Assessment of Recanalization after Intra-Arterial Thrombolysis in Patients with Acute Ischemic Stroke : Proposed Modification of the Qureshi Grading System
Article information
Abstract
Objective
We aimed to investigate the correlation between the success of recanalization and a modified version of the Qureshi grading system in acute ischemic stroke patients.
Methods
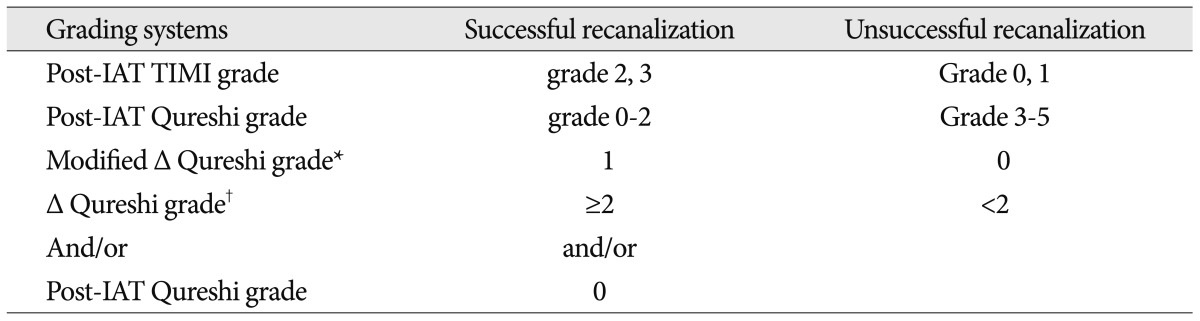
We retrospectively analyzed the intra-arterial thrombolysis (IAT) records of 37 patients who were evaluated by Thrombolysis in Myocardial Infarction (TIMI) and a modified version of the Qureshi grading systems as follows : 1) post-IAT Qureshi grade, 2) modified Δ Qureshi grade : pre-IAT group grade - post-IAT group grade (grade 1 : Qureshi grades 0-2 and grade 2 : Qureshi grade 3-5) and 3) Δ Qureshi grade (post-IAT Qureshi grade - pre-IAT Qureshi grade). Successful recanalization was defined as follows : 1) post-IAT TIMI grades 2 and 3, 2) post-IAT Qureshi grade 0-2, 3) modified Δ Qureshi grade=1, and 4) Δ Qureshi grade of ≥2 and/or post-IAT Qureshi grade=0. We investigated the correlation between the post-IAT TIMI grade and the modified Qureshi grade and also compared the various grading systems with modified Rankin Scale scores for evaluating the clinical outcome at 3 months.
Results
The post-IAT Qureshi grade and Δ Qureshi grade and/or post-IAT Qureshi grade were significantly correlated with the TIMI grade (γ=0.976 and, 0.942, respectively). Further, post-IAT Qureshi grade and Δ Qureshi grade and/or post-IAT Qureshi grade showed a significantly stronger association with clinical outcome than did the post-IAT TIMI grade (p=0.001 and, 0.000 vs. 0.083, respectively).
Conclusion
Our preliminary results suggest that the modified Qureshi grading system is a useful tool for assessing the success of recanalization after IAT.
INTRODUCTION
Evaluating the reestablishment of distal blood flow is an immediate predictor for assessing treatment success after intra-arterial thrombolysis (IAT)14,16). However, recanalization does not necessarily imply clinical success; the success of recanalization and the clinical benefit obtained in ischemic stroke patients cannot be correlated on the basis of any previous studies.
While, several studies have reported a general relationship between recanalization and good clinical outcome, this relation is known to be complex and is dependent on several interactive variables, including baseline stroke severity, lesion volume, location of arterial occlusion, time from stroke onset, and collateral blood flow11,15).
