Chronic Subdural Hematoma after Eccentric Exercise Using a Vibrating Belt Machine
Article information
Abstract
We report a case of bilateral chronic subdural hematoma (CSDH) in a 75-year-old man after exercise using a vibrating belt machine on the head. He suffered from headache and intermittent left side numbness for ten days. He denied any head injuries except eccentric exercise using a vibrating belt on his own head for 20 days. An MRI revealed bilateral CSDH. The hematoma was isodense on the CT scan. We made burr-holes on the both sides under local anesthesia. We identified the neomembrane and dark red subdural fluid on both sides. In the postoperative CT scan, we found an arachnoid cyst on the left temporal pole. Although the arachnoid cyst itself is asymptomatic, trivial injury such as vibrating the head may cause a CSDH.
INTRODUCTION
Chronic subdural hematoma (CSDH) occurs mainly in the aged. Although a history of head trauma is absent in 25 to 50% of these cases, mild head injury is the cause of most CSDHs. Often trivial injuries, such as ordinary sports activities, riding a roller coaster or even head banging were reported as the trauma inducing CSDH. However, exercise using a vibrating belt machine is a unique trauma causing CSDH. We report a case of bilateral CSDH after eccentric exercise using a vibrating belt on the head.
CASE REPORT
A 75-year-old man presented with a headache and intermittent left side numbness from 10 days ago. He had suffered from hypertension, diabetes mellitus, renal insufficiency and gout. On admission, he was in a relatively normal status without any significant neurological deficit. We suspected transient ischemic stroke, so we performed magnetic resonance imaging (MRI). On MRI, the T1-weighted IR images revealed bilateral subdural isointense collections (Fig. 1A). On T2-weighted SE and T2-FLAIR images, bilateral subdural collections showed hypointensity (Fig. 1B, C). We also performed gradient-echo T2-weighted MR imaging. The image of the right side collection was more prominently hypointense than the left side (Fig. 1D). Bilateral hematomas were appeared as homogeneous lesion without multilayered or lobulated structure. Besides, arachnoid cyst was appeared on left temporal pole (Fig. 1E, F).
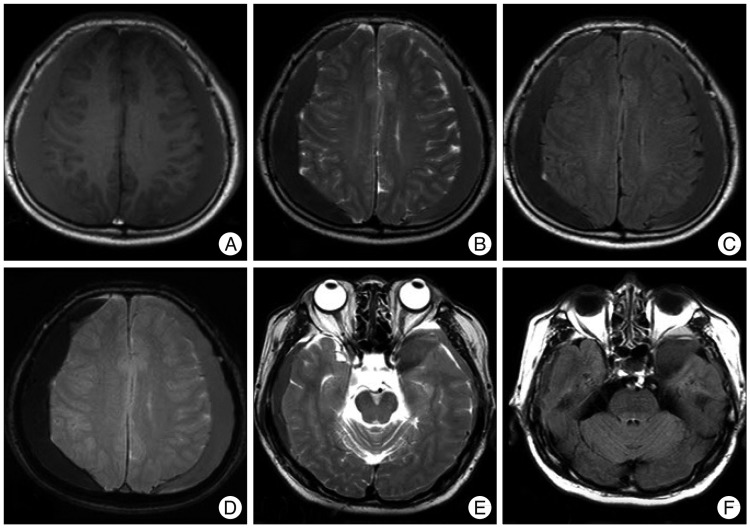
(A) T1-weighted image reveals bilateral subdural isointense collections, (B) T2-weighted SE and (C) T2-FLAIR image reveals bilateral subdural collections with hypointensity, (D) Gradient echo T2-weighted image reveals bilateral hematomas with different signal intensities; the right side is more hypointense than the left side, (E) T2-weighted SE image shows arachnoid cyst on the left temporal pole, (F) T2-FLAIR image shows arachnoid cyst on the left temporal pole.
We also obtained computed tomographic (CT) scans. The CT scan revealed thick crescent homogeneous isodensity lesions in both fronto-temporo-parietal regions without midline shift (Fig. 2).
