Long Term Outcomes of Gamma Knife Radiosurgery for Typical Trigeminal Neuralgia-Minimum 5-Year Follow-Up
Article information
Abstract
Objective
Gamma knife radiosurgery (GKRS) is the least invasive surgical option for patients with trigeminal neuralgia (TN). However, the indications and long term outcomes of GKRS are still controversial. Additionally, a series with uniform long-term follow-up data for all patients has been lacking. In the present study, the authors analyzed long-term outcomes in a series of patients with TN who underwent a single GKRS treatment followed by a minimum follow-up of 60 months.
Methods
From 1994 to 2009, 40 consecutive patients with typical, intractable TN received GKRS. Among these, 22 patients were followed for >60 months. The mean maximum radiation dose was 77.1 Gy (65.2-83.6 Gy), and the 4 mm collimator was used to target the radiation to the root entry zone.
Results
The mean age was 61.5 years (25-84 years). The mean follow-up period was 92.2 months (60-144 months). According to the pain intensity scale in the last follow-up, 6 cases were grades I-II (pain-free with or without medication; 27.3%) and 7 cases were grade IV-V (<50% pain relief with medication or no pain relief; 31.8%). There was 1 case (facial dysesthesia) with post-operative complications (4.54%).
Conclusion
The long-term results of GKRS for TN are not as satisfactory as those of microvascular decompression and other conventional modalities, but GKRS is a safe, effective and minimally invasive technique which might be considered a first-line therapy for a limited group of patients for whom a more invasive kind of treatment is unsuitable.
INTRODUCTION
Trigeminal neuralgia (TN) is a debilitating pain syndrome that is characterized by agonizing, paroxysmal, and lancinating pain. The recommended first-line treatment for TN is medical therapy, but this often fails to provide pain relief. Thus, second-line treatment modalities are given to patients whose symptoms are intractable or who cannot tolerate medication. These treatment modalities include invasive procedures such as microvascular decompression (MVD), and ablative procedures such as gamma knife radiosurgery (GKRS), percutaneous balloon microcompression, radiofrequency rhizotomy, and glycerol rhizolysis. GKRS is an attractive surgical modality for TN14). Recently, GKRS has been used as a treatment modality in several centers for patients with concurrent medical illness who are poor candidates for MVD or who refuse more invasive surgery17,20). Other treatment modalities provide short-term pain relief at a rate of 80-90%; GKRS also produces short-term alleviation of pain at similar rates, usually within 6-12 months after the operation2,3,7,9,11,15,18,23,29-31). Pain relief after MVD and radiofrequency rhizotomy for long-term periods has been well reported. In previous studies, patients who underwent MVD and radiofrequency reported favorable long-term pain relief of for more than 5 years1,5,10,25,28,32). However, long-term outcomes of GKRS for TN have been published in only a few reports12,22,29). Thus, we conducted the present study to analyze the long-term outcomes in a series of patients with TN who underwent single GKRS treatment and were followed up for a minimum of 60 months.
MATERIALS AND METHODS
Between March 1995 and March 2009, 40 patients with typical TN underwent GKRS at our clinic. Indications for GKRS included medically intractable pain, >65 years of age, refusal of invasive procedures, or failure of previous invasive procedures. Among them, we retrospectively reviewed the medical records of patients with TN undergoing GKRS treatment that had a minimum follow-up of 60 months. Patient demographic characteristics, clinical presentation, treatment history, and the radiosurgical modality were reviewed in 22 patients whose median follow-up was 92.2 months (range : 60-144 months).
All patients were treated with Leksell Gamma Knife (Eleckta Instruments, Stockholm, Sweden) under local anesthesia. As a planning tool, the KULA system was used until 2001, and the Leksell Gamma Plan System (Eleckta AB, Stockholm, Sweden) has been used since 2001. All patients were treated using a single isocenter through a 4-mm collimator helmet targeting the root entry zone of the trigeminal nerve (Fig. 1). Maximum doses ranged from 65.2-83.6 Gy. The mean maximal dose to the target was 77.1 Gy (range, 65.2-83.6 Gy).