Several grading systems have been developed in an attempt to quantify recanalization rates after IAT. The Thrombolysis in Myocardial Infarction (TIMI) grading system has been widely accepted and is used either in its original or modified form10,13). Another modification of the TIMI grading scheme, the Thrombolysis in Cerebral Infarction (TICI), has recently been proposed5). The TIMI system was originally adopted for describing flow in the coronary arteries13). Therefore, these grading systems do not account for the site of occlusion and presence of collateral flow, both of which are important parameters in successful recanalization after IAT. To counter this, Qureshi9) proposed a new grading system primarily based on the angiographic appearance of occlusion, which incorporates the anatomic site of occlusion and the collateral flow to the affected region.
However, there are no definite criteria for assessing the success of recanalization after IAT; since this issue is not addressed by any currently used grading system, a new grading system is needed. In this study, we investigated the correlation between recanalization and a modified version of the Qureshi grading system; further, we have proposed a set of criteria for evaluating the success of recanalization based on our proposed modification of the Qureshi grading systems.
MATERIALS AND METHODS
The study protocol was approved by the institutional review boards. The study population comprised 37 consecutive patients undergoing urgent IAT for acute ischemic stroke between January 2008 and October 2009. We retrospectively analyzed the clinical data and records of these patients. A stroke neurologist evaluated all the patients with acute ischemic stroke presenting to the emergency room within 6 h from the onset of symptoms. Patients with persistent neurological deficit following intravenous thrombolysis were also included in our study. We reviewed the patient's clinical records, radiologic findings, and various factors associated with ischemic stroke. The following data were collected : National Institutes of Health Stroke Scale (NIHSS) score at presentation; modified Rankin Scale (mRS) score at 3 months; mortality; brain computed tomographic scan at presentation and after completion of thrombolysis, age; sex; past history of hypertension, diabetes mellitus, hyperlipidemia, atrial fibrillation and coronary artery disease; time interval between the onset of symptoms and initiation of IAT; location of thrombus; collateral circulation; post-IAT TIMI grade; modified Qureshi grade; and post-IAT symptomatic hemorrhage.
The Qureshi grading system uses the following grades for occlusion : 0 (no occlusion), 1 (1 branch vessel occlusion), 2 (2 branch vessels occlusion), 3A or 3B (M1 stem occlusion with preserved or lost lenticulostriate vessels), 4A or 4B [internal carotid artery (ICA) or basilar artery (BA) occlusion with collaterally supplied antegrade or retrograde flow], and 5 (complete ICA or BA occlusion)9). We modified the Qureshi grading system as follows : 1) post-IAT Qureshi grade, 2) modified Δ Qureshi grade : pre-IAT group grade - post-IAT group grade (grade 1 : Qureshi grades 0-2 and grade 2 : Qureshi grade 3-5) and 3) Δ Qureshi grade (post-IAT Qureshi grade - pre-IAT Qureshi grade).
The criteria for successful recanalization after IAT were as follows : 1) post-IAT TIMI grades 2 and 3, 2) post-IAT Qureshi grade 0-2, 3) modified Δ Qureshi grade=1, and 4) Δ Qureshi grade of ≥2 and/or post-IAT Qureshi grade=0 (Table 1).
Clinical outcome was assessed by clinical examination using the mRS score at 3 months after stroke. We defined mRS scores of 0-3 as favorable, and mRS scores 4-6 as poor outcomes. Death corresponded to a mRS score of 6.
We investigated the correlation between post-IAT TIMI and the modified Qureshi grading systems. Further, we compared the rate of successful recanalization based on the grading systems with mRS scores at 3 months.
For comparison of baseline variables between different grading systems, the chi-square test was used for categorical variables; and Student's t-test for continuous variables. The correlation between the TIMI grade and the modified Qureshi grade was analyzed using κ statistics. A probability value less than 0.05 was considered statistically significant.
