Microvascular Decompression for Primary Trigeminal Neuralgia : Short-Term Follow-Up Results and Prognostic Factors
Article information
Abstract
Objective
The aim of this prospective study was to demonstrate the influence of some factors on the prognosis of microvascular decompression in 37 patients with trigeminal neuralgia.
Methods
The results of microvascular decompression (MVD) in 37 patients with trigeminal neuralgia were evaluated at 6 months after surgery and were compared with clinical and operative findings.
Results
The sex of the patient, the patient's age at surgery, the side of the pain, and the duration of symptoms before surgery did not play any significant roles in prognosis. Also, the visual analogue scale (VAS) of the patient, the duration of each pain attack, and the frequency of pain over 24 hours did not play any significant roles in prognosis. In addition, intraoperative detection of the type of conflicting vessel, the degree of severity of conflict, and the location of the conflict around the circumference of the root did not play any roles in prognosis. The only factors affecting the prognosis in MVD surgery were intraoperative detection of the site of the conflict along the root and neuroradiological compression signs on preoperative magnetic resonance imaging (MRI)/magnetic resonance angiography (MRA).
Conclusion
These findings demonstrated that if neurovascular compression is seen on preoperative MRI/MRA and/or compression is found intraoperative at the root entry zone, then the patient will most likely benefit from MVD surgery.
INTRODUCTION
Trigeminal neuralgia (TN) is a neuropathic pain disorder characterized by episodes of intense pain in the face, originating from the trigeminal nerve. The primary treatment method for trigeminal neuralgia is medical treatment, but most cases develop tolerance to medical treatment over time. Based on the hypothesis that vascular compression is the cause of most cases of primary trigeminal neuralgia, a cure without the need for medical treatment can be achieved in the majority of patients with the microvascular decompression (MVD) technique. Although alternative surgical techniques (e.g., alcohol blockage, neurectomy, radiofrequency thermocoagulation, balloon compression, radiosurgery) are less invasive, it has been shown that these techniques have slightly higher recurrence rates5-7,14,24). MVD has some risks and is not always successful; the most appropriate treatment plan can be achieved by considering several prognostic factors, such as the age, clinical condition and preference of the patient. The aim of this prospective study was to demonstrate the influence of some factors on the prognosis of microvascular decompression in 37 patients with trigeminal neuralgia.
MATERIALS AND METHODS
Thirty-seven patients with primary trigeminal neuralgia were treated with MVD, without any lesioning or cutting of the adjacent rootlets, after August 2002 at the Neurosurgery Department of Erciyes University. All 37 cases were taking single or combined medical agents, which were recommended by physicians in several disciplines, before presenting at our clinic. These drugs included carbamazepine, oxcarbazepine, baclofen, gabapentin, and amitriptyline. The patients presented at our clinic because of the reduced effectiveness or adverse effects of these drugs. Twenty-five patients were using carbamazepine alone, while 12 were receiving combined therapy. Drugs were withheld during the postoperative period if pain was relieved.
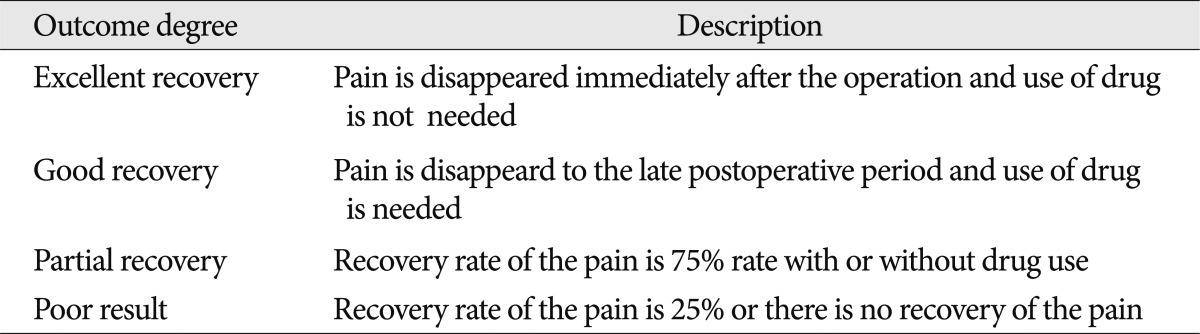
Clinical evaluations of these patients were performed preoperatively and at six months after the operation. Radiological evaluations were performed preoperatively period. Postoperative recovery was classified into four groups, as defined by Li et al.18) : excellent recovery, good recovery, partial recovery, and poor recovery (Table 1). The patients were assessed in two groups according to their duration of symptoms, as <12 months or >12 months; in three groups according to pain frequency over 24 hours, as <5, 5-10, and >10 pain episodes/24 hours; in three groups according to pain duration, as <2, 2-5, and >5 seconds; and in two groups according to visual analogue scale (VAS), as 0-5 and 5-10 points. Preoperative values were used to assess the grade of postoperative recovery. There were some exclusion criteria, including cases with intracranial masses, those who responded to medical therapy, those who were not operated on using pure MVD, and those who did not come to follow-up six months after their operations were excluded from the study.