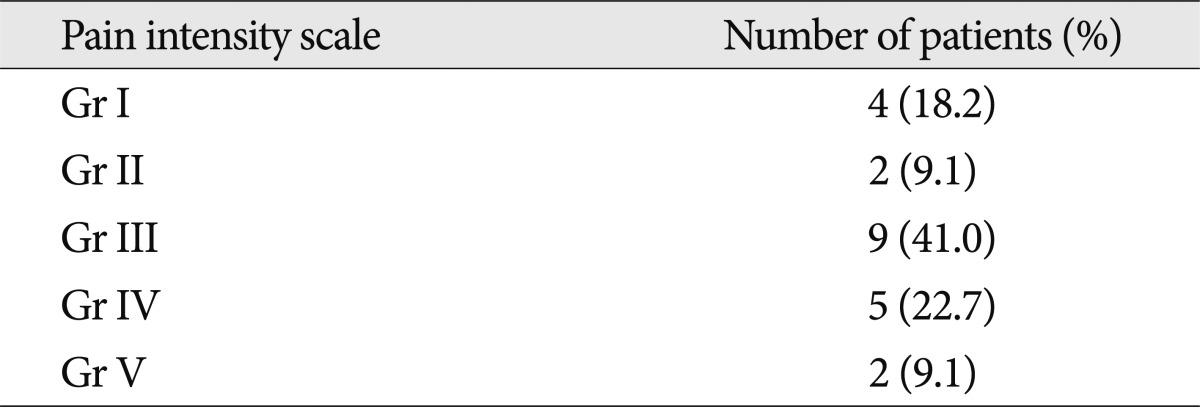
Long-term outcomes were established by face to face interview with a written questionnaire after the treatment in the outpatient clinic. The questionnaire was devised based on the Barrow Neurological Institute (BNI) pain scale24) but modified at our institution to better incorporate the use of adjuvant medications. Facial pain outcomes were categorized into one of the following classes : grade I, no pain, no medication; grade II, no pain with medication; grade III, >50% improved pain with medication; grade IV, ≤50% improved pain with medication; and grade V, no pain relief. Patients with grade I-II on the pain scale (equivalent to BNI grades I and IIIa) were considered to have a good treatment outcome. Patients with grade IV-V on the pain scale (equivalent to BNI grades IV and V) were considered to have a poor treatment outcome (Table 1). Descriptive statistics were determined by standard methods for calculation of median or mean values. Statistical verification was determined using SPSS statistic software, version 13.0 (SPSS, Inc., Chicago, IL, USA). A p value <0.05 was accepted as statistically significant.
RESULTS
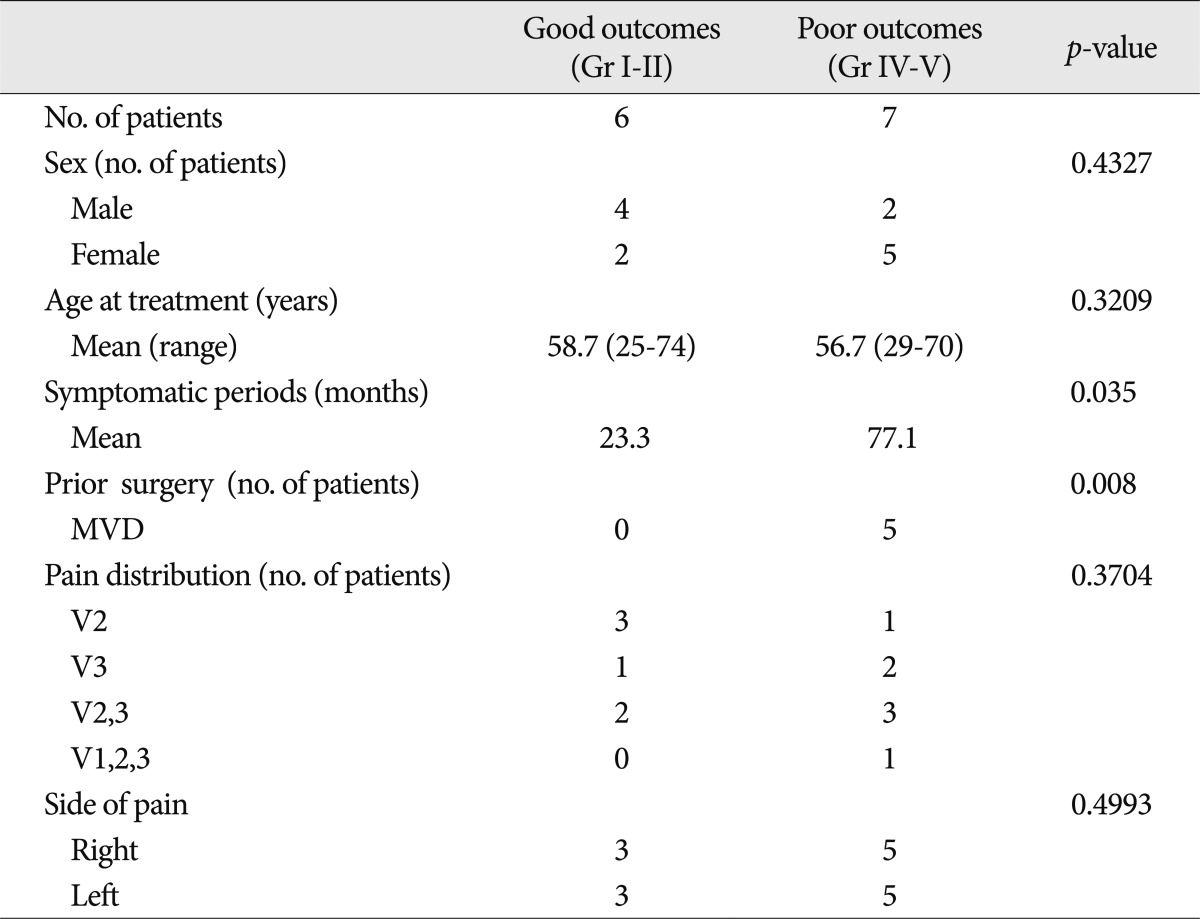
The demographic characteristics of the 22 patients are shown in Table 2. The mean age was 61.5 years (range 25-84 years), and the mean symptom duration from onset to treatment was 46.8 months (range 1-84 months). Six patients were previously treated with MVD. The most common distribution of pain involved the second and third divisions of the trigeminal nerve, observed in a total of 40.9% of patients (9 out of 22 patients). Thirteen patients had right-sided pain, and 9 had left-sided pain.
During the last follow-up period, 6 patients (27.3%) had good treatment outcomes (represented by grades I and II), and 7 patients (31.8%) had poor treatment outcomes (represented by grades IV and V) during a median follow-up period of 92.2 months (range 60-144 months). Of the 6 patients with good outcomes, 4 patients (18.2%) experienced complete pain relief without medication, and 2 (9.1%) had complete pain relief with medications. Of the 7 patients with poor outcomes, 5 patients (22.7%) experienced ≤50% improved pain with medication, and 2 (9.1%) had no pain relief (Table 3).
Subgroup analysis of excellent, good, and poor outcomes found 2 statistically significant factors related to achieving and maintaining complete pain relief : symptomatic periods before treatment (p=0.035) and previous surgery (p=0.008). However, sex, age, pain distribution, and laterality of pain did not correlate with facial pain improvement (Table 4).
