A Textiloma on the Pterion : A Rarely Occurred Craniotomy Complication
Article information
Abstract
Textiloma is an inflammatory mass containing surgical sponges that are unintentionally left behind in a surgical wound. This complication has been most commonly described by abdominal and gynecologic surgeons. However, the occurrence of textiloma after intracranial procedures especially under the temporalis muscle has not been documented. The author reports a rare case of textiloma of the pterion in a patient who presented with a subcutaneous tumor developed eight years after frontotemporal craniotomy for aneurysm clipping.
INTRODUCTION
Textiloma is a term used to describe a foreign-body reaction to the retained material routinely used during operations such as cotton or gauze. Textilomas are inflammatory granulomas that often mimic residual or recurrent tumors or abscesses clinically or radiologically. A study involving 254 cases of textilomas showed common occurrences in the order of abdomen (56%), pelvis (18%), thorax (11%), and limb (7%), spine (4%), and head and neck (4%)10). In contrast, the existence of textilomas after craniotomies has been observed in a limited number of studies. The author reports the first case of textiloma due to retained gauze that was left under the temporalis muscle eight years ago in a patient who underwent pterional craniotomy for ruptured aneurysm.
CASE REPORT
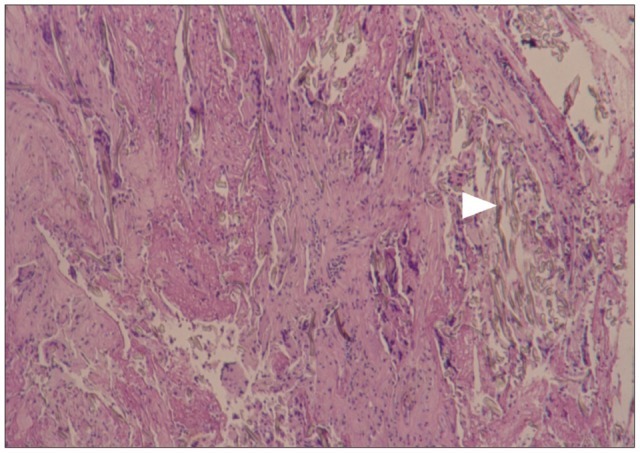
A 64-year-old woman complained of a painful expansion in the temporal region that she had first noticed five months previously. This patient underwent left pterional craniotomy 8 years earlier for a ruptured aneurysm. There were no complications at the time of her operation. On examination, a well-circumscribed, firm, raised scalp mass at the area of previous craniotomy was defined. Computed tomography (CT) showed a tomb-like isodense lesion having a moderate enhancement under the musculo-cutaneous flap (Fig. 1). Thus, a second surgery was performed. A piece of gauze encapsulated by a large amount of granulation tissue was found at the layer between temporalis muscle and dura through surgical defect of calvarium (Fig. 2). Histopathological study confirmed cotton fibers surrounded by a granulomatous foreign body reaction (Fig. 3). She continued to do well after wound revision.

Computed tomography of a textiloma developed after pterional craniotomy for aneurysm clipping. Nonenhanced (A) and enhanced (B) scans show an isodensity of homogeneous mass with a peripheral contrast enhancement in the temporalis muscle (arrow).

Intraoperative appearance of the lesion demonstrates an osseous defect and a mass of granulation tissues adherent to the temporalis muscle (arrow). The lesion is extending into the underlying dura mater.
DISCUSSION
Retention of surgical materials within wounds has been reported to occur with a frequency of one in 5000 for all operations3). Among them, textilomas in the fields of neurosurgery have been found to appear after spinal surgery7), craniotomies for trauma6), tumor resection1), clot evacuation9), cotton wrapping of aneurysms5), and microvascular decompression2). The vast majority of reported postcraniotomy textilomas were subdural lesions10).
Intraoperatively applied foreign materials can cause infection or abscess formation in the early stage, whereas others mostly remain asymptomatic for many years8). Chronic cases of fibrinous textiloma like the present one involves slow adhesion formation such as encapsulation and granuloma. They are often overlooked or can be confused with other soft-tissue masses. Time to discovery in this case, 8 years, was much longer because of the high likelihood of intracranial textilomas related complications within the first 2 years after surgery1,2,5,6,9). Being sterile, the surgical cottons do not initiate an infective reaction and thus remain clinically silent and missed for a long duration in the postoperative period until they are thought of. After a certain period, when the patient's resistance decreases or a bout of bacteremia ensues, organisms will lodge into the area of the foreign body and a sterile inflammatory reaction will turn symptomatic. This may be associated with tooth extraction or throat infection or after a flu-like syndrome. A continuing foreign body granulomatous reaction may be speculative explanation for this case that presents late as a progressively enlarging mass in the temporalis muscle.
In contrast with other lesions, intracranial and spinal textilomas sometimes show early severe symptoms like neurologic deficit, pain or seizure. Patients with textilomas after craniotomy for tumors are at risk of unnecessary treatment because these lesions manifest as recurrent tumors. Patients with textilomas could in fact show more aggravated symptoms due to the mass effect of granuloma after microvascular decompression for cranial rhizopathy. Furthermore, spine surgeons may mistake textilomas for recurrent disc herniations in some cases. However, the present case showed only bulging on the surgical wound without neurological deterioration. This was quite different from most patients who underwent pterional craniotomy and experienced remarkable depression in the frontozygomatic fossa.
Imaging is essential to the workup for textilomas, and the common differential diagnosis includes primary, metastatic, recurrent tumor, radiation necrosis or abscess. Suggested CT findings are low-density heterogeneous masses with a hyperdense rim that was further enhanced after contrast injection like the present case, and sometimes they present with a spongiform pattern containing air bubbles6). The signal intensity of magnetic resonance imaging may vary according to aging, histologic composition, and its fluid content. Almost all lesions are hypointense on T1-weighted images and hyperintense on T2-weighted images, but textilomas cannot be easily distinguished from a recurrent tumor or abscess due to their less characteristics8). Therefore, careful history taking about previous operations and being aware of textiomas are very important for imaging diagnosis.
An increased risk of a foreign body retainment after craniotomy was highly correlated with emergency cases, unexpected changes in operations, and inaccurate counts of sponges and instruments, involvement of more than one surgical team, and patients with a high body-mass index4). Although textilomas are rarely encountered under the temporalis muscle, these must always be considered in the differential diagnosis of cranial masses arising after craniotomy. Early second-look surgery may be advised to ascertain the diagnosis for certain cases, especially when unusual progression of the intra- and extracranial lesion is seen during treatment or routine follow-up. This lifts the burden of uncertainty from both the patient and the physician and allows for a more conservative treatment.
CONCLUSION
The author reports a case of textiloma under the temporalis muscle found in the second surgery performed 8 years after the first. The rarity of postcraniotomy extracranial textilomas and their nonspecificities in the imaging features preclude preoperative diagnosis. The occurrence of a textiloma following craniotomy can only be avoided by surgeons who are aware of this uncommon but clinically significant event.