Imaging protocol
Magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA) were performed before surgery. The images were assessed by an experienced neuroradiologist regarding compression of the fifth cranial nerve, not only at the REZ but also at the cisternal segment. The assessment of the presence of neuroradiological compression was based on the morphologic contact between the outer walls of the offending vessel and the trigeminal nerve. The degree of vascular contact with the trigeminal nerve was classified into the following categories: absence, contact, and compression (distortion or deviation of the nerve). Vascular compression or contact with the trigeminal nerve was considered an MRI-positive findings.
Surgical protocol
Under general anesthesia, a vertical skin incision posterior to the mastoid process was created, and a lateral suboccipital craniectomy was performed using the park-bench position. The trigeminal root entry zone was approached through a superolateral cerebellar route, and stretching of the acoustico-facial bundle was avoided. If the superior petrosal vein could not be saved, it was coagulated and divided 5 mm away from the root entry zone. The ipsilateral cerebellar hemisphere was retracted inferiorly, and the arachnoid membrane covering the fifth cranial nerve was opened. The fifth cranial nerve was exposed widely. After removing the conflicting vessel from the root, a Teflon graft was placed between the nerve and the conflicting vessel. If the vein was a conflicting vessel, it was divided and coagulated.
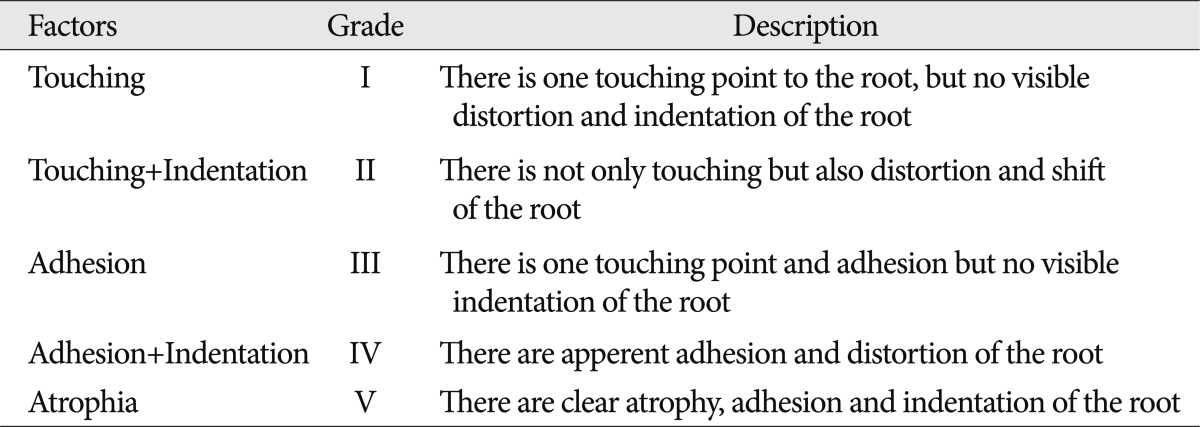
The anatomical details surrounding the trigeminal nerve were thoroughly recorded (type of conflicting vessel, degree of severity of conflict, site of the conflict along the root, and location of the conflict around the circumference of the root). When several conflicting vessels were found during the operation, only the main conflicting vessel was considered for the statistical analysis. The degree of severity of conflict was graded using the criteria defined by Li et al.18) : touching, touching+indentation, adhesion, adhesion+indentation, and atrophy (Table 2). The site of the conflict along the root was determined to be the root entry zone (REZ), middle third of the root, or Meckel's cave. Locations of the conflict around the circumference of the root were determined to be superior, inferior, anterior, or posterior.