Out of a total of 22 patients, 16 patients had been treated with medication only before GKRS (primary group), and 6 had gone through MVD prior to GKRS (secondary group). During the final follow-up period, patients with good outcomes were 37.5% and 0% in the primary and secondary group, respectively; patients with poor outcomes, on the other hand, were 12.5% and 83.3% in the primary and secondary group, respectively (Table 5).
Of the 22 patients, only one patient (4.54%) experienced facial numbness after GKRS, with grade III pain on the pain scale. GKRS was performed in this patient to a maximum dose of 83.6 Gy. This patient experienced full recovery after 12 months. None of the patients had neuropathic pain, dry eye, keratitis, or jaw weakness after GKRS.
DISCUSSION
TN patients in whom medical therapy fails are recommended to undergo several treatment modalities, including MVD, radiofrequency rhizotomy, percutaneous balloon microcompression and GKRS. In general, the most effective surgical treatment is considered to be MVD in healthy patients because it has a demonstrated effective initial pain-free rate and good long-term outcomes. Barker et al.1) reported that the pain-free rate was maintained at 70% of 1185 patients for a median of 6.2 years after MVD. Severe complications that developed include 2 deaths (0.2%) and 16 patients (1%) with ipsilateral hearing loss. Tronnier et al.27) reported that 65% of patients had excellent outcomes at 10 years, and 63% at 20 years after MVD. In this study, the mortality rate was 0.8%, and facial hypesthesia developed in 12.5% of patients. Broggi et al.4) reported that 53-94% of MVD patients were pain-free after a long-term follow-up. They also reported that the mortality of MVD was 0.3% and that cranial nerve dysfunction rates ranged from 0.1-3%. Additionally, radiofrequency rhizotomy also demonstrated an effective long-term outcome for TN patients. Taha et al.26) found that 75% were pain-free at 10 years, and 23% experienced facial dysesthesia. In previous studies, patients who underwent MVD reported long-term pain relief at rates of 62-89%, and patients who underwent radiofrequency reported long-term pain relief at rates of 20-82% for >5 years after achieving a short-term pain relief rate of >90%1,4,5,10,25-28,32). However, severe complications have occurred in TN patients who underwent MVD or radiofrequency rhizotomy at rates of approximately 2-19%1,4,5,10,25-28,32).