RESULTS
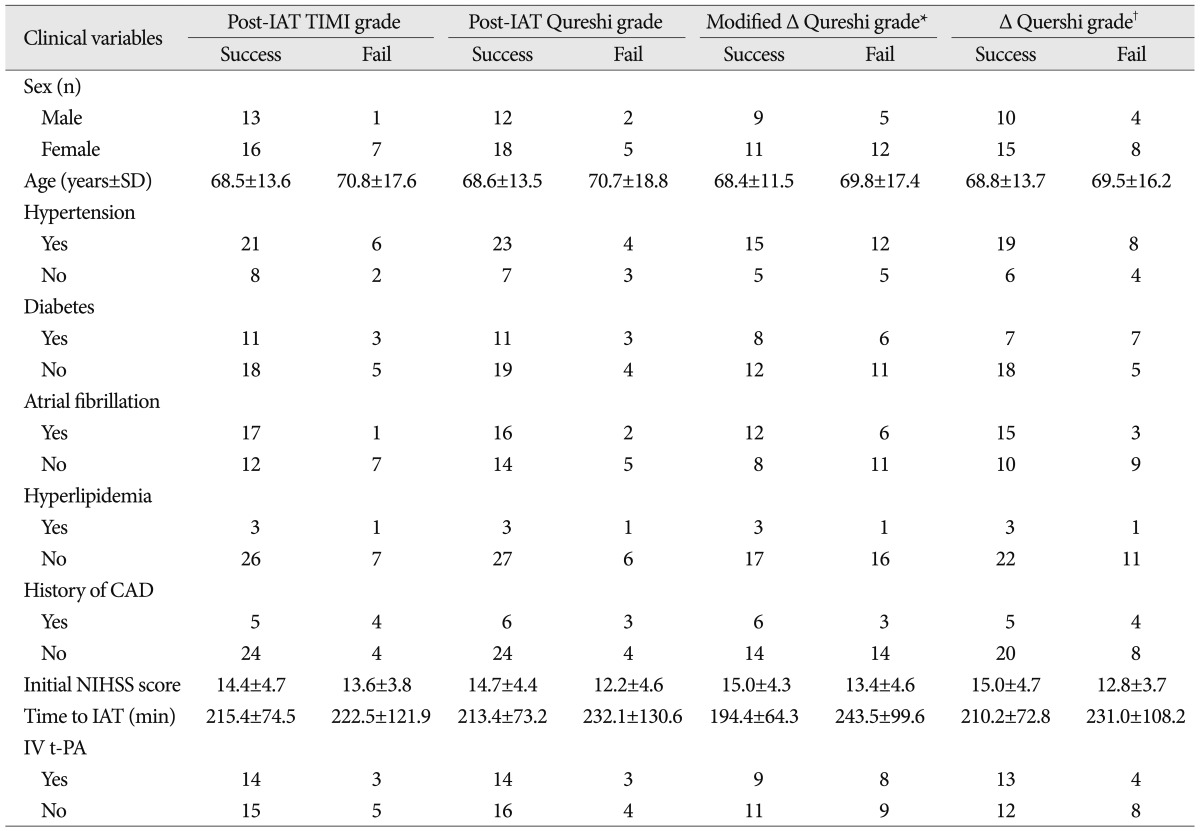
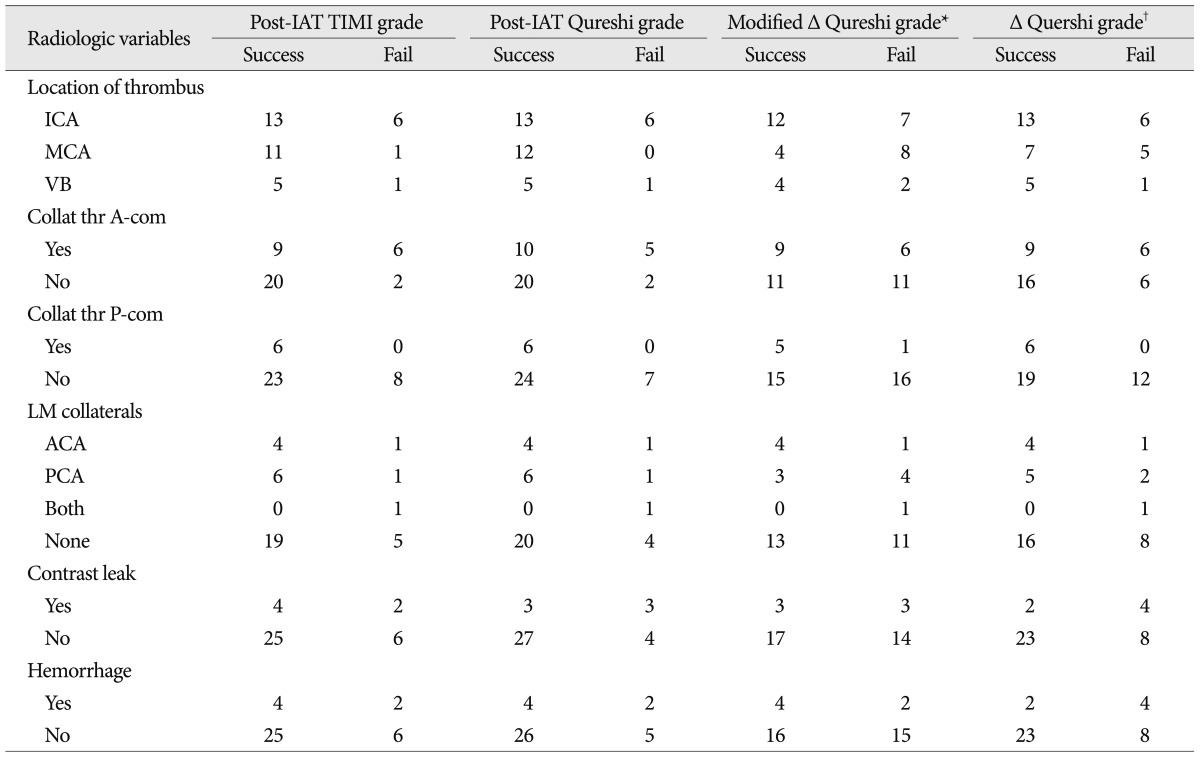
We analyzed 37 patients (14 men, 23 women) with a mean age of 69±14 years. The median baseline NIHSS score on admission was 14 (range 5-24). The median time from symptom onset to initiation of IAT was 217 min. The occlusion sites were ICA (n=19), middle cerebral artery (n=12), and vertebrobasilar artery (n=6). There were no significant differences in the demographic, clinical or angiographic variables among the different grading systems (Table 2, 3).
Successful recanalization was achieved with the following grades : post-IAT TIMI grade, n=29 (78.4%); post-IAT Qureshi degrade, n=30 (81.1%); modified Δ Qureshi grade, n=20 (54.1%); and Δ Qureshi grade and/or post-IAT Qureshi grade, n=25 (67.6%) (Table 4).