Statistical analysis
Commercially available software was used to perform the data analysis. The results of qualitative data are expressed as percentages and quantitative data as means. Comparisons were performed using the chi-square test. A p<0.05 was considered statistically significant. For the statistical analysis, trigeminal neuralgia was considered cured when complete recovery was accomplished. Good recovery, partial recovery, and poor results were considered failures.
RESULTS
The sex and age of the patient, side (left or right), past history (months), daily frequency of pain (times), duration (seconds), VAS of the pain, and neuroradiological compression signs on preoperative MRI are presented in Table 3. The type of conflicting vessel, degree of severity of conflict, site of conflict along the root, and location of the conflict around the circumference of the root were detected intraoperatively and are presented in Table 4. Of the 37 cases with primary TN, full recovery was achieved in 28 cases (75.6%), whereas good recovery in occurred in two cases (8.9%), partial recovery in five cases (11.1%), and poor results in two cases (4.4%) at the follow-up visit at postoperative month 6 after the MVD operation.
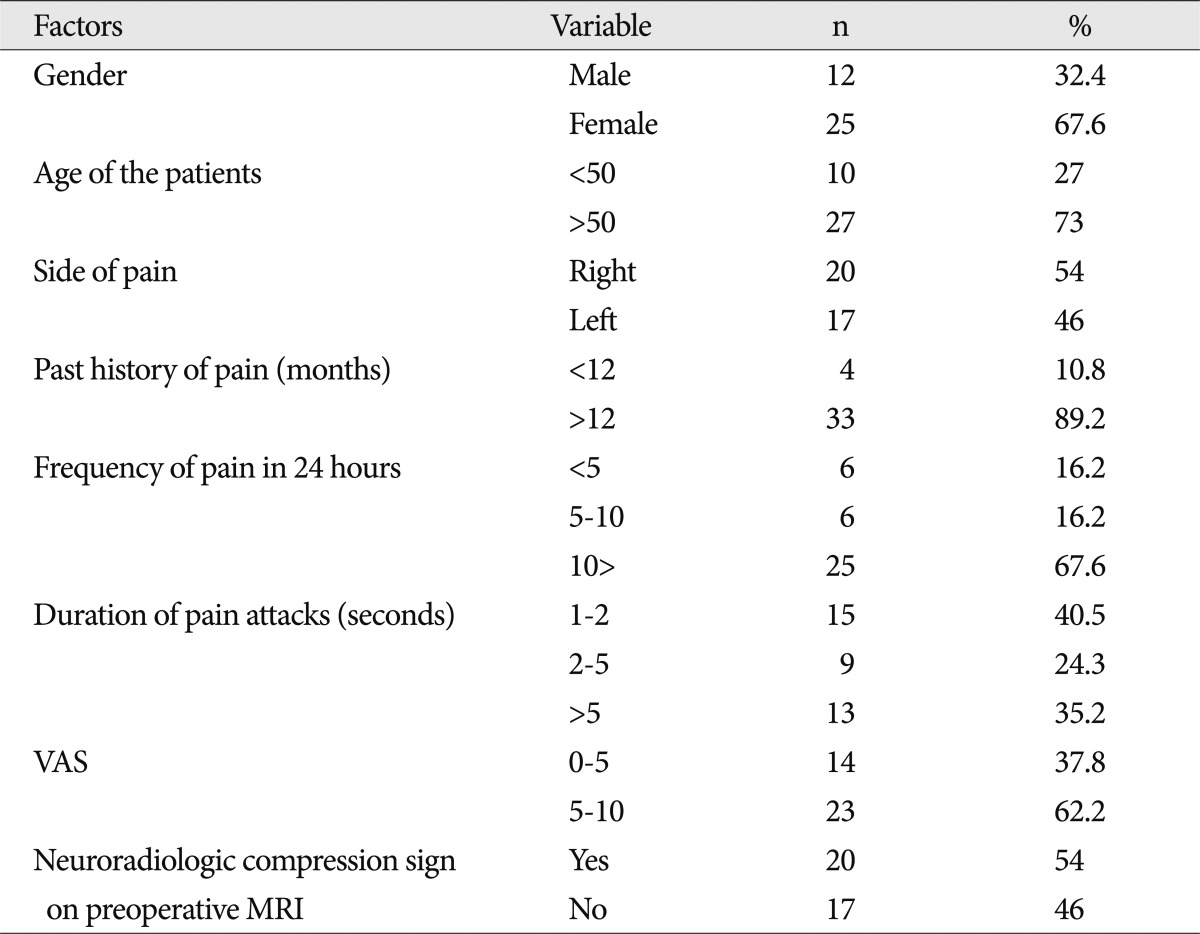
Table showing gender and age of the patients, side, past history, daily frequency, duration and VAS of the pain, and neuroradiological compression sign on preoperative MRI
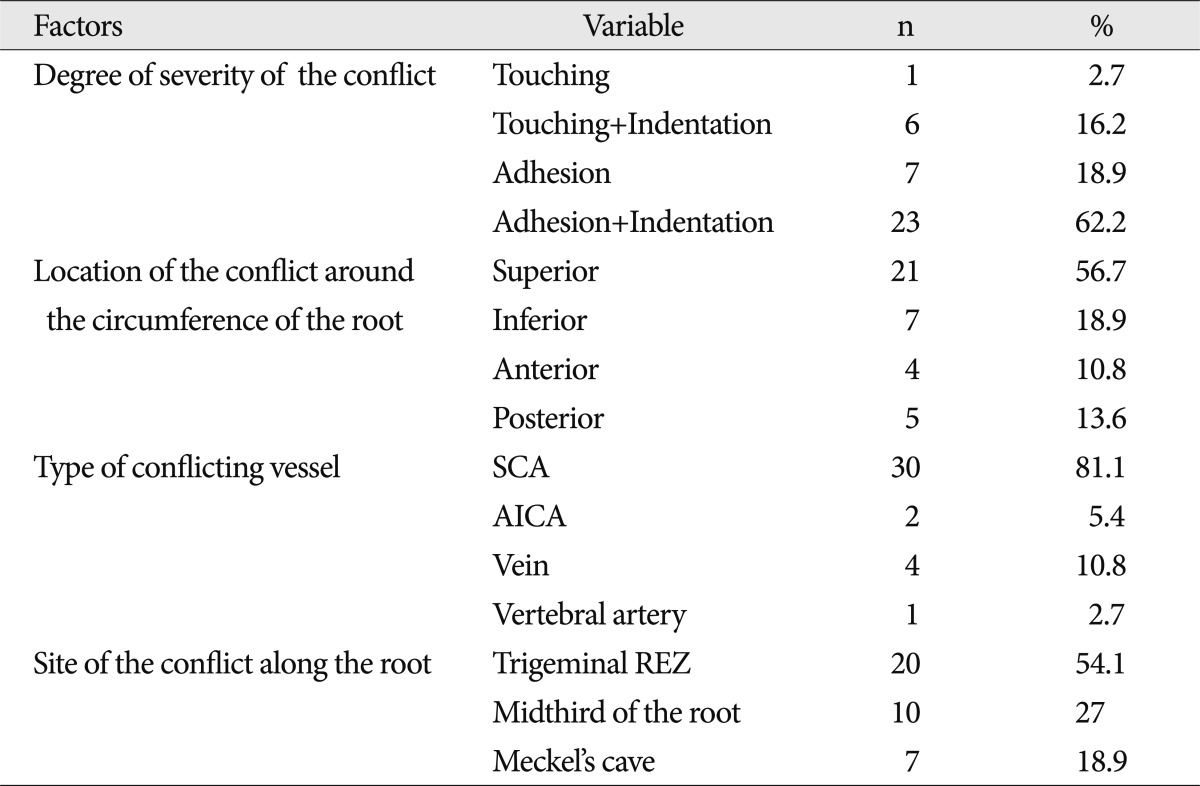
Table showing intraoperatively detected type of conflicting vessel, degree of severity of conflict, site of the conflict along the root and location of the conflict around the circumference of the root
Of the 37 MVD cases, there were 25 women (67.6%) and 12 men (32.4%). The median age was 53.6 years old (range: 29-66 years); there were 10 patients (27%) younger than 50 years of age and 27 patients (73%) older than 50 years of age. Pain was localized on the left side in 17 patients (46%) and on the right side in 20 cases (54%). No significant differences were detected between post-operative recovery grade and sex, age of the patient, and localization of the pain (p>0.05) (Table 5). When symptom duration was considered, it was found that there were four cases (10.8%) in the group with symptom duration <12 months and 33 cases (89.2%) in the group with symptom duration >12 months. No significant differences were detected between post-operative recovery grade and symptom duration of pain (p>0.05).