In previous reports with long-term follow-up, GKRS for TN patients has long term outcomes slightly inferior to MVD and radiofrequency rhizotomy, but with lower complication rates. Urgosik et al.29) reported that 80% of 107 patients had good outcomes (patients with 60% <residual pain) at a median of 5 years. Little et al.12) reported that 83% of 136 patients had good outcomes (BNI pain score of Class I, II, or III) at a median of 6.3 years. Riesenburger et al.22) reported that 58.5% achieved good outcomes (BNI pain score of Class I, II, or III) at a follow-up period of 48 months. These reports have demonstrated that GKRS is a safe technique for the management of TN, as trigeminal sensory disturbance, the main complication of radiosurgery for TN, only developed in approximately 10% of the patients. In addition, GKRS patients did not develop any of the severe complications which patients that had undergone MVD or radiofrequency rhizotomy experienced14). However, most of the other reports on GKRS and TN combined the longer-term follow-up patients with more recently treated patients, thus making it more difficult to identify long-term results.
In the present study, we strictly evaluated long-term outcomes at a follow-up period of a minimum of 5 years. Thus, our data demonstrate that patients experience lasting pain relief with few complications after GKRS, although patients with good outcomes are fewer than in the previous long-term follow-up studies of outcomes after GKRS. This seems to be due to the fact that only patients with no pain regardless of medication were included in the "good outcome" patient group in our study, whereas published reports on long-term follow-up studies on GKRS included patients with medication-controlled pain in the "good outcome" group. Because pain negatively impacts upon the quality of life of chronic TN patients, we think that the goal of treatment in TN should be complete pain relief. Therefore, we believe it is better to grade patient outcome by the reporting of pain-free outcomes that clearly separates effective pain relief from continued pain. In the current study, patients with pain that had decreased by 50% or more with the use of medication were classified separately as patients with fair outcomes. As a result, our data demonstrated that patients with good and fair outcomes comprise 72.7% of all treated patients, which is a similar outcome to that in previous reports. Therefore, from the results of this 5-year long-term follow-up study, we suggest that the proportion of patients with good outcomes, consisting purely of pain-free patients with or without medication, after GKRS was 27.3%.
Published reports have used radiation dose protocols ranging from 70-100 Gy7,8,21,31). In general, higher doses of radiation are related to better outcomes, but complications, including facial sensory loss and paresthesia, increase at doses greater than 90 Gy19,21).
Generally, maximal radiation doses between 70-90 Gy are used to treat TN. In previous long-term follow-up studies, the mean maximal radiation dose was approximately 80 Gy, and complications included facial numbness, which affected approximately 10% of the treated patients12,22,29). In the present study, the mean maximal dose was 77.7 Gy, which is lower than that utilized in other recent studies; this is partly due to the long follow-up period which started from 1995, and partly because the dose was slightly lowered to avoid the development of lasting complications. In our study, only one patient (4.54%) experienced facial dysesthesia. Thus, we believe that lower radiation doses are associated with lower complication rates.
Several studies have found prognostic factors for short-term outcomes. The presence of previous surgery is regarded as a predictive factor significantly associated with a poor short-term outcome6,13,16,20). However, long-term pain relief factors have not been well studied until recently. Little et al.12) recently reported that at long term follow-up, 75% of patients who were treated with primary GKRS achieved long-term pain relief at 7 years, but only 10% of patients in whom previous surgery had achieved a similar outcome. Similarly, our study found that good outcomes in primary GKRS group (37.5%) was better than in secondary GKRS group (0%), respectively. Also, the presence of previous surgery was observed to be a statistically significant factor related to achieving and maintaining complete pain relief according to our subgroup analysis of good and poor outcomes. Based upon these findings, we have come to believe that there is significant correlation between previous surgery and poor long-term outcomes.
Several limitations of our study are worth mentioning. First, although the pain intensity scale is validated tools for the quantification of pain, they are subjective outcome measures because they are dependent on personal interpretations and variation. Second, the small sample size and retrospective study design limit the power of our outcome observations.
CONCLUSION
GKRS performed at lower radiation doses not only decreased complication rates, but also lessened the development of more severe complications in the long run. However, the long-term results of GKRS for TN are not as satisfactory as those of MVD and other conventional modalities. Although GKRS achieves relatively good outcomes of initial pain relief, our results suggest a steady rate of late failure, particularly among patients who performed secondary GKRS following prior surgery. Proper patient selection is essential in management of TN. GKRS is a safe, effective and minimally invasive treatment modality for only limited group of patients who are not suited to more invasive treatment.