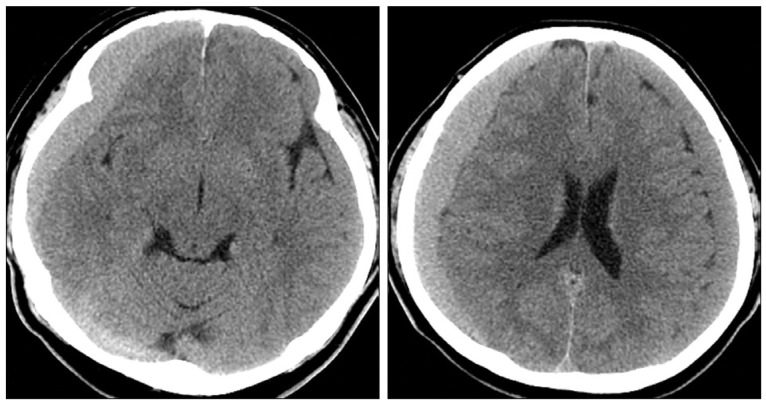
CT scans reveal thick crescent homogeneous isodensity lesions in both fronto-temporo-parietal regions without midline shift.
Based on the CT and MR findings, we could diagnose as bilateral CSDH. We tried to obtain any trauma history in detail again. However, the patient did not have even a minor trauma, except for using a vibration belt massage to his own head for 20 days.
He was treated by burr-holes in the both parietal regions. We could identify the subdural neomembrane on both sides. Dark red fluid was evacuated from both sides. We kept silastic drainage tubes for 24 hours, which were removed on the next day. Postoperatively, CT scan revealed removal of CSDH with subdural air. We could find an arachnoid cyst (AC) on the left temporal pole which was unnoticed on the preoperative CT scan (Fig. 3).

Postoperative CT scans reveal nearly total removal of chronic subdural hematoma. We could identify an arachnoid cyst on the left temporal pole which is unnoticed on the preoperative CT scan (arrow).
The patient discharged to home after release of symptoms. Follow-up CT scans obtained 2 months after surgery, revealed an asymptomatic recurred CSDH on the left fronto-temporo-parietal region (Fig. 4). An AC was remained on the left temporal pole.

Follow-up CT scans 2 months later reveal recurred subdural hematoma on the left side. An arachnoid cyst is still found on the left temporal pole.
On 5 months after surgery, the recurred CSDH was completely resolved spontaneously (Fig. 5). However, the AC was still found on the left temporal pole.
DISCUSSION
Bilateral CSDHs were found in this 75-year-old man with an AC after eccentric exercise using a vibrating belt on his head. Some sports related subdural hematomas associated with AC have been reported in both contact and noncontact sports17). In the case of noncontact head trauma, the brain injury can be explained by translation, rotation, or angular motion of the head, causing acceleration and deceleration of the brain4). This pathophysiology was described in CSDH cases attributed to roller coaster rides, capoeira, basketball, racing, jumping, football and head banging3,4,6,7,11-13,15,16).
Beneath the dura, the pia-arachnoid complex (PAC) is a very important anatomical structure of the brain. During head impact or inertial loading, the relative motion (i.e. separation and sliding) between the inner skull and brain will result in a tangential shear loading on PAC layer. Although studies on the injury thresholds based on the biomechanics of head motion questioned the causal relationship between CSDHs and roller coaster rides14), it is not easy to get the threshold sufficient to separate the dural border cell layer or to tear fragile vessels. In general, mechanical properties of cerebral tissues vary widely both inter- and intraspecies and are inhomogeneous, non-linear, and rate dependent. Even without any trauma or predisposing conditions, subdural bleeding might result from a sudden increase in intravenous pressure18). A sudden alteration of the intracranial pressure, such as forcible exhalation, blowing, Valsalva maneuver, coughing, defecation, lifting a heavy weight, or systemic vascular hypotension may cause the rupture of bridging dural veins. Vibrating belt on the head may cause these motions, which can produce shearing forces on bridging veins, causing bleeding1,8), especially in patients with AC.
In general, CSDH is shown as more hyperintense region than normal brain tissue on both T1- and T2- weighted MRI10). Previous reports suggested that TI values of CSDHs were shorter than gray matter and longer than white matter, and T2 values were longer than normal brain tissue5,9,10).
The MR signal is due to the chemical change of hemoglobin to methemoglobin. The presence of methemoglobin in bloody CSF stored hypoxically for 3 days and methemoglobin caused T1 shortening in aqueous solution due to combined inner-sphere and outer-sphere effects2). In this case, both subdural collections were isointense on the T1-weighted and hypointense on the T2-weighted SE and T2 FLAIR images. These findings suggest both subdural hematomas were in chronic stage. However, intensity difference on gradient-echo T2-weighted images suggests that the left side hematoma contains more CSF component.
CONCLUSION
We report a case of bilateral CSDH after eccentric exercise using a vibrating belt machine on the head. Acceleration or deceleration of the brain induced by vibration may cause subdural bleeding especially in patients with AC. Exercise using a vibrating belt machine is a unique trauma causing CSDH. Although the AC itself is asymptomatic, trivial injury such as vibrating the head may cause a CSDH.