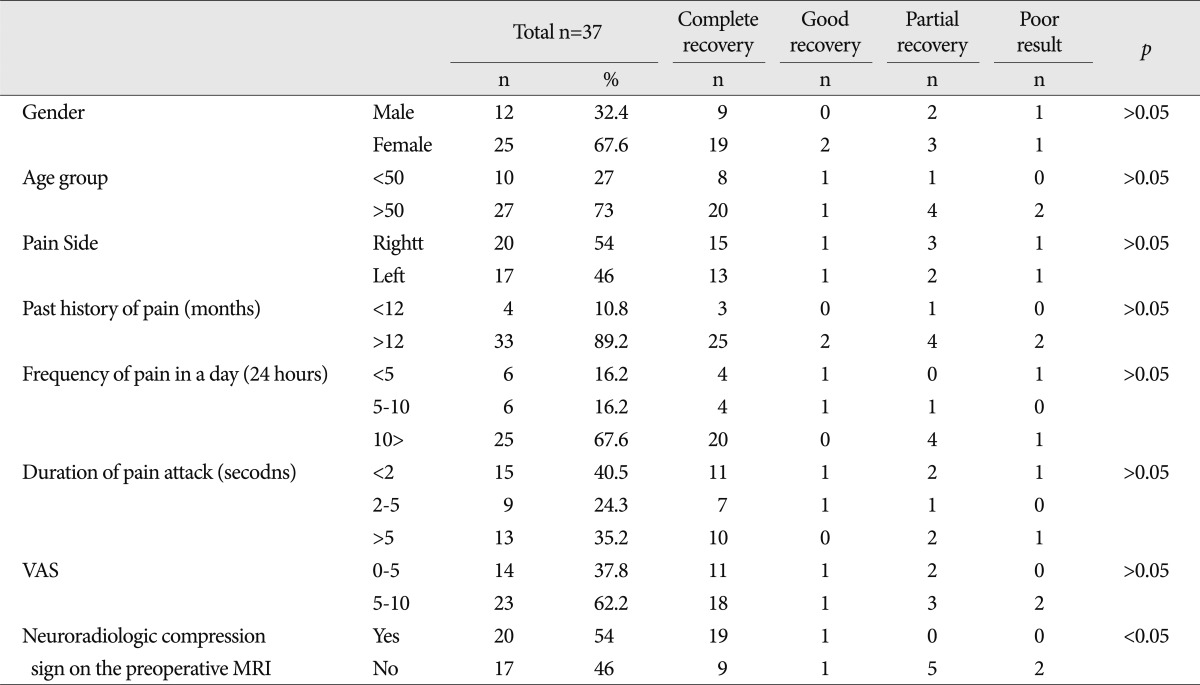
Table showing the statististical correlation between outcome after surgery and gender and age of the patients, side (left or right), past history (months), daily frequency (times), duration (seconds) and VAS of the pain, and neuroradiological compression sign on preoperative MRI
When daily pain frequency was assessed, there were six cases (16.2%) in the group with the frequency <5, six cases (16.2%) in the group with a frequency of 5-10, and 25 cases (67.6%) in the group with a frequency of >10 episodes. No significant differences were detected between post-operative recovery grade and daily frequency of pain (p>0.05) (Table 5). When pain duration was considered, there were 15 patients (40.5%) with pain duration <2 seconds, 9 patients (24.3%) with pain duration of 2-5 seconds, and 13 patients (35.2%) with pain duration >5 seconds. No statistical differences were detected between pain duration and postoperative recovery grade (p>0.05) (Table 5). When VAS was considered, there were 14 patients (37.8%) with a VAS of 0-5 and 23 patients (62.2%) with VAS of 5-10 (62.2%). No statistical differences were found in the analysis of VAS and postoperative recovery grade (p>0.06) (Table 5).