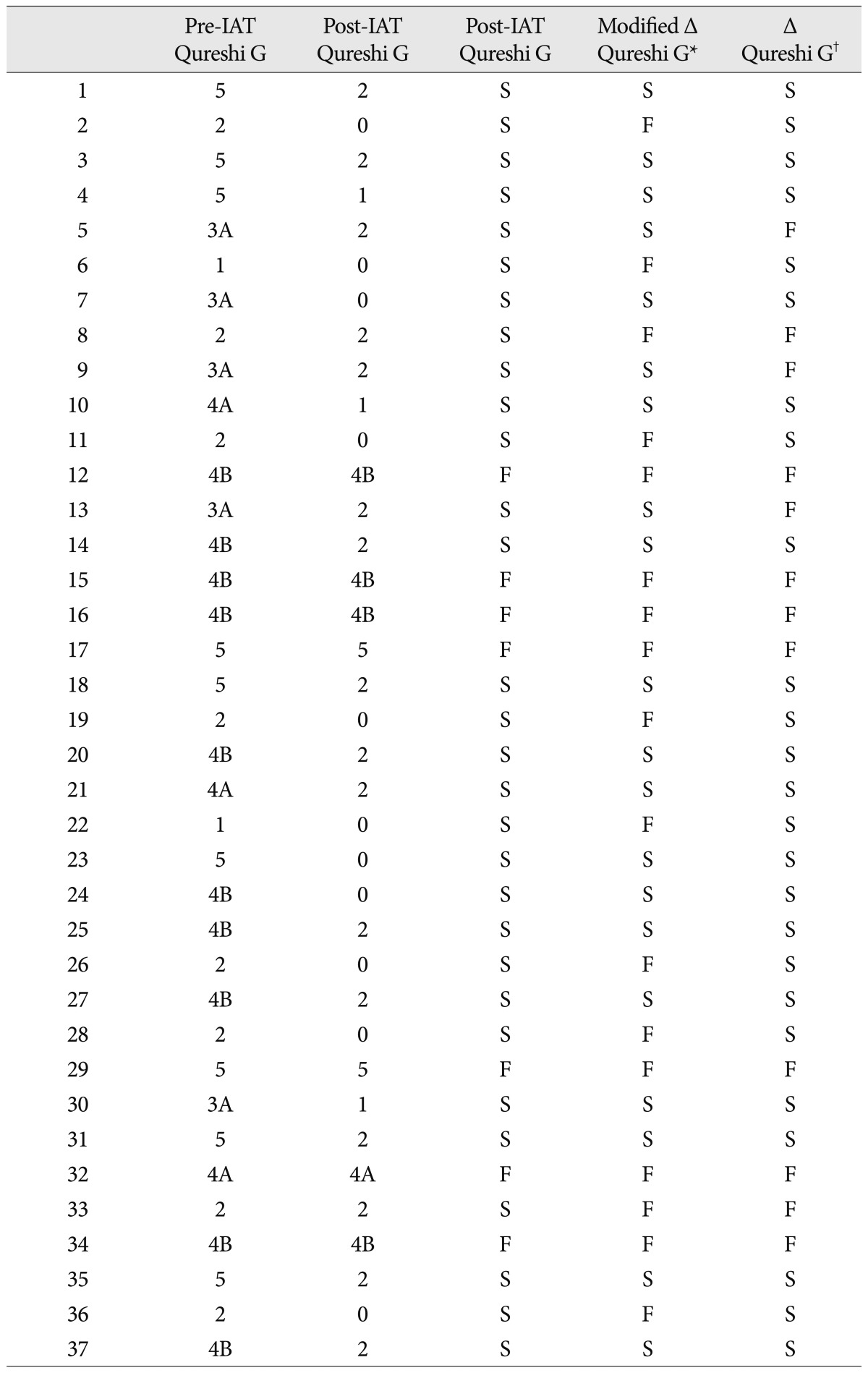
Pre- and post-intra-arterial thrombolysis Qureshi grade and results of recanalization in the consecutive 37 patients
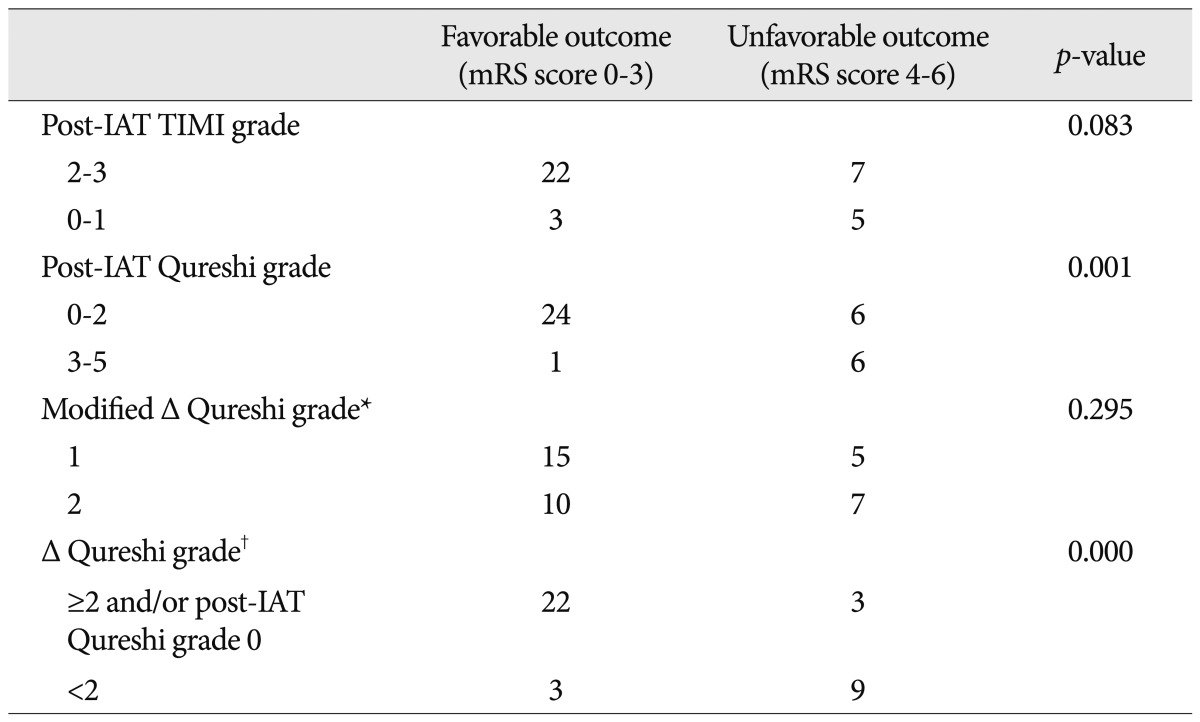
The correlations with post-IAT TIMI grade were significant for the post-IAT Qureshi grade and Δ Qureshi grade and/or post-IAT Qureshi grade 0 (γ=0.976 and 0.942, respectively) (Table 5).
The mRS score after three months was ≤3 in 25 patients (67.6%), indicating a favorable outcome, while 12 patients (32.4%) had a poor outcome (mRS score=4-6); of these 12 patients, 5 (13.5%) died. 6 patients (16.2%) suffered a symptomatic intracerebral hemorrhage. The clinical outcome was favorable in 3 of the 8 patients (37.5%) with post-IAT TIMI grades 0-1 and in 22 of the 29 (75.8%) patients with post-IAT TIMI grades 2-3 (p=0.083). Moreover, a favorable outcome was noted in 30 patients (80%) with post-IAT Qureshi grades 0-2 and in 1 of 7 patients (14.2%) with post-IAT Qureshi grades 3-5 (p=0.001). The outcome was also favorable in 15 of 20 patients (75%) with successful modified Δ Qureshi grade as compared with an unsuccessful grade (58.8%) (p=0.295). 22 of 25 patients (88%) with successful Δ Qureshi grade and/or post-IAT Qureshi grade 0, and 3 of 12 patients (25%) with unsuccessful grade had a favorable outcomes (p=0.000) (Table 6).
DISCUSSION
In this study, we proposed a modified Qureshi grading system that concurrently evaluates the degree of recanalization before and after IAT to help predict successful recanalization and clinical outcome in a patient undergoing IAT for acute ischemic stroke.
