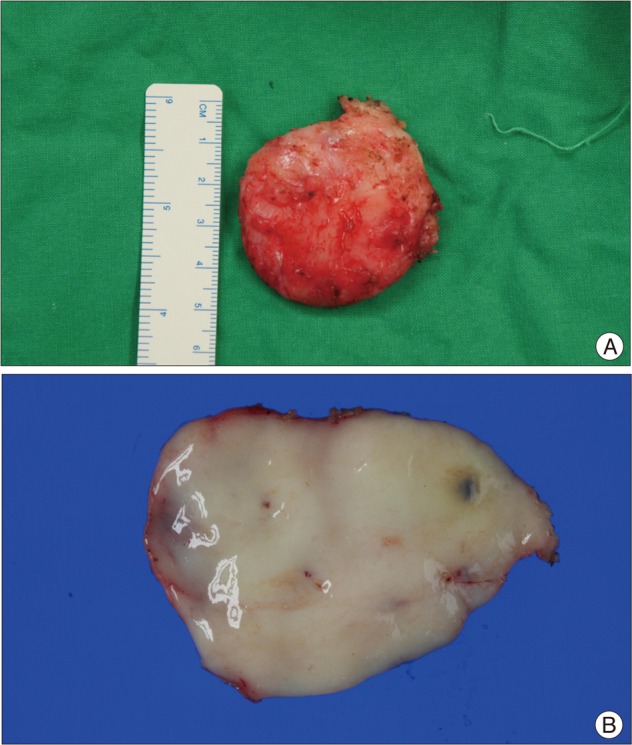
A : Photographs of the whitish and soft subcutaneous mass (5.0×4.0×0.8 cm). B : The cut surface shows a homogenous, whitish appearance.
DISCUSSION
Spinal cord tumors are a rare diagnosis in the pediatric population. In children, intradural extramedullary tumors are less frequent (between 5 and 10% of all central nervous system tumors)5). Coincidentally, intradural extramedullary tumors are pathologically benign in more than 90% of cases5,12). In contrast, intramedullary and extradural tumors are more frequently malignant11). Among all intradural extramedullary tumors, ependymomas constitute 29.6%, dermoid/epidermoid 23.8%, teratoma 15.8%, lipoma 13.1%, schwannomas 9.6%, and meningiomas 8.5%9). The symptoms and signs of intradural extramedullary spinal tumors are neither distinctive nor unique, and due to slow tumor growth and gradual displacement of the spinal cord, symptoms are frequently less than would be expected. In children, pain is the most common symptom, occurring in two-thirds of patients3). In very young children, localizing of pain may be difficult, but becomes apparent because of the child's general irritability or avoidance of certain positions. MRI is an important tool for the detection of intradural extramedullary tumors. Recognition of morphological patterns, signal intensities, and enhancement patterns frequently permit a specific diagnosis or a limited differential diagnosis. As most of these tumors are benign, the surgical goal is usually complete resection. Since Victor Horsley was credited with the first successful removal of a spinal cord tumor, remarkable progress has been achieved in spinal tumor surgery by neurosurgeons7). In the present case, an intradural extramedullary and subcutaneous mass occurred in a neonate. The patient was neurologically static for two months. The only symptom was an upper back mass. Cutaneous signs such as lipoma or dermal sinus associated with spinal dysraphism. The term spinal dysraphism encompasses many congenital anomalies of the spine, including meningocele, myelochisis, occult spinal bifida, diastematomyelia, diplomyelia, tethered conus, intraspinal lipoma, lipomyelomeningocele, dermoid cyst, and dermal sinus16). At first, we thought there was a connection between the subcutaneous mass and the intradural extramedullary mass. However, there was no connection, and each mass histopathological diagnosis was the same. This is the first reported case of an intradural extramedullary tumor with a subcutaneous mass. We grossly total surgical excision of the intradural extramedullary mass, which was causing cord compression, and completely removed the subcutaneous mass. The histopathological diagnosis is an atypical myxoid spindle cell neoplasm, possibly nerve sheath in type. Pathologists base the latter suggestion on the growth pattern and involvement of a nerve root. Given the infiltrative margin and overall appearances, somewhat concerned with low grade malignant peripheral nerve sheath tumor. Congenital inclusion tumor exist at birth but become overtly symptomatic later in life because of a characteristic slow growth14). But in present case tumor mass was rapidly growing. Infants are more likely to present with sole cutaneous stigmata and be neurologically intact than older children1).
Microsurgical resection for accessible and symptomatic intradural extramedullary cord tumors is the standard treatment. However, the potential adverse effect of surgery in the pediatric population is the risk of spinal deformity after laminectomy or laminoplasty. As a result of immature skeletal systems, younger children have a greater proportion of cartilage, increased ligamentous laxity, and more horizontally oriented facet complexes6). In addition to the growth of the spine, these features accentuate the alteration of spinal biomechanics caused by tumor resection with consequent spinal deformity6,13). Our patient was two months old when the surgery was performed, and he was only 16 days old at the time of the initial diagnosis. At that time, he had no neurological deficit. However, a follow-up MRI showed that the mass had increased and the spinal cord was compromised. The surgery performed successfully. Four months post-surgery, a follow-up MRI was done. There was no recurrence and no residual tumor. Six months after the surgery, development was appropriate for his age, with a good strength and range of motion in all extremities.
CONCLUSION
We report a rare case of an intradural extramedullary spinal tumor with a subcutaneous mass in a neonate. Spinal tumors are more likely curable with radical surgery in children. Early diagnosis and treatment improve postoperative outcome. It is necessary to monitor the patient's status by examining consecutive radiologic images, and the symptoms and neurological changes should be observed strictly during long-term follow-up.
Acknowledgements
This research was supported by the Yeungnam University research grants in 2010.