Of the 37 MVD cases, the vessel causing compression was the superior cerebellar artery in 30 cases (81.1%), the AICA in two cases (5.4%), and the vertebral artery in one case (2.7%) and a vein compression was detected in four cases (10.8%). The degree of severity of compression to the nerve was detected as follows: touching in one case (2.7%), touching+indentation in six cases (16.2%), adhesion in seven cases (18.9%), and adhesion+indentation in 23 cases (62.2%). The location of the conflict around the circumference of the root was superior in 21 cases (56.7%), inferior in seven cases (18.9%), anterior in four cases (10.8%), and posterior in five cases (13.6%). No significant relationship was found between surgical outcome and the type of the conflicting vessel (p>0.05), the degree of severity of the conflict (p>0.05), or the location of the conflict around the circumference of the root (p>0.05) (Table 6).
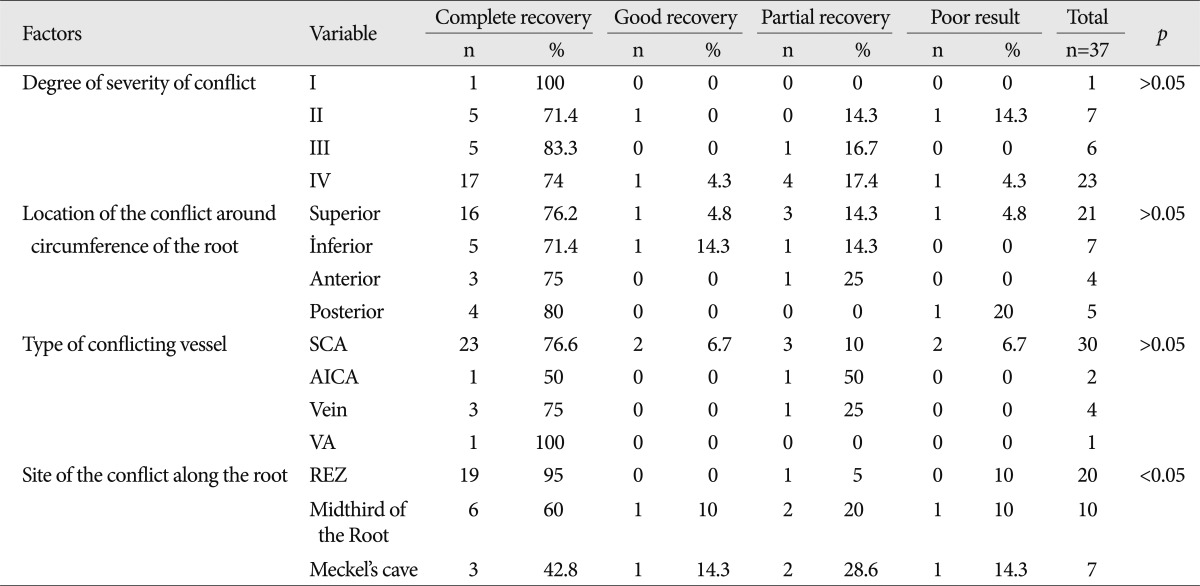
Table showing the statististical correlation between outcome after surgery and intraoperatively detected type of conflicting vessel, degree of severity of conflict, site of the conflict along the root and location of the conflict around the circumference of the root
On preoperative MRI, neuroradiological compression signs were found in 20 cases (54%), and in 17 cases (46%), there was no sign of compression on preoperative MRI. A significant relationship was found between the presence of compression on preoperative MRI and surgical outcome (p>0.05) (Table 5). In all 37 cases, there was compression of the trigeminal nerve intraoperatively. According to the compression site, there was compression at the REZ in 20 cases, at the middle third of the root in 10 cases, and at Meckel's cave in seven cases. A significant relationship was detected between postoperative recovery and compression at the REZ; a favorable effect on postoperative recovery was detected in patients with compression at the REZ (p>0.05) (Table 6).
There was hearing loss in one case, which was recovered at post-operative month 2. Psychosis developed in one case, which was treated medically. Wound infection occurred in two cases, which recovered with appropriate antimicrobial therapy. Facial hypoesthesia developed in one case, which was found to be significantly improved at the follow-up visit at postoperative month 6.