Recanalization is considered a surrogate marker for predicting clinical outcome in stroke trials14,16). Therefore, clinically reliable standards need to be established for assessing the severity of acute arterial occlusion and response to treatment. Mori et al.8) described a grading system that assessed both recanalization and reperfusion following intravenous thrombolysis. The TIMI score described distal flow perfusion and revascularization before and after treatment and became a standard for reporting the efficacy of reperfusion therapy. Higashida et al.5) attempted to standardize the reporting of flow restoration and described thrombolysis in cerebral infarction, TICI score. However, in these studies, the methods of assessment of recanalization differ considerably, rendering the comparison of each study with the others difficult. Further, these grading systems did not specifically take into account the location of the arterial occlusion or deinscribe collateral blood flow, both of which are major determinants of stroke outcome1,3,9,12).
To overcome these shortcomings, Qureshi9) suggested a grading scheme based on the location of the arterial occlusion and the presence or absence of collateral blood supply. Subsequent reports have noted a significant association between the Qureshi grading scheme and the initial severity and outcome of stroke as well as the subsequent volume of brain infarction6,7). Interobserver agreement for pre- and post-IAT angiography has been demonstrated to be higher using the Qureshi grading system than either the TIMI grading or Mori classification systems9). Accordingly, a neurointerventionist or physician can use the Qureshi grading system rapidly and conveniently for assessing the severity of arterial occlusion and for determining the length of the procedure and its termination in emergency situation.
A grading scheme that can be used to quickly and reliably measure the angiographic severity of occlusion as well as the response to treatment is necessary. To emphasize the use of a standard grading system for IAT specific to the intracranial cerebral circulation, we have proposed the modified Qureshi grading system in this paper. Our modified system makes it possible to assess the vascular patency before and after IAT simultaneously. Before obtaining a successful model, we dichotomized the Qureshi grading scheme (grades 0-2 and 3-5) with grades 0-2 at procedure termination considered as successful recanalization. However, this simple dichotomy may overestimate the rate of successful recanalization for occlusion of M2, A2, and posterior cerebral artery. Therefore, we modified the Qureshi grading system as follows : group grade 1 (Qureshi grades 0-2) and 2 (grades 3-5). We simply subtracted the pre-IAT group grade from the post-IAT group grade. Successful recanalization was considered as a value of 1. This strict grading method may underestimate the rate of successful recanalization for occlusion of the proximal or distal ICA and vertebrobasilar artery. Further, this grading method did not correlate with the clinical outcome or TIMI grades. Therefore, the definition applied in the Desmoteplase in Acute Ischemic Stroke and Dose Escalation of Desmoteplase for Acute Ischemic Stroke trials for characterizing successful recanalization was used2,4). Successful recanalization was defined as an improvement of ≥2 points on the Qureshi grading scheme after IAT as compared to the pre-IAT grade or Qureshi grade 0 after IAT. This modification of the Qureshi grading scheme correlated significantly with the TIMI grade; further, the modified grading system also demonstrated a better correlation with the clinical outcome than did the TIMI grade.
The modified Qureshi grading system described here provides a more objective method for assessing the final results of recanalization. For example, Qureshi grade 3 after IAT is simply considered as unsuccessful recanalization according to the modified Δ Qureshi grade. However, according to the Δ Qureshi grade, it would be considered as successful recanalization in a patient with pre-IAT Qureshi grade 5. Unfortunately, we did not encounter such a patient in our series. A further study will help in elucidating whether Qureshi grade 3 can be truly considered as successful recanalization in a patient with pre-IAT Qureshi grade 5.
Our study has certain limitations in our study, apart from the inherent limitations of a retrospective study. First, the single-center effect precludes general conclusions that can be applied interinstitutionally. The second limitation is the lack of consistency in the thrombolysis regimens used to treat the 37 acute ischemic stroke patients, who were treated with 4 different regimens (intravenous and IA pharmacological therapy, IA pharmacological and mechanical therapy, and all 3 together). This issue may degrade the prognostic value of the modified grading system.
CONCLUSION
These preliminary results suggest that the modified Qureshi grading system would be a useful tool for assessing the success of recanalization after IAT, which demonstrates a better correlation with the clinical outcome than does the TIMI grading system. Additional validation studies will be needed before this modified Qureshi grading system can be universally adopted.