DISCUSSION
Primary TN is a neuropathic disorder characterized by episodes of intense pain in the face, originating from the trigeminal nerve. In primary TN, pain episodes usually continue for few seconds or minutes. Episodes may occur at any time, and they are not only triggered by sensorial stimulation of face but also by motions (e.g., chewing or yawning). Continuous, pulsatile, severe pain at the distribution of the trigeminal nerve is not considered primary TN. Non-specific terms, such as "atypical TN" or "secondary TN," have been proposed to name these non-primary trigeminal neuralgias. The differences between primary and secondary TN have not been identified clearly and reliably2). Secondary TN is a general term, which is used to identify facial pain discrepant from the presentation of primary TN. With such a diagnostic system, there is a risk of neglecting some cases that normally would be treated, by classifying them as secondary neuralgia2).
Despite the small sample size, vascular compression was detected in all 37 patients (100%) who underwent MVD in the present study. Currently, several surgical procedures are available for the treatment of TN that is resistant to medical therapy. Among these, MVD, defined by Janetta10-13), seems to be the most ideal procedure, as MVD targets the etiology in most primary TN cases and can relieve pain while causing little or no facial loss. However, this method also includes certain important disadvantages. Because a mortality of 1% was reported in almost every study, including many cases, and because postoperative complications and nerve injury occur to considerable degrees, this surgery should be performed by only experienced surgeons in this field.
MRA has 100% sensitivity and 96% specificity in the diagnosis of TN. If abnormal vascular contact is detected in TN cases by using MRI/MRA, this results in a successful MVD operation15-17). In the present study, vascular compression of the fifth cranial nerve was preoperatively detected in 20 cases using MRI/MRA. In all 37 cases, there was compression of the trigeminal nerve intraoperatively. Successful outcomes of MVD surgery were achieved in 95% of these cases. Regarding neurovascular compression, there was a discrepancy between MRI/MRA and surgical findings. Failure to identify neuroradiological compression on MRI/MRA was noted in the cases with compression of veins and small arteries or with distal compression.
MVD is recommended to patients younger than 65 years of age without significant medical or surgical risk factors20). Hilton et al. suggested that MVD is a safe and effective method in the treatment of primary TN. The high success rate in the long term makes MVD an attractive choice in persistent TN cases. Although TN is not sufficiently understood and is a matter of debate in terms of the underlying mechanism, most cases respond well to surgical decompression of the trigeminal nerve root9,21-23). MVD causes less damage to the fifth cranial nerve when compared to other methods. Another advantage of MVD is its low risk for significant sensorial deficits and dysesthesia of the facial region. According to consecutive case series at principal centers, MVD relieved pain in more than two-third of the cases and caused sensorial loss of the facial region in 1% at 10-year follow-up19).
Although a postoperative success rate of up to 95% was seen with MVD for TN, surgical outcomes worsen over time The recurrence rates were 1.5% and 3% in two series1,4). The reasons for recurrence in TN cases include continuing elongation of vessels, the presence of a new vessel that compresses the nerve, re-canalization of a vein that has been cauterized but not dissected, atrophy of implanted muscle, and Teflon adhesion. It was reported that patients with severe compression had better prognoses than those with mild compression1). However, no effect on prognosis was detected for compression degree in this study. Burchiel et al. reported that symptom duration had no effect on prognosis3). Also, we detected that symptom duration had no significant effect on prognosis.
Although rare, cases of TN also exist that are not caused by focal vascular compression. The cause in such cases may be focal compression (and associated myelin loss) affecting a part of nerve but not recognized during surgery9). Because all of our cases showed compression intraoperatively, we may hypothesize that vascular compression of the trigeminal nerve, especially at the REZ, is the main etiological factor in primary TN8,20).
CONCLUSION
Considering the prognostic factors for trigeminal neuralgia, it was observed that surgical outcomes were better in cases in which vascular compression was detected on preoperative MRI/MRA and when the compression occurred at the REZ region intraoperatively. If preoperative MRI/MRA shows a vascular conflict and/or the surgeon finds this conflict at the REZ region, the patient most likely will benefit from MVD surgery. These findings also demonstrated the role of vascular compression of the trigeminal nerve, especially at the REZ, in the etiology of trigeminal neuralgia.
Acknowledgements
We are very grateful to Prof. Ahmet Menkü and thank him for his valuable